general information
From an anatomical point of view, human lips are musculocutaneous folds surrounding the oral cavity. They consist of the orbicularis muscle, skin and mucous membrane. The upper and lower lips are connected to each other by commissures (commissures) at the corners of the mouth.
Lips are constantly exposed to external and internal factors and act as a platform for the manifestation of various diseases. An indicator of pathological changes in the body is, in particular, a symptom that is simply called “white lips”.
Vinikli nutrition - consult a doctor
To make an appointment for a consultation, call or fill out the return form:
(050) 301-99-26 (067) 446-11-79
Damn,
Your request has been successfully sent!
A call center specialist will contact you as soon as possible to clarify all the details.
In normal condition, the lips stretch without pain, have a pink or light red color, and a smooth surface. White lips in a child or adult are a leading sign of various diseases, to which dryness, swelling, soreness, and cracking may be added.
Lips are an important detail that affects the aesthetic perception of the face and performs many other functions. The lips are involved in the formation of facial expressions; they contain receptors responsible for different types of sensitivity. In addition, they serve as an indicator of a person's health status.
When a pathological process occurs in the body, the lips can change their size, become less elastic, lose sensitivity, become covered in rashes, and turn white. Consulting a dermatologist will help eliminate these manifestations or prevent them.
Iron deficiency anemia in infants and young children
Anemia and anemic syndrome, caused by many causes, can be mentioned among the most common pathological conditions that general pediatricians have to deal with every day. This group includes various diseases and pathological conditions characterized by a decrease in the content of hemoglobin and/or red blood cells per unit volume of blood, leading to disruption of the oxygen supply to tissues. The following laboratory criteria for anemia are applied (N.P. Shabalov, 2003). Depending on the age of the children, the hemoglobin level is:
- 0–1 day of life - < 145 g/l;
- 1–14 days of life - < 130 g/l;
- 14–28 days of life - < 120 g/l;
- 1 month - 6 years - < 110 g/l.
Of all anemias, the most common is iron deficiency (IDA), which accounts for approximately 80% of all anemias. According to the World Health Organization (WHO), more than 500 thousand people worldwide suffer from IDA. The prevalence of IDA in children in Russia and developed European countries is: about 50% in young children; more than 20% - in older children.
IDA is a clinical and hematological syndrome characterized by impaired hemoglobin synthesis as a result of iron deficiency, developing against the background of various pathological (physiological) processes, and manifested by signs of anemia and sideropenia.
Iron is one of the main microelements in the human body. Normally, the adult body contains 3–5 g of iron in bound form. 70% of the total amount of iron is part of hemoproteins. The iron in these compounds is bound to porphyrin. The main representative of this group is hemoglobin (58% iron); Iron is also contained in myoglobin (8%), cytochromes, peroxidases, catalases - up to 4%. Iron is also part of non-heme enzymes (xanthine oxidase, nicotinamide adenine dinucleotide (NADH) dehydrogenase, aconitase, localized in mitochondria); transport form of iron (transferrin, lactoferrin). Iron reserves in the body exist in two forms: in the form of ferritin (up to 70%) and hemosiderin (up to 30%). The peculiarity of iron distribution in young children is that they have a higher iron content in erythroid cells and less iron in muscle tissue.
Iron absorption occurs predominantly in the duodenum and proximal jejunum. The daily diet usually contains about 5–20 mg of iron, and only about 1–2 mg per day is absorbed. The degree of iron absorption depends both on its amount in food consumed and bioavailability, and on the state of the gastrointestinal tract (GIT).
Iron is more easily absorbed in heme (meat products) - 9–22%. Absorption of non-heme iron is determined by diet and gastrointestinal secretion patterns.
Iron absorption is especially active from breast milk, although its content is low - only 1.5 mg per liter; The bioavailability of iron in breast milk is up to 60%. This is facilitated by the special form in which it is presented - in the form of the iron-containing protein lactoferrin. In the lactoferrin molecule, two active binding sites for Fe3+ ions are identified. Lactoferrin is found in breast milk in saturated and unsaturated forms. The ratio of lactoferrin forms varies depending on the lactation period. During the first 1–3 months of life, the saturated iron transport form of lactoferrin predominates. The presence of specific receptors for lactoferrin on the epithelial cells of the intestinal mucosa promotes the adhesion of lactoferrin to them and its more complete utilization. In addition, lactoferrin, by binding excess iron that is not absorbed in the intestine, deprives the opportunistic microflora of the microelement necessary for its life and triggers nonspecific bactericidal mechanisms. It has been established that the bactericidal function of immunoglobulin A is realized only in the presence of lactoferrin.
Physiological losses of iron in urine, sweat, feces, through the skin, hair and nails do not depend on gender and amount to 1-2 mg per day, in women during menstruation - 2-3 mg per day. In children, iron loss is 0.1–0.3 mg per day, increasing to 0.5–1.0 mg per day in adolescents.
The daily requirement of a child's body for iron is 0.5–1.2 mg per day. In young children, due to rapid growth and development, there is an increased need for iron. During this period of life, iron reserves are quickly depleted due to increased consumption from the depot: in premature infants by the 3rd month, in full-term infants by the 5th–6th month of life. To ensure the normal development of a child, the daily diet of a newborn should contain 1.5 mg of iron, and for a child 1–3 years old - at least 10 mg.
Iron deficiency in children leads to an increase in infectious diseases of the respiratory system and gastrointestinal tract. Iron is necessary for the normal functioning of brain structures; if it is insufficient, the child’s neuropsychic development is disrupted. It has been established that in children who had iron deficiency anemia in infancy, at the age of 3–4 years, disturbances in the transmission of nerve impulses from the centers of the brain to the organs of hearing and vision are determined due to impaired myelination and, as a consequence, impaired nerve conduction.
The causes of iron deficiency in children are very diverse. The main cause of IDA in newborns is considered to be the presence of IDA or hidden iron deficiency in the mother during pregnancy. Antenatal causes also include complicated pregnancy, impaired uteroplacental circulation, fetomaternal and fetoplacental bleeding, fetal transfusion syndrome in multiple pregnancies. Intrapartum causes of iron deficiency are: fetoplacental transfusion, premature or late ligation of the umbilical cord, intrapartum bleeding due to traumatic obstetric care or abnormal development of the placenta or umbilical cord. Among the postnatal causes of sideropenic conditions, the first place is taken by insufficient intake of iron from food. In this case, newborns who are bottle-fed with unadapted milk formulas, cow's and goat's milk suffer the most. Other postnatal causes of IDA are: increased body need for iron; iron losses exceeding physiological ones; gastrointestinal diseases, malabsorption syndrome; deficiency of iron stores at birth; anatomical congenital anomalies (Meckel's diverticulum, intestinal polyposis); consumption of foods that inhibit iron absorption.
Premature children and children born with a very large weight, children with a lymphatic-hypoplastic type of constitution are always at risk.
In children of the first year of life, iron deficiency is most often caused by an unbalanced diet, in particular, feeding exclusively with milk, vegetarianism, and insufficient consumption of meat products.
Bleeding of various etiologies can lead to sideropenia. The source of this may be: hiatal hernia, esophageal varices, gastrointestinal ulcers, tumors, diverticula, ulcerative colitis, hemorrhoids, as well as bleeding from the genitourinary tract and respiratory tract. Taking certain medications, such as nonsteroidal anti-inflammatory drugs, salicylates, coumarins, and glucocorticosteroids, can also lead to iron loss. Iron deficiency always accompanies diseases accompanied by impaired intestinal absorption (enteritis, Crohn's disease, parasitic infestations, etc.). Intestinal dysbiosis also interferes with normal digestion of food and thereby reduces the body's ability to absorb iron. In addition, there may be a disruption in iron transport due to insufficient activity and decreased transferrin levels in the body.
It is extremely important to recognize the cause of the development of IDA in each specific case. Focus on nosological diagnosis is necessary, since in most cases, when treating anemia, it is possible to influence the underlying pathological process.
IDA manifests itself with general symptoms. One of the main and visible signs is pallor of the skin, mucous membranes, and conjunctiva of the eyes. Noteworthy are general lethargy, moodiness, tearfulness, easy excitability of children, decreased overall body tone, sweating, lack or decreased appetite, shallow sleep, regurgitation, vomiting after feeding, decreased visual acuity. Changes in the muscular system are detected: the child has difficulty overcoming physical activity, weakness and fatigue are noted. In children of the first year of life, regression of motor skills may be observed.
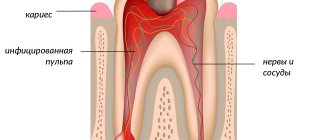
In the second half of life and in children older than one year, signs of damage to epithelial tissue are observed - roughness, dry skin, angular stomatitis, painful cracks in the corners of the mouth, glossitis or atrophy of the oral mucosa, fragility and dullness of hair, hair loss, dullness and brittleness of nails, tooth decay (caries), retardation in physical and psychomotor development.
Depending on the severity of the disease, symptoms of damage to organs and systems are identified: cardiovascular - in the form of a functional heart murmur, tachycardia; nervous system - in the form of headaches, dizziness, fainting, orthostatic collapse. Possible increase in the size of the liver and spleen. From the gastrointestinal tract, there is difficulty swallowing, bloating, diarrhea, constipation, perversion of taste - the desire to eat clay, earth.
The diagnosis of IDA is made based on the clinical picture, laboratory signs of anemia and iron deficiency in the body: hypochromic (color index < 0.85) anemia of varying severity, hypochromia of erythrocytes, decrease in the average hemoglobin concentration in erythrocytes (less than 24 pg), microcytosis and poikilocytosis of erythrocytes (in peripheral blood smear); decrease in the number of sideroblasts in bone marrow aspirate; decrease in iron content in blood serum (<12.5 µmol/l); an increase in the total iron-binding capacity of serum (TIBC) of more than 85 µmol/l (an indicator of “starvation”); an increase in the level of transferrin in the blood serum, with a decrease in its saturation with iron (less than 15%); decreased serum ferritin levels (<15 µg/L).
Treatment of IDA
Treatment of IDA in young children should be comprehensive and based on four principles: normalization of the child’s regimen and nutrition; possible correction of the cause of iron deficiency; prescription of iron supplements; concomitant therapy.
The most important factor in correcting iron deficiency is a balanced diet, and primarily breastfeeding. Breast milk not only contains iron in a highly bioavailable form, but also increases the absorption of iron from other foods consumed at the same time. However, intense metabolic processes in infants lead to the fact that by the 5th–6th month of life, antenatal iron reserves are depleted even in children with a good perinatal history and babies fed with breast milk.
Among other foods, the greatest amount of iron is found in pork liver, beef tongue, veal kidneys, egg yolk, oysters, beans, sesame seeds, seaweed, wheat bran, buckwheat, pistachios, chick peas, peaches, oatmeal, spinach, hazelnuts and etc. (table).
Iron absorption is inhibited by tannins contained in tea, carbonates, oxalates, phosphates, ethylenediaminetetraacetic acid used as a preservative, antacids, and tetracyclines. Ascorbic, citric, succinic and malic acids, fructose, cysteine, sorbitol, nicotinamide enhance iron absorption.
Long walks in the fresh air, normalization of sleep, a favorable psychological climate, prevention of acute respiratory viral infections (ARVI), and limitation of physical activity are necessary. The child's diet should be balanced and include foods rich in iron and substances that enhance its absorption in the intestines. Children suffering from IDA need to be introduced to complementary foods 2–4 weeks earlier than healthy ones. It is advisable to start introducing meat complementary foods at 6 months. You should avoid introducing cereals such as semolina, rice, and bearberry into your child’s diet, giving preference to buckwheat, barley, and millet.
However, these measures are insufficient and do not lead to the cure of IDA, so the basis of therapy is iron supplements. The main ones used orally include: ferric iron compounds - hydroxide-polymaltose complex (iron polymaltose), maltofer, maltofer foul, ferrum lek and iron-protein complex (iron protein succinylate) - ferlatum; divalent iron compounds - actiferrin, ferroplex, tardiferon, hemofer, totema, ferrous fumarate, ferronate.
Therapy should be started with drugs for oral administration and only if they are poorly tolerated (nausea, vomiting, diarrhea), malabsorption syndrome, resection of the small intestine, etc. - iron supplements are prescribed parenterally. When prescribing oral forms, preference should be given to nonionic iron compounds - protein (ferlatum) and hydroxide-polymaltose Fe3+ complexes (maltofer, maltofer foul, ferrum lek). These compounds have a large molecular weight, which makes it difficult for them to diffuse across the intestinal mucosal membrane. They enter the blood from the intestines as a result of active absorption. This explains the impossibility of overdosing on drugs, unlike iron salt compounds, the absorption of which occurs along a concentration gradient. There is no interaction between them and food components and medications, which allows the use of non-ionic iron compounds without disturbing the diet and treatment of concomitant pathologies. Their use significantly reduces the incidence of side effects usually observed when prescribing oral iron supplements (nausea, vomiting, diarrhea, constipation, etc.). In addition, in young children, the dosage form of the drug is of great importance. At this age, it is convenient to use drops and syrups, which also provides the possibility of precise dosing of drugs and does not cause a negative attitude from the child.
When prescribing any iron supplements, it is necessary to calculate the individual need for it for each patient, based on the fact that the optimal daily dose of elemental iron is 4–6 mg/kg. The average daily dose of iron in the treatment of IDA is 5 mg/kg. The use of higher doses does not make sense, since the amount of iron absorption does not increase.
The use of parenteral iron supplements is indicated to quickly achieve an effect in severe anemia; gastrointestinal pathology combined with malabsorption; nonspecific ulcerative colitis; chronic enterocolitis; with severe intolerance to oral forms of drugs. Today in the Russian Federation, only one drug is approved for intravenous administration - venofer (iron sucrose), while ferrum lek can be used for intramuscular administration.
It must be remembered that in young children, iron deficiency is never isolated and is often combined with a deficiency of vitamins C, B12, B6, PP, A, E, folic acid, zinc, copper, etc. This is due to the fact that nutritional deficiency and impaired intestinal absorption, leading to iron deficiency, also affects saturation with these micronutrients. Therefore, it is necessary to include multivitamin preparations in complex therapy for IDA.
The effectiveness of IDA therapy can be judged after 7–10 days by an increase in reticulocytes by 2 times compared to the initial number (the so-called reticulocyte crisis). The increase in hemoglobin is also assessed, which should be 10 g/l or more per week. Accordingly, achievement of the target hemoglobin level is observed on average 3–5 weeks from the start of therapy, depending on the severity of anemia. However, treatment with iron supplements should be carried out in sufficient doses and for a long time (at least 3 months) even after normalization of hemoglobin levels in order to replenish iron reserves in the depot.
If within 3-4 weeks there is no significant improvement in hemoglobin levels, then it is necessary to find out why the treatment was ineffective. Most often we are talking about: an inadequate dose of iron supplement; ongoing or unknown blood loss; the presence of chronic inflammatory diseases or neoplasms; concomitant vitamin B12 deficiency; incorrect diagnosis; helminthic infestation and other parasitic infections.
Contraindications to the use of iron supplements are:
- lack of laboratory confirmation of iron deficiency;
- sideroachrestic anemia;
- hemolytic anemia;
- hemosiderosis and hemochromatosis;
- infection caused by gram-negative flora (enterobacteria, Pseudomonas aeruginosa, Klebsiella).
With the development of severe anemia, accompanied by inhibition of erythropoiesis and a decrease in erythropoietin production, the administration of recombinant human erythropoietin (rhEPO) preparations is indicated. The use of rhEPO is of particular importance in the development of early anemia of prematurity, which develops in the second month of life and occurs, according to various authors, in 20–90% of cases. The administration of rhEPO drugs (Recormon, Eprex, Epocrine) leads to a sharp activation of erythropoiesis and, as a consequence, to a significant increase in iron requirements.
Therefore, the use of rhEPO is an indication for the administration of iron supplements, usually parenteral. Currently, a- and b-epoetins are approved for use in the Russian Federation and are included in the list of additional medicinal products. Prescribing rhEPO allows, in most cases, to avoid blood transfusions, in which there is a high probability of complications (transfusion reactions, sensitization, etc.). The preferred route of administration of rhEPO preparations, especially in early childhood, is subcutaneous. The subcutaneous route of administration is safer and more economical, since smaller doses are required to achieve an effect than with intravenous administration. Until recently, in the countries of the European Union and in the Russian Federation, mainly β-erythropoietins were used for the treatment of hyporegenerative anemia in children, which, when administered subcutaneously, did not cause significant adverse reactions, unlike a-erythropoietins, when administered subcutaneously, there was a high risk of developing red cell aplasia. The most widely used drug among β-erythropoietins is Recormon (F. Hoffmann-La Roche), which is easy to use and leads to a rapid increase in the level of erythrocytes and reticulocytes without affecting leukopoiesis, increases the level of hemoglobin, as well as the rate of incorporation of iron into cells.
Since 2004, European countries have allowed subcutaneous administration of a-erythropoietins, among which in our country the most commonly used are Eprex (Jansen-Silag) and Epocrine (Sotex-GosNII OCHB).
The goal of rhEPO treatment is to achieve hematocrit levels of 30–35% and eliminate the need for blood transfusions. The target hemoglobin concentration values may vary depending on the days and months of the child’s life, but cannot be lower than 100–110 g/l. Depending on the dose, target hemoglobin concentrations and hematocrit are achieved after approximately 8–16 weeks of rhEPO treatment.
To prevent iron deficiency anemia, rhEPO is prescribed to premature newborns born weighing 750–1500 g before the 34th week of pregnancy.
Treatment with erythropoietin should begin as early as possible and continue for 6 weeks. The drug Recormon is administered subcutaneously at a dose of 250 IU/kg 3 times a week. However, it must be taken into account that the younger the child is, the higher doses of erythropoietin he requires, so the dose can be increased.
As mentioned above, rhEPO therapy leads to a sharp increase in iron intake, therefore, in most cases, especially in premature infants, along with an increase in hematocrit, serum ferritin levels decrease. Rapid depletion of iron reserves in the body can lead to IDA. Therefore, all patients receiving rhEPO therapy are prescribed iron supplements. Therapy with iron supplements should continue until serum ferritin levels are normalized (at least 100 mcg/ml) and transferrin saturation (at least 20%). If serum ferritin concentration remains persistently below 100 mcg/ml or there are other signs of iron deficiency, the dose of iron should be increased, including the use of parenteral drugs.
Prevention of IDA in young children includes: antenatal (correct regimen and nutrition of the pregnant woman, timely detection and treatment of anemia in the pregnant woman, preventive administration of iron supplements to women at risk for developing IDA); postnatal (observance of hygienic living conditions for the child, long-term breastfeeding and timely introduction of complementary foods, adequate choice of formula for children on mixed and artificial feeding, prevention of the development of rickets, malnutrition and ARVI in the child). The following people need prophylactic administration of iron supplements:
- women of reproductive age suffering from heavy and prolonged menstrual bleeding;
- regular donors;
- pregnant women, especially repeat pregnancies following a short interval;
- women with iron deficiency during lactation.
Preventive administration of iron supplements is indicated for children at risk for developing IDA:
- premature babies (from 2 months of age);
- children from multiple pregnancies, complicated pregnancies and childbirths;
- large children with high rates of weight gain and height;
- children with constitutional anomalies;
- suffering from atopic diseases;
- those who are artificially fed with unadapted formulas;
- with chronic diseases;
- after blood loss and surgical interventions;
- with malabsorption syndrome.
The dose of iron prescribed for preventive purposes depends on the degree of prematurity of the child:
- for children with birth weight less than 1000 g - 4 mg Fe / kg / day;
- for children with birth weight from 1000 to 1500 g - 3 mg Fe/kg/day;
- for children with birth weight from 1500 to 3000 g - 2 mg Fe/kg/day.
The significance of the problem of IDA in young children is due to its high prevalence in the population and its frequent development in various diseases, which requires constant vigilance among doctors of all specialties. Nevertheless, at the present stage, the doctor’s arsenal has enough diagnostic and therapeutic capabilities for early detection and timely correction of sideropenic conditions.
Literature
- Anemia in children / ed. V. I. Kalinicheva. L.: Medicine, 1983. 360 p.
- Anemia in children: diagnosis and treatment / ed. A. G. Rumyantseva, Yu. N. Tokareva. M., 2000. 128 p.
- Arkadyeva G.V. Diagnosis and treatment of iron deficiency anemia. M., 1999. 59 p.
- Beloshevsky V. A. Iron deficiency in adults, children and pregnant women. Voronezh, 2000. 121 p.
- Borisova I.P., Skobin V.B., Pavlov A.D. Early administration of recombinant erythropoietin in premature infants/7th National Congress “Man and Medicine”. M., 2000. P. 125.
- Vakhrameeva S.N., Denisova S.N. Latent form of iron deficiency anemia in pregnant women and the health status of their children // Russian Bulletin of Perinatology and Pediatrics. 1996. No. 3. pp. 26–29.
- Dvoretsky L. I., Vorobyov P. A. Differential diagnosis and treatment for anemic syndrome. M.: Newdiamed, 1994. 24 p.
- Dvoretsky L.I. Iron deficiency anemia//Russian Medical Journal. 1997. No. 19. pp. 1234–1242.
- Idelson L.I. Hypochromic anemia. M.: Medicine, 1981. 190 p.
- Kazakova L. M., Makrushin I. M. Immunity in iron deficiency // Pediatrics. 1992. No. 10–12. pp. 54–59.
- Kazyukova T.V., Samsygina G.A., Levina A.A. Iron deficiency in children: problems and solutions//Consilium medicum. 2002. pp. 17–19.
- Malakhovsky Yu. E., Manerov F. K., Sarycheva E. G. Mild form of iron deficiency anemia and latent iron deficiency are borderline conditions in children of the first two years of life // Pediatrics. 1988. No. 3. pp. 27–34.
- Papayan A.V., Zhukova L.Yu. Anemia in children: a guide for doctors. St. Petersburg: Peter, 2001. 382 p.
- Prigozhina T. A. Efficacy of recombinant erythropoietin in the complex prevention and treatment of early anemia of prematurity: abstract. dis. ...cand. honey. Sci. M., 2001. 19 p.
- Rumyantsev A. G., Morshchakova E. F. Pavlov A. D. Erythropoietin. Biological properties. Age-related regulation of erythropoiesis. Clinical application. M., 2002. S. 137–144; 266–270.
- Rumyantsev A. G., Morshchakova E. F., Pavlov A. D. Erythropoietin in the diagnosis, prevention and treatment of anemia. M., 2003. 568 p.
- Sergeeva A. I., Sultanova K. F., Levina A. A. et al. Indicators of iron metabolism in pregnant women and young children // Hematology and Transfusiology. 1993. No. 9–10. pp. 30–33.
- Tetyukhina L.N., Kazakova L.M. Prevention of iron deficiency as a measure to reduce morbidity in children // Pediatrics. 1987. No. 4. pp. 72–73.
- Dallman PR, Looker AC, Johnson CL et al. Iron Nutrition in Health and Disease. Eds. Hallberg L., Asp N. G. Libbey; London. 1996; 65–74.
- Messer Y., Escande B. Erytropoietin and iron in the anemia of prematurity. TATM 1999; 15–17.
- Ohls RK The use of erythropoetin in neonatoles//Clin Perinatol. 2000; 20(3):681–696.
- Ulman J. The role of erythropoietin in erythropoiesis regulation in fetuses and newborn infants//Ginekol. Pol. 1996; 67:205–209.
L. A. Anastasevich , Candidate of Medical Sciences A. V. Malkoch , Candidate of Medical Sciences, Russian State Medical University, Moscow
Why are lips white
Human lips, their surface, mucous membrane, and surrounding skin very often display pathological changes that fall within the scope of consideration of several areas of medicine. As a rule, these are deviations that require dermatological, dental, therapeutic care, and the attention of infectious disease doctors.
Only a qualified specialist will be able to determine whether, in your case, white lips are an external sign of illness or a temporary cosmetic problem.
The main reasons why a person’s lips turn white are as follows.
- Manifestation of anemia. The lips and their mucous membranes lose their natural color and turn white due to a decrease in hemoglobin content in the blood. Such changes are observed mainly in iron deficiency or anemia caused by a lack of vitamin B12. The change in color is often accompanied by a deterioration in general health, headaches, burning and painful sensations in the lips, and their dryness.
- Oral candidiasis. More common in young children. It develops when infected with yeast-like fungi of the genus Candida. First, white dotted spots appear on the lips, later they merge and form a continuous film.
- Leukoplakia. A chronic disease accompanied by increased keratinization of the epithelium and inflammation of the mucous membrane. The color of the lesions on the lips can vary, including whitish or white-gray.
- Smoking. Under the influence of nicotine, foci of whitish hyperkeratosis may appear.
- The influence of meteorological conditions (dry air, wind, low temperatures). In such situations, a short-term change in color is observed, followed by restoration of normal tone when the provoking factor is eliminated.
If the natural color of the lips is not restored within several days, they are sore, there are rashes on the surface, or a deterioration in the general condition, you need to consult a doctor - a therapist or a dermatologist. He will study your complaints, conduct anamnestic information collection and a physical examination. If there is a suspicion of a systemic or infectious disease, he will refer a specialist of the appropriate profile for consultation.
How and when can you become infected?
Sources of rotavirus infection can be a sick child or an asymptomatic carrier. The virus is excreted from the body in the stool and gets onto household items, clothing and food with dirty hands.
Doctors often call rotavirus infection a “dirty hands” disease.
A healthy child can introduce the virus into the body first by touching things, and then by touching the face, and also by eating unwashed vegetables and fruits.
Rotavirus outbreaks typically occur in winter, early spring, or late fall because viruses persist in the environment longer at low temperatures. In summer, food poisoning occurs more often - the cause is usually bacterial contamination of food, and bacteria multiply better in the hot season.
White lips in adults and children: diagnosis and treatment
In cases where anamnesis and visual examination of the affected areas of the lips are not enough to make an accurate diagnosis, laboratory and instrumental studies are prescribed. Usually this:
- clinical blood and urine analysis;
- blood chemistry;
- microscopy of lip plaque, histological examination of the selected material;
- Ultrasound, CT, MRI - if necessary, assess the condition of internal organs.
After the diagnosis is made, measures are taken to eliminate the causes of the disease. For some, the doctor will recommend getting rid of bad habits, preventing the adverse effects of the environment, and reviewing their diet in order to saturate it with vitamins and microelements. Others will need drug therapy with systemic and local medications. The choice of medications is carried out taking into account the characteristics of pathological changes in the lips and the nature of the body diseases identified during diagnosis.
What to do to avoid getting sick
Frequent and thorough hand washing with soap is the prevention of any viral and bacterial infections.
- You need to teach your child to do this from an early age: after going outside and going to the toilet, before meals, and just several times a day.
- Parents should wash their hands themselves before touching or feeding the baby.
- It is important to wash vegetables and fruits before eating, observe temperature conditions when preparing food, and drink boiled or bottled water.
The largest amount of virus is excreted in the stool in the first 5 days of illness, so during this period you need to wash your hands more often and wet clean your home.
How to make an appointment with a pediatrician
If the situation has become urgent, then you can dial an ambulance from our clinic, whose phone number is +7 (495) 229-00-03. You can also contact us through our website using the feedback form.
Our medical center staff act as quickly as possible. Especially if we are talking about an emergency situation that requires urgent hospitalization. The clinic carries out diagnostics and immediately prescribes the optimal treatment method that will help your child overcome all the difficulties of the disease as quickly as possible.
How to help the body recover
“Previously, there was an opinion that if you have a rotavirus infection, you should not consume dairy products,” says Elena Kolganova. — Now scientists have revised their opinion on this matter: if a child is breastfed or formula-fed, then nothing needs to be changed. For adult children, it is advisable to remove fresh fruits and vegetables, as they enhance peristalsis and fermentation processes in the intestines.”
If a child has a temperature above 38.5 ºС, you can give him antipyretics, and in case of severe pain - antispasmodics. You should not give painkillers - this will mask the symptoms and it will be difficult for the doctor to make a diagnosis. You should not rinse your child’s stomach - this will increase vomiting and lead to extreme dehydration - loss of consciousness, convulsions.
“Treatment of uncomplicated rotavirus infection is symptomatic: the main thing is to drink plenty of fluids. Vomiting and loose stools usually go away on their own. However, taking probiotics can speed up the recovery process; their administration is safe and quite effective,” says Daria Zakharova.
It is always easier to prevent a disease than to treat it - observe the rules of personal hygiene and teach your children to do the same, wash fruits and vegetables and do not drink tap water.
Appetite and sleep
Parents often pay attention to the most obvious things: for example, appetite and sleep. Does poor appetite indicate anything? Of course, since this is a reflection of the general state of the baby’s nervous system, its balance and comfort.
If a child is, as they say, “skin and bones,” and has bruises under his eyes and often catches colds, you can suspect a tendency to tuberculosis, and in this case you need to see a TB doctor more often. The appetite must correspond to the energy expended by the body, and when the child is inactive and likes to play “quiet games,” it’s okay if he eats a little. If, on the other hand, he runs around all day and comes home “with his tongue hanging out,” you most likely will not have to persuade him to eat properly.
However, if a child eats a lot, regardless of his physical activity, and does not gain weight, this may also indicate a disease, for example, the presence of worms or some kind of psychological problems.
Parents are also worried about the child’s poor sleep. Most often, healthy children do not wake up at night, but may have difficulty falling asleep. Think about how often you neglect your child’s daily routine—whether he goes to bed at a strictly set time, doesn’t watch scary cartoons or action films at night, or spends the evening at the computer. All this excites the child’s nervous system and confuses his biorhythms.
How to help your child
Pediatrician and infectious disease specialist at the GMS clinic Daria Zakharova reminds that the infection in different children can occur in different ways: for some - in the form of mild malaise, decreased appetite with minor abdominal discomfort and a single loose stool, for others - with fever, repeated vomiting and severe diarrhea.
“The parents’ actions largely depend on the severity and age: where to turn for help. If a child feels sick every hour and complains of severe abdominal pain, then you need to call an ambulance, which will take him to the hospital, where the cause of the pain will be determined. In all other cases, you need to call a doctor,” emphasizes Daria Zakharova.
In children over five years of age, the infection is usually milder, so you can help them on your own.
“You need to start with drinking plenty of fluids to replenish the fluid deficit - what the child loses with vomiting and diarrhea,” says Elena Kolganova. There are special formulas for calculation, but usually 50-100 ml of water per kg of body weight per day is required, i.e. if a child weighs 30 kg, then with rotavirus infection he will need from 1.5 to 3 liters of liquid per day. It is better to use a special pharmaceutical solution: for children it should contain a minimum of salt and sugar. You need to give your child water often and little by little - 10-15 times an hour, 2-3 sips.”
Nervous system
Usually parents pay attention to body temperature: normal means everything is fine, high means you need to give aspirin. But even with this everything is not so simple. For example, the temperature rises, and your hands feel like ice. This indicates a spasm of peripheral blood vessels.
If your baby's hands are constantly cold, this is a signal that he has increased excitability of the nervous system. In general, a violation of thermoregulation indicates the vulnerability of the child’s body, the inability of its nervous system to cope with stress. This also applies to such a feature of the child as sweating. Constantly wet palms, constantly wet underwear, even if there were no violent games, are a signal of problems in the nervous regulation of the body.
Other signs also indicate a state close to neurosis - the baby likes to fiddle with something in his hands, bite his nails, often suddenly shudders, talks in his sleep (it’s okay if this happens from time to time, but if it happens every night, it has It makes sense to consult a neurologist).
If a child is constantly nervous, excitable, if it is difficult to captivate him with a game, and once he starts playing, he can no longer stop, forgets himself, reacts aggressively to attempts to intervene, throws prolonged tantrums, then you should not attribute everything to a bad character - perhaps these are symptoms of increased intracranial pressure . It is recommended to show such a child to a neurologist.
Disturbances in the functioning of the thyroid gland can also lead to excessive excitability of the nervous system. In this case, the baby may have a rapid heartbeat. Slightly bulging eyes also indicate excess thyroid hormones. In this case, consultation with an endocrinologist is necessary.
Language
Doctors of the old school began the examination with a request to stick out the tongue as much as possible, even if the stomach or back hurt. The tongue is a mirror of the gastrointestinal tract; all our diseases are “written” on it no worse than on a prescription form.
If there is a constant yellow or white coating on the tongue, this indicates a problem with the functioning of the stomach or intestines. You should also be wary of the so-called “geographical” patterns on the tongue, which are often observed after long-term use of antibiotics or with intestinal dysbiosis, a lack of beneficial bacteria inhabiting it.
What are the dangers of rotavirus without treatment?
Diarrhea and vomiting cause the body to lose a lot of water along with sodium, potassium, magnesium and other electrolytes. This leads to disruption of the lungs - the child begins to breathe frequently and shallowly; the heart and blood vessels - the heart rate increases, blood pressure decreases; and the brain - dizziness, headache, and weakness appear.
In infants, rotavirus infection is most dangerous because convulsions or loss of consciousness can occur as a result of the loss of large amounts of fluid and electrolytes. It is very important to immediately call an ambulance at the first signs of an intestinal infection in infants.
Vaccination against rotavirus
There are two vaccines - the Belgian Rotarix and the Russian RotaTek. Only RotaTek is registered in the Russian Federation. It contains the 5 most common strains. Vaccination against rotavirus infection is not included in the national vaccination schedule, but it can be done at the request of parents. RotaTek has strict age restrictions and intervals between revaccinations - be sure to consult your pediatrician.
“The effectiveness and safety of vaccines against rotavirus infection, subject to age limits, has been confirmed in many studies,” says Elena Kolganova, a pediatrician at the Fantasy children’s clinic. — After receiving the third dose of the vaccine, the number of hospitalizations decreased by 100%, and visits to the clinic decreased by 96%. Rotavirus, unlike influenza, rarely mutates, and therefore vaccination does not need to be carried out every year - immunity lasts up to three years.”