Causes of candidiasis
Thrush in children is caused by yeast-like fungi of the genus Candida, class Fungi Imperfecti. They belong to opportunistic microorganisms, that is, they can provoke disease only if they are directly in the child’s body in sufficient quantities and under favorable conditions. These mushrooms can retain their properties in a dried state for three years, easily tolerate freezing, but when boiled and under the influence of disinfectants they die instantly.
Yeast infection most often occurs in newborns of both sexes, as well as in teenage girls. The main reason infants become infected with candidiasis is infection from a sick mother during the birth process. When a child passes through the birth canal, Candida yeast-like fungi settle on his skin and mucous membranes. In addition, infection can occur while bathing after an infected family member. In teenagers, thrush usually develops due to hormonal changes.
There are a number of factors contributing to the formation of candidiasis in children:
- period of teething;
- long-term and unsystematic use of antibiotics;
- weakened immunity;
- frequent colds;
- endocrine pathology in children (diabetes mellitus, obesity, bronchial asthma);
- diseases of the digestive tract;
- prematurity;
- dry and hot climate in the room where the child is;
- unfavorable sanitary and hygienic conditions.
In recent years, there has been a steady increase in the incidence of diseases caused by opportunistic fungi, among which candidiasis is the most frequently recorded. The increase in the incidence of candidiasis is associated, first of all, with the use of modern therapeutic agents, as well as with environmental changes, in particular, with an increase in background radiation and other factors that weaken the immune system.
Etiology
Candidiasis is caused by yeast-like fungi of the genus Candida
, widespread in nature and classified as opportunistic microorganisms.
of Candida
are registered as causative agents of candidiasis , which are considered pathogenic for humans;
these include C. albicans, C. tropicalis, C. krusei
, etc.
Epidemiology
The causative agents of candidiasis are isolated from the intestines, genitals and bronchial secretions on average in every third person. Primary colonization of the body occurs in the birth canal, and after birth - through contact and nutrition. Infection of a child can occur due to candidiasis of the mother's nipples, from service personnel, through household items, etc. There have been outbreaks of candidiasis in newborns in maternity hospitals. Sexual transmission of candidiasis cannot be ruled out.
Pathogenesis
The main factor in the development of candidiasis is considered to be a background condition or disease of the body, in which opportunistic pathogens acquire pathogenic properties. In recent years, many researchers have come to the conclusion that the main predisposing factor for the occurrence of superficial forms of candidiasis, incl. in HIV infection, is mainly a violation of cellular immunity. A certain role in the development of candidiasis is played by the frequent and not always justified prescription of broad-spectrum antibiotics, incl. for prophylactic purposes, as well as the widespread use of drugs that have an immunosuppressive effect - glucocorticoid hormones and cytostatics. According to Zh.V. Stepanova and L.L. Smolyakova, in children staying in somatic departments of hospitals and receiving antibacterial therapy, damage to the oral mucosa caused by yeast-like fungi is observed in 6.6% of cases, of the oral mucosa and skin - in 15%, of the intestines - in 2.5% , candidiasis in the intestines – in 9.2%.
Candidal paronychia and onychia on the fingers, as a rule, develops in women who have frequent contact with water, while separation of the nail skin (eponychion) from the nail plate is observed, creating favorable conditions for fungal infection in the matrix area. The disease can occur in people suffering from diabetes mellitus, HIV-infected people, who have been receiving antibacterial drugs, corticosteroids, immunosuppressants, etc. for a long time. In recent years, women have begun to use false nails, and therefore another risk factor has emerged for the development of fungal and bacterial infections.
Yeast-like fungi of the genus Candida
can cause damage to the mucous membranes, skin and its appendages, and internal organs. The most common forms of mycosis are superficial.
Clinical picture: Candidiasis of smooth skin
The main localization of the disease is large (inguinal-femoral, intergluteal, under the mammary glands, axillary cavities) and small (interdigital) folds, but rashes can occur on the smooth skin of the trunk and limbs, incl. palms and soles. Outside the folds, foci of candidiasis develop mainly in infants, as well as in adults suffering from diabetes mellitus or severe general illness. In large folds small bubbles, the size of millet grains, and sometimes pustules appear, which open to form erosions. Due to peripheral growth, erosions quickly increase in size and merge, forming large areas of damage. The lesions are dark red in color with a burgundy tint, shiny, with a moist surface, irregular in shape, with a strip of exfoliating epidermis along the periphery. Fresh small erosions (screenings) form around large foci. In children, especially weakened ones, from the folds the lesion spreads to the skin of the thighs, buttocks, abdomen, and sometimes to the entire skin. There may be painful cracks deep in the folds. Candidiasis of smooth skin outside the folds (chest, abdomen, shoulders, forearms, legs, etc.) in children has a clinical picture of seborrheic dermatitis; in adults, the disease can manifest itself in the form of erythematous spots with peeling in the center and small blisters along the periphery. Candidiasis of smooth skin of small folds (interdigital erosion) most often occurs between the 3rd and 4th, 4th and 5th fingers of the hands, less often of the feet, and is characterized by the formation of eroded foci of a rich red color with a smooth, shiny, as if varnished surface, clear boundaries, with flaking of the horny layer of the epidermis along the periphery. The disease can begin with the appearance of small blisters on the lateral touching hyperemic surfaces of the skin, then spreads to the area of the interdigital fold, swelling, maceration, and peeling appear. Interdigital candidal erosion is observed mainly in individuals who have prolonged contact with water, which contributes to the development of skin maceration; in addition, favorable conditions are created for the development of candidal infection. In addition to the third and fourth folds, others may be affected, not only on one, but also on both hands. Patients are concerned about itching, burning, and if there are cracks, pain. The course of the disease is chronic, with frequent relapses. Candidiasis of the smooth skin of the nipples in nursing women deserves attention. Its clinical manifestations can be different: slight hyperemia in the area of the isola; lesion near the nipple with maceration, clear boundaries; fissure with maceration along the periphery and small bubbles between the nipple and the isola.
Candidiasis of the palms and soles is rare. On the palms, the disease can occur as dry lamellar dyshidrosis (superficial lamellar, ring-shaped or garland-shaped peeling), vesicular-pustular form (vesicles and pustules against the background of hyperemic and edematous skin) and hyperkeratotic eczema (against the background of diffuse hyperkeratosis or individual areas of keratinized skin are observed sharply limited wide skin grooves with a dirty brown color). Candidiasis of the skin of the soles occurs mainly in children and is characterized by the presence of small blisters and pustules, hyperemic spots with peeling and exfoliating macerated epidermis along the periphery.
Candidiasis of the nail folds and nails (candidal paronychia and onychia)
The disease begins from the posterior ridge, most often in the area of its transition to the lateral ridge, with the appearance of hyperemia, swelling and swelling of the skin. Then the inflammatory phenomena spread to the entire roller, which becomes thicker and seems to hang over the nail, and peeling is observed along the edge of the roller. The skin of the roller becomes thin, shiny, and the nail skin (eponychion) disappears. When the roller is pressed, ichor, a lump of white crumbly mass, or a drop of pus may be released (due to the addition of a secondary infection). Later, the nail plate changes: it becomes dull, in the area of the lunula it is separated from the bed, destroyed as onycholysis, or transverse grooves and elevations appear on it. These changes are associated with impaired blood supply in the matrix area, i.e. they are trophic in nature and are caused by inflammation in the area of the cushion. When the fungus penetrates the nail plate, and this happens from the lateral edges, the nails become thinner, separate from the bed, acquire a yellow-brown color and look as if they are trimmed on the sides. In young children, inflammatory phenomena in the area of the cushion are more pronounced, and the nail plate changes from the distal edge. There is candidiasis of the nails without inflammation of the ridge. In this case, the change in the plate begins from the distal edge and develops according to the type of onycholysis; the plate becomes thinner, does not adhere to the bed, and there may be multiple lesions of the nails.
Diagnosis and differential diagnosis
In superficial forms of candidiasis, the diagnosis is based on the presence of a characteristic clinical picture in the patient and identification of the fungus in pathological material (skin flakes, scrapings from nails) during microscopic examination. The diagnosis can be considered reliable if pseudomycelium or true mycelium and budding cells are detected. Sowing on a nutrient medium is carried out to identify the type of yeast-like fungus of the genus Candida
. Isolating only a culture of the fungus has no diagnostic value, since it can be obtained by culturing scrapings from the skin and nails of healthy people.
With candidiasis of smooth skin of large folds and outside the folds, the disease should be differentiated from seborrheic eczema, psoriasis, and other mycoses - inguinal athlete's foot, superficial trichophytosis, pseudomycosis erythrasma (complicated form); with interdigital candidal erosion on the hands - from dyshidrotic eczema, on the feet - from mycosis caused by Trichophyton interdigitale
and
Trichophyton rubrum
; when nails and ridges are affected - from onychia and paronychia of bacterial etiology, eczema and psoriasis.
Treatment
Considering that candidiasis is an opportunistic mycosis, first of all, it is necessary to identify and, if possible, eliminate the pathogenetic factors of the disease (study of the immune and endocrine status, gastrointestinal tract and corrective therapy). Limited and sometimes widespread forms of smooth skin lesions, especially those that developed during treatment with antibacterial drugs, as a rule, are easily treated with local antifungal agents and can resolve without treatment after discontinuation of antibiotics. Local and systemic antimycotics are prescribed as etiotropic therapy. In recent years, azole drugs with a broad spectrum of action, as well as polyene antibiotics, have been widely used in the treatment of candidiasis.
For candidiasis of large folds of smooth skin with acute inflammatory phenomena, treatment should begin with the use of an aqueous solution of brilliant green (1-2%) in combination with an indifferent powder and continue for 2-3 days, then antimycotic drugs should be prescribed until the clinical manifestations resolve.
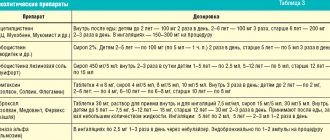
For candidiasis of large, small folds and other areas of smooth skin, antifungal agents are used in the form of cream, ointment and solution: ketoconazole, clotrimazole, oxyconazole, bifonazole, natamycin. The cream or ointment is applied in a thin layer to the lesions and rubbed in 1-2 times a day, the duration of treatment is until the clinical manifestations resolve, then it is recommended to continue using the cream for another 7-10 days to prevent relapse. In case of widespread processes on the skin and the ineffectiveness of local therapy, systemic antimycotics are prescribed: fluconazole - for adults at a dose of 100-200 mg, for children at a dose of 5 mg/kg body weight; itraconazole - adults at a dose of 100-200 mg; nizoral - adults at a dose of 200 mg 1 time per day daily, as well as the polyene antibiotic natamycin (adults 100 mg 4 times a day, children 50 mg 2-4 times a day). The duration of therapy is 2-4 weeks.
For candidiasis of the nail folds and nails, anti-inflammatory treatment of the fold is first carried out using applications of pure ichthyol, which are done once a day until the inflammatory phenomena subside. Then apply antimycotic agents (ketoconazole, oxiconazole, isoconazole, clotrinazole, etc.) for topical use, rubbing them under and around the roller. The procedures are carried out 2 times a day, in the evening the drugs can be used under an occlusive dressing. It is possible to combine an ointment (cream) with a solution, alternating them. If the nail plate is involved in the process, you can not remove it or clean off the infected areas after softening with keratolytic agents (bifonazole in the nail treatment kit), and then treat the nail bed with antifungals for external use. Therapy is carried out until clinical manifestations resolve and a healthy nail plate grows. If it is ineffective, systemic antimycotics are prescribed: fluconazole according to an intermittent regimen (adults 150 mg once a week, children 5-7 mg/kg body weight); itraconazole (adults) using the pulse therapy method (200 mg 2 times a day for 7 days, then a 3-week break) for 2-3 months; nizoral (adults) 200 mg per day daily for 2-4 months.
Prevention
- To prevent the development of candida infection in children who are in somatic departments of hospitals and receiving antibacterial drugs, they need to be prescribed fluconazole at a rate of 3-5 mg/kg body weight once a day. The daily dose depends on the degree of risk, treatment is carried out during the main therapy.
- Patients with candidiasis in the intestines are prescribed nystatin 2-4 ml IU per day or natamycin 50 mg for children and 100 mg for adults 2 times a day for 15 days.
- Prevention of the development of candidiasis in patients with severe somatic and endocrine diseases, as well as with immunodeficiency (multiple mycological studies).
- Prevention of dysbiosis.
- Prevention of the development of candidiasis in newborns.
Types of candidiasis
In children, the following main types of thrush are distinguished:
- candidiasis of the skin and its appendages;
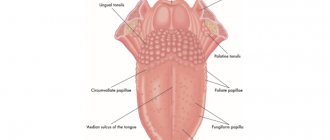
- candidiasis of the mucous membranes (oral cavity, corners of the mouth, tongue, pharynx, larynx, trachea, gastrointestinal tract, genitals, urethra);
- visceral or systemic candidiasis (yeast endocarditis, meningitis, sepsis, etc.).
Depending on the duration of the inflammatory process and the manifestations of the disease, acute and chronic forms of thrush are distinguished. Depending on the extent of the lesions, candidiasis can be focal or generalized. Based on the depth of spread, thrush is divided into visceral and superficial (smooth skin, mucous membranes, and nails are affected).
A separate type of disease includes secondary allergic rashes that appear as a result of additional sensitization of the skin to the proteolytic enzymes of the fungal pathogen.
Candidiasis of interdigital skin folds
Candidiasis of the interdigital folds is often an occupational disease and occurs in people employed in production using Candida spp. for industrial purposes, or those where there is a high probability of contamination by them (confectionery, canning, processing of vegetables and fruits, etc.), as well as for women who do a lot of housework without protective gloves, nurses.
Hand skin candidiasis
More often, the folds between the third and fourth fingers of the hands and the lateral surfaces of these fingers are affected, where the skin is macerated, whitish in color, and is easily torn off, exposing an eroded shiny surface.
Symptoms of candidiasis
The clinical symptoms of candidiasis vary due to the different localization of the inflammatory process in the body.
Oral thrush in children is characterized by:
- A whitish, cheesy coating in the mouth that is easily removed with a finger or a spatula. It is localized mainly on the mucous membrane of the cheeks, tongue, tonsils, hard and soft palate, red border of the lips. At first, candidal plaque is present in the form of small white dots, reminiscent of semolina, then merges into larger plaques with the characteristic appearance of “curd residue” or milky films in the mouth. In the absence of proper treatment and when the process becomes chronic, plaque transforms into a dense yellow film, which is difficult to separate from the mucous membranes with the formation of bleeding erosions.
- Hyperemia of the mucous membrane (overflow of blood vessels), erosion.
- Pain and burning in the mouth.
- Seizures, maceration of the skin in the corners of the mouth.
- Child's moodiness, loss of appetite up to complete refusal to eat.
Genital candidiasis is characterized by the following symptoms:
- Redness and swelling of the genitals, severe itching.
- A cheesy, thick discharge from the genitals with an unpleasant sour odor.
- Pain during urination.
- White milky films on the skin of the external genitalia, in the chronic process - congestive hyperemia, tissue thickening.
Candidiasis of the esophagus , stomach and intestines is characterized by the presence of the following symptoms:
- Colic and flatulence, frequent regurgitation.
- Pain when swallowing.
- Pain in the stomach and intestines.
- Decreased appetite, refusal to eat.
- Unshaped stool with an admixture of white inclusions, reminiscent of curd mass.
Skin candidiasis is characterized by the formation of a rash in the form of papules or vesicles, which eventually open and form weeping erosions with a white coating. In infants, the elements of the rash are most often localized in the area of large folds on the abdomen. In older children, yeast infections usually appear between the fingers.
How to get rid of candidiasis in a child
To get rid of candidiasis, you need to strengthen your immune system.
Based on the results of the analysis, if the specified bacteria exceed the norm, the doctor will prescribe the necessary medications.
The very first and most important task is to bring the intestinal microflora to a normal state and normalize the functioning of the digestive system. It is also necessary to strengthen the immune system.
In addition, it is necessary to conduct additional research for the presence of various abnormalities that may cause the appearance of this disease. The form of treatment will directly depend on the results identified. Typically, treatment of this disease has the following goals:
- Correct treatment of the disease. Based on the results of the study, medications will be prescribed.
- General strengthening therapy. This type of infection begins to manifest itself when immunity is low and there is an insufficient amount of nutrients in the body.
- Based on this, taking various vitamins is also necessary.
Thematic video will tell you about candidiasis:
https://www.youtube.com/watch?v=2M7sely6ph8
Diagnosis of candidiasis
The first step in diagnosing thrush is an examination by a pediatrician. If the doctor detects signs of fungal infection (white cheesy coating on inflamed mucous membranes, the appearance of eroded surfaces after removing the milk film), a set of additional laboratory and instrumental studies is prescribed to confirm the diagnosis of candidiasis and determine the cause of its appearance:
- General blood and urine analysis.
- Blood chemistry.
- Microbiological examination of stool.
- Serological study.
- Microscopy of a scraping or smear from the affected organ to determine the presence of Candida fungus.
- Cultural culture of blood, urine, feces, biopsy of the mucous membrane.
- Ultrasound examination of the abdominal and pelvic organs.
- Endoscopy of the digestive organs.
Treatment methods for candidiasis
Therapy for yeast infections in children involves an integrated approach to treatment. Pediatricians are faced with the task of not only destroying the fungus that causes lesions, but also eliminating pathogenetic mechanisms, restoring normal microflora and increasing immunological reactivity.
When choosing tactics for drug treatment of thrush in children, they try to refrain from prescribing antibiotics. Affected mucous membranes and skin are usually treated with antifungal creams, ointments and solutions. For the visceral form of candidiasis, systemic antifungal drugs are used.
During treatment, the patient needs a healthy diet, in which proteins predominate and carbohydrates are limited. In addition, as prescribed by your doctor, you need to take vitamins, anti-dysbacteriosis medications and immunostimulating drugs.
Since children’s immunity is still quite weak, it is necessary to take a responsible approach to the prevention of thrush and follow simple rules:
- regularly sterilize all pacifiers and pacifiers given to the child;
- bathe in clean water in an individual bath;
- carefully care for the skin and mucous membranes;
- observe the correct diet, monitor the state of the child’s gastrointestinal tract;
- completely cure candidal colpitis and vulvitis before or during pregnancy, so as not to infect the child during childbirth.
Consequences of candidiasis
If a timely diagnosis is made and rational treatment is prescribed, thrush in children is completely cured and leaves no consequences. With improper therapy and late seeking medical help, the disease can become chronic and become resistant to further treatment measures. In addition, against the background of a chronic yeast infection, candidosepsis can develop, a dangerous disease that can be fatal. Intestinal candidiasis is fraught with complications such as heavy bleeding, perforation of the intestinal wall, and ulcers.