The upward trend in the birth rate of children with congenital facial malformations is not decreasing. One of the first places in their structure is occupied by the cleft of the upper lip and palate. According to WHO, the worldwide incidence of births of children with congenital cleft lip and palate (CCLP) is 0.6-1.6 cases per 1000 newborns. This developmental defect is accompanied by anatomical and functional disorders, the severity of which depends on the degree of clefting and the age of the child.
VRVGiN is a fundamental factor in the development of mixed breathing, and also causes the reflux of food into the nasal cavity during feeding [1]. This congenital defect creates favorable conditions for secondary infection of the ENT organs. ENT pathology ranks second in children with varicose veins after maxillofacial disorders [2, 3].
There is a small number of studies stating more frequent cases of diagnosis of acute sinusitis, rhinitis, tonsillitis and other ENT diseases in children with varicose veins compared to healthy children [1-3].
A few foreign publications are devoted mainly to the condition of the paranasal sinuses in children with varicose veins. In these works, the authors compared the volume of the sinuses on the healthy side and on the cleft side and the timing of their pneumatization in comparison with similar sinuses of healthy children. It was found that the development of the maxillary sinuses in children with varicose veins does not lag behind the development of the sinuses of healthy children [4-6].
There is insufficient data on the prevalence of inflammatory pathology of the paranasal sinuses in this group of children, the causes and predisposing factors; examination algorithms have not been developed to prevent the onset of the disease or identify it in the early stages, which would reduce the treatment time and increase its effectiveness.
The purpose of the study was to assess the condition of the paranasal sinuses and structures of the nasal cavity in children with varicose veins.
Introduction
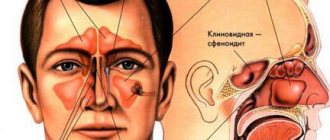
The maxillary sinus (MSS) is a pyramidal-shaped cavity in the upper jaw, lined with single-layer multirow ciliated epithelium.
Of course, it plays a role in improving nasal breathing, but, contrary to popular belief, according to HL Sieron et al., it is not involved in the movement of inhaled air [1]. In addition, a significant immune function of the sinus in the production of nitrogen monoxide (NO) has been proven. It plays an important role in protecting the orbit and brain in the event of a facial skull fracture, as well as in reducing the mass of the skull. The immune function of the sinus is performed in the case of adequate functioning of mucociliary transport. The functioning of the ciliated epithelium may be disrupted due to congenital disorders, entry of a foreign object into the sinus cavity and further development of the inflammatory process, dysfunction of the natural anastomosis and the formation of a vicious circle, the presence of a neoplasm, etc. The VChP is not involved in the circulation of inhaled air, so the appearance of its cavity of various dense inclusions located under the mucous membrane often does not manifest itself with clinical symptoms. Thus, after sinus lift surgery, most patients do not notice changes in nasal breathing, and osteomas of the maxillary sinus are often an accidental finding.
The sinus lift operation (or alveolar ridge augmentation) is performed on patients with insufficient alveolar ridge height for the installation of dental implants in the area of the molars and/or premolars of the upper jaw. The operation is performed by creating a trapezoidal mucoperiosteal flap in the area of the upper arch of the vestibule, forming a bone “window” in the area of the lateral part of the upper jaw. Through the “window”, the mucous membrane of the sinus bottom is peeled off from the jaw bone in the projection of the planned dental implantation. Bone material is introduced into the resulting space, the “window” is closed with a collagen membrane, the flap is placed in place, and the wound is tightly sutured [2]. As a result of surgical treatment, additional volume of the alveolar process is created by reducing the volume of the upper jaw.
According to various authors, delayed complications in the area of alveolar process augmentation in the form of sinusitis occur extremely rarely [3]. Inflammatory complications most often relate to early postoperative complications. Patients with a history of chronic rhinosinusitis, as well as thick mucous membrane of the upper jaw, are most at risk for intra- and postoperative complications.
Osteoma of the upper jaw is a rare pathology. The incidence of osteomas of the maxillary sinus among all osteomas of the paranasal sinuses is only 2% [4], among all tumors of this area - 5% [5]. Osteoma is a benign tumor originating from bone tissue. The tumor may have a predominant compact or spongy component, or they may be of a mixed nature. A feature of osteoma is uncontrolled but slow growth. Asymptomatic course of the disease is the most common option. Clinical manifestations occur after a long period of time after the start of growth of pathological tissue, when the tumor reaches a certain size and acquires a special location in relation to nearby organs and structures. Osteomas are characterized by extensive growth and are usually located on a wide or narrow base growing from unchanged bone tissue. The wide base of osteoma is not an unambiguous sign of its malignancy.
The disease can be diagnosed using radiation methods. Osteoma can be recognized on planar images, such as teleradiography in various projections, orthopantomography, and even targeted images. The techniques only allow one to see the pathological process, but do not give an idea of the extent of the spread of the tumor, its location in relation to neighboring cavities and structures. The most complete picture of the topography of sinus osteoma is provided by computed tomography - cone beam CT (CBCT) and multislice CT (MSCT). The advantage of MSCT is the ability to assess the density characteristics of a bone tumor in Hounsfield units. In addition, when using CT data in a surgical navigation station, MSCT will create less “noise” than CBCT, which will significantly increase the accuracy of intraoperative navigation [6].
Fibrous dysplasia has radiological manifestations similar to osteomas of the upper jaw. A distinctive feature of fibrous dysplasia is its repetition of the contour of the bone involved in the pathological process [7]. The growth of osteoma is usually extensive, not following the contours of anatomical structures.
Like any tumor, osteoma of the upper jaw is subject to mandatory surgical removal, primarily to obtain a morphological result. Due to the active development of endoscopic technologies these days, it has become possible to excise osteoma of the maxillary sinus using an endoscopic transnasal approach. Depending on the location of the tumor, the following approaches to the sinus are used: through the lower nasal passage, through the area of the natural anastomosis, and a combination of approaches. In case of extensive growth of the bone tumor, severe clinical manifestations and the absence of endoscopic equipment in the clinic, it is possible to use access through the anterior wall of the upper quadrant. The combination of transnasal and transoral approaches is also used in practical sinus surgery. Navigation equipment makes it possible to determine the tumor resection boundary as accurately as possible intraoperatively.
Navigation stations make it possible to visualize the tip of the navigated instrument in the lumen of the sinus as accurately as possible (according to some authors, the error is 0.6 mm [8]). The device uses electromagnetic or infrared radiation to compare the location of the instrument tip and the preoperative CBCT or MSCT data loaded into the system. In addition, some navigators allow the use of navigable drills. It must be remembered that intraoperative changes occur only in the surgical field; in the CT image in the navigator, the structures remain intact. The use of this equipment is possible only in the hands of an experienced surgeon who perfectly knows the anatomy of the maxillary sinus and is proficient in the endoscopic technique of its surgical treatment.
When does perforation of the maxillary sinus floor occur?
In ordinary life, perforation is impossible; it always becomes a complication of any dental manipulations with the upper teeth. Perforations occur during root removal, during installation of implants, and during the treatment of pulpitis. At the same time, a gross violation of treatment tactics by the doctor, as well as the special structure of the skull and the anatomy of the teeth can become a source of trouble for a person.
For example, the risk for the patient increases many times if preliminary radiography reveals too small a distance between the apex of the tooth root and the bottom of the maxillary sinus.
There is also danger if the doctor tries too hard to expand the root canals or fills them with excessive compaction. The filling material, transforming, is able to go beyond the apex of the tubule; subsequently, the sinus is perforated in almost one hundred percent of registered cases.
A breakthrough can also occur when installing a pin or inserting an implant. In the latter cases, it is always the dentist's mistake. Such an accident significantly complicates further procedures when performing prosthetics. The jaw bones of patients who have lost their teeth long ago and applied late for implantation are extremely vulnerable. If a tooth is removed, the processes of tissue degeneration accelerate. The doctor must take this feature into account when determining the size of the pin and performing pre-implantation preparation.
Perforation also occurs during root resection if the dentist did not bother to carefully study the patient’s examination data in advance and does not know the size of the bone plate that separates the maxillary sinus and the inflamed cyst on the tooth. Inaccurate movement and perforation occurs. It can also be caused by surgery to remove a significant amount of jaw bone.
Clinical observation
Patient K., 39 years old, consulted an otorhinolaryngologist with complaints of discomfort in the projection of the left upper quadrant and recurrent left-sided sinusitis over the past 5 years. According to CBCT data, a formation of bone density with a heterogeneous structure, approximately 5 × 11.5 mm in size, is determined in the left upper jaw (Fig. 1A).
On examination, the face is symmetrical, without pathological rashes. Breathing through the nose is free, there is no free discharge from the nose. The mucous membrane of the nasal cavity is pale pink. Palpation in the projection of the left upper quadrant is painless.
The patient underwent surgical treatment
. Under conditions of general anesthesia, under the control of an electromagnetic navigation station and endoscopes of 0, 30, 45, 70 degrees, access to the left upper nasal sinus was performed through the lower nasal meatus. The sinus cavity is visualized. In the area of the alveolar sinus bay, the formation of bone density was visualized. Using curved diamond burs, the tumor was reduced to the base. Fragments of the formation were sent for histological examination. The operating window is closed. Lateralization of the inferior turbinate was performed. Anterior nasal tamponade with hemostatic tampons. Blood loss is minimal.
In order to prevent possible postoperative infectious and inflammatory complications, irrigation of the nasal cavity with saline solutions and the use of MestaMidin-nos nasal drops were consistently performed. This drug has a good antiseptic effect against, including multi-resistant microorganisms [9]. In addition, the product promotes faster regeneration of the nasal mucosa [10]. Places Midin-nose is easy to use, so the patient can independently perform treatment of the nasal cavity. Antibacterial therapy was not required in the postoperative period.
7 days after surgery, patient K underwent a follow-up CBCT scan (Fig. 1B, C). According to the study: surgical access in the area of the lower nasal meatus is visualized; there are no signs of a formation in the lumen of the left upper nasal passage.
The result of histological examination: intertwined bone beams and connective tissue. The formation is represented by mixed osteoma (Fig. 2).
The patient has been observed on an outpatient basis for 2 years since surgical treatment. There are no signs of osteoma growth or maxillary sinusitis.
Treatment of perforation of the maxillary sinus
Non-surgical intervention is possible only in the case of instantly detected perforation, when it is diagnosed during the procedure of tooth extraction or treatment of pulpitis. The doctor immediately sends the patient for an x-ray and, based on the results, determines whether an infection of the maxillary sinus has developed.
For example, a cavity wall was perforated during tooth extraction. The dentist noticed the defect immediately. In this case, the doctor makes efforts to preserve the blood clot in the hole where the tooth was previously located. The therapy involves the application of tampons with iodine, and the tampon is tightly fixed in the formed depression and is not removed from there during treatment - so as not to disturb the clot that seals the wound. It usually takes up to a week for the breakout to granulate and disappear.
The option of fixing a plastic barrier separating the axillary cavity from the oral cavity is allowed. This plate is held on adjacent teeth with special clasps. Meanwhile, the perforation heals on its own.
If it was not possible to avoid the penetration of foreign bodies into the maxillary sinus or the infection began to spread, the sinus will need to be opened and cleaned. The resulting wound is closed plastically.
conclusions
The most objective way to diagnose dense space-occupying formations of the upper jaw is computed tomography (CBCT or MSCT).
If signs of osteoma are detected in the cavity of the upper jaw, the patient must be recommended to undergo surgical excision of the formation. Morphological verification of the removed material is mandatory.
The combination of an endoscopic transnasal approach and navigation equipment in the removal of osteomas of the upper jaw is the most modern and optimal option for treating the pathology.
MestaMidin-nos has proven itself in local therapy as a means to prevent possible postoperative infectious and inflammatory complications. The use of MestaMidin-nos allows you to avoid a course of systemic antibacterial therapy.
The publication was carried out with the support of Solopharm in accordance with internal policy and current legislation of the Russian Federation.
Patients and methods
We analyzed the results of 114 RCT and 10 MRI patients with odontogenic maxillary sinusitis. The X-ray CT study took place in the computed tomography department of the Kursk Regional Clinical Hospital (KOKB) using X-ray computed tomographs (USA) NXI and VCT models in axial and coronal projections. MRI examination - on tomographs of the SIGNA PROFILE 0.2 T and SIGNA OVATION 0.35 T models in axial, sagittal and coronal projections. Measurements were made using the RadiAnt DICOM Viewer diagnostic image viewing program using line and ellipse tools.
Old perforations
It happens that the patient does not go to the clinic after treatment due to accidental perforation. At first the pain is sharp and pronounced, but gradually its character changes and the sensations smooth out. A fistulous tract is formed between the affected sinus and the outer part of the gum. Everything that happens is accompanied by the development of symptoms of typical sinusitis: pain from the perforated intramaxillary cavity, constant nasal congestion, outflow of pus from the nasal passages (and sometimes the fistula on the gum begins to fester). Some patients complain of swelling of the cheek on the side where the sinus is damaged.
If after treatment a person develops strange sensations, as if he feels the movement of air through the gums when sneezing, coughing, and drunk liquid enters the nose, there is a direct indication of an old perforation of the maxillary sinus.
Unfortunately, non-invasive techniques will not help here. An operation is required to remove foreign matter and foci of infection from the sinus. The fistula is cut out, and the opened defect is repaired. After the procedure, a course of antibiotics is prescribed with accompanying physiotherapeutic treatment and the use of drugs that reduce the risk of allergic reactions.
How to treat sinus inflammation in adults and children?
Sinusitis, sinusitis and other inflammatory processes have similar symptoms. Treatment in adults will be effective if a specialist makes an accurate diagnosis and selects the optimal complex therapy, which will include:
- special medicines;
- healing procedures;
- prevention.
It is important not only to relieve the symptoms of the disease, but also to eliminate the causes of the disease. And they can be different. Some people have a weakened immune system, while others should have their body examined or give up bad habits and an unhealthy lifestyle.
In children, treatment of sinusitis, sinusitis and other inflammatory processes of the nasal sinuses also includes a whole range of measures:
- it is important to see a doctor quickly to make a diagnosis and avoid complications;
- you need to strictly adhere to the recommendations of specialists and monitor the child’s condition;
- It will be necessary to prevent inflammation in order to maintain the health of the child’s sinuses.
In the fight against serious inflammatory processes, one must not hesitate. For example, sinusitis can lead to inflammation in the skull or meninges. Acute catarrhal sinusitis develops in 70% of children who regularly suffer from ARVI. Odontogenic sinusitis develops in those who have dental problems.
Consequences of perforation
The patient should not expect that the perforation will heal on its own; such a wound should not be perceived superficially. Attempts at self-treatment with folk remedies or opening a fistula at home are prohibited. The consequences of careless intervention look ominous:
- Loss of healthy teeth in close proximity to the perforation site;
- Penetration of infection into other intracranial cavities;
- Development of abscesses and phlegmons with extremely serious health consequences;
- The risk of developing meningitis or meningoencephalitis due to the proximity of the brain to the inflamed lesions inside the maxillary sinus. With each act of sneezing, being under great pressure, the pathological flora scatters inside the cavities and is able to penetrate into areas from where it is easy to affect the meninges. All this can lead to death.
Therapy of old perforations overgrown with fistula tracts is usually complex and time-consuming. Relapses with new breakthroughs from the sinus to the gum surface are common. Fistulas are not at all harmless formations; they are not easy to cure.