Severe periodontitis
At this stage, the treatment of periodontitis is no longer limited to conservative measures; here it is necessary to resort to surgical methods of treatment - removal of the most damaged teeth, open curettage, and flap operations.
In addition, in case of severe periodontitis, targeted regeneration (building) of bone tissue is used with the help of osteogenic preparations, membranes, etc., which strengthen and compact the bone and create the prerequisites for its restoration where possible.
Causes of periodontitis.
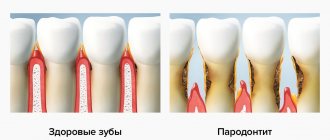
Inflammatory processes, known as periodontitis and gingivitis, occur in periodontal tissues and are interrelated forms of the same disease. Their main difference is in localization. Pathologically, the process can be inflammatory or dystrophic in nature.
Gingivitis (early stage of periodontitis) is an inflammation of the gums (the process affects only the tissues of the gingival margin, while affecting only the upper gum tissues) without compromising the integrity of the periodontal junction.
Risk factors: tobacco smoking; poor oral hygiene; acute lack of vitamins and minerals; problematic fillings; nasal breathing disorder.
Main symptoms: redness and swelling of the gums; the appearance of soft and hard deposits on teeth; bleeding gums when brushing teeth; weakened immunity.
As for periodontitis, it affects all periodontal structures. It is characterized by chronic inflammation of the gums and destructive changes - destruction of the periodontium and bone tissue of the alveolar process. The dentogingival attachment is disrupted, periodontal pockets are formed and, in the future (with an active course), due to the rapid destruction of the alveolar processes, teeth fall out.
The rate of spread of periodontitis is greater, the more numerous the risk factors are: immunosuppressive conditions; there are deviations in the development of the dental system (occlusion pathology); any diseases of internal organs have been diagnosed.
Classification and symptoms of generalized periodontitis
If you take into account the depth of the pockets and the severity of bone tissue destruction, the doctor can diagnose three forms of manifestation of the disease. They differ in symptoms and signs.
Mild periodontitis
This stage is characterized by a slight sensation of itching and burning. Bleeding periodically occurs during brushing your teeth and after eating (hard foods - meat, fresh fruits and vegetables). The depth of periodontal pockets reaches 3.5 mm, and a decrease in gum tissue is observed at approximately 1/3 of the height of the root. Pathology may not manifest itself for a long time. Therefore, at the first stage of the disease, patients are in no hurry to contact doctors, which provokes the transition of the disease to more severe forms.
Average degree of periodontitis
During its course, various pathological changes occur in the patient. In particular, the functions of the dental system change. The pocket reaches a depth of 5 mm, the teeth become mobile and slightly loose. Gaps appear between them. The tissue structure of the hole is reduced by half the root. There may be an unpleasant odor coming from your mouth.
Severe periodontitis
This disease is typical for adult patients. The depth of the periodontal pockets exceeds 5 mm, the loss in tissue is more than ½ the length of the tooth root. The gums are subject to severe inflammation and bleed. They come out with purulent discharge. Not only tissue elements are destroyed, but also bone parts. Sometimes the walls between the teeth completely dissolve, leading to severe tooth mobility. In this case, it is almost impossible to preserve them in their natural form.
The more advanced the disease, the more difficult it is to cope with it and choose adequate treatment. And the chances of a full recovery decrease with each step of its progression.
Classification of periodontitis.
The course of the disease, area of distribution and severity - these are the classification criteria.
According to the course of periodontitis there are:
- Spicy;
- Chronic;
- Periodontitis with abscess formation.
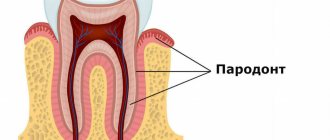
Periodontitis in the area of distribution can be local (focal) - individual parts of the periodontium are affected, and generalized (diffuse) - diffuse damage to the periodontal complex. The pathological process involves all periodontal tissues of one tooth, a group or all teeth: gums, circular ligament of the tooth, periodontal tissue, bone tissue (compact and spongy substance), the vascular system of these formations and the dental pulp.
According to its manifestation, periodontitis can be mild, moderate and severe.
The most important clinical sign of periodontitis is the presence of a periodontal pocket of varying depth (this can be used to judge the degree of damage).
The stronger the inflammation, the greater the pathological mobility of teeth becomes. As a rule, mobility is accompanied by the appearance of gaps between teeth and the overlap of one tooth over another. When determining the severity of periodontitis, the specialist evaluates the position of each tooth in the dental arch.
The degree of periodontal atrophy and the functional value of teeth underlie the choice of treatment for periodontitis.
Reasons for the development of generalized periodontitis
The precursors to the formation of the disease are some exogenous and endogenous factors. The first group is small; most of the diseases of this system are provoked precisely by the internal state of the body. All etiological factors are classified into local (plaque, tartar, problems with bite, abnormal position of teeth, strands of the mucous membrane) and general (diseases of the body - diabetes mellitus, goiter of toxic origin, excess weight, hypovitaminosis, hepatitis, gastritis, etc. ). All this one way or another affects the condition of the periodontium and leads to a deterioration in its functioning.
Microbiological studies have been able to prove the fact that the leading role in the development of this condition is given to microorganisms called Prevotella Intermedia, Bacteroides forsythus, Peptostreptococcus, etc. In order for the dental system to be protected from their influence, protection in the form of plaque is provided in the dental plaque , accumulated in the gingival sulcus, periodontal pockets, and tooth roots.
The life products of pathogenic organisms contribute to the activation of the secretion of certain substances (prostaglandins, cytokines, enzymes), which lead to the destruction of periodontal tissue structures. Factors that entail a decrease in local and general protection from the influence of pathogenic bacteria include:
- smoking,
- radiation damage,
- ignoring the rules of personal hygiene regarding the oral cavity.
The development of this condition is usually preceded by inflammation of the gingival margin, which entails disruption of the connection, destruction of the ligamentous apparatus, and resorption of the alveolar bone. These changes lead to pathological mobility of teeth, overload of their individual groups, and occlusion. In the absence of adequate therapy, this disease provokes tooth loss or removal, as well as problems with the functioning of the jaw system as a whole.
Treatment of periodontitis.
Removal of dental plaque and professional teeth cleaning in combination with medications (massages, lotions and rinses) - this is the treatment at the initial stage of periodontitis.
More severe periodontitis requires surgical intervention (to remove deep deposits of tartar, specialists perform curettage, bone tissue augmentation, splinting, implantation) and drug treatment. Anti-inflammatory and antiseptic drugs are used (they are also injected into periodontal pockets). There are non-steroidal anti-inflammatory drugs in the form of gels and pastes, which greatly facilitates their administration; in addition, tissue regeneration stimulants are often used, which are applied topically. In the complex therapy of periodontitis, vitamins are prescribed that strengthen the vascular walls.
Rational treatment and systematic hygienic oral care can achieve remission.
In the treatment of periodontitis, physiotherapy is successfully used: electrophoresis with painkillers and vitamin preparations, laser radiation, fluctuarization (therapeutic currents of medium frequency), darsonvalization (pulse currents). The latest modern methods of treating periodontitis, such as ultrasound and laser beams, are also widely used in dental practice. The laser beam painlessly removes tissue affected by inflammation and closes not too deep periodontal pockets. Ultrasound is an excellent way to get rid of pathogenic microflora accumulated in gum pockets.
It is strictly necessary to visit a doctor for consultation; he will determine the symptoms and prescribe treatment for periodontitis. Preventing periodontitis and regularly visiting the dentist is the best way to maintain oral health.
Directions of therapy for mild periodontitis
The chronic form of mild periodontitis is treated in stages, here is an approximate diagram.
- First, plaque and deposits formed on the tooth enamel are removed.
- Subsequently, the doctor prescribes topical antibacterial agents. They need to be applied in the form of applications to the affected areas. An important role is played by rinsing the mouth with solutions containing antiseptic components.
- The key to successful therapy is compliance with hygiene procedures (purchase and use of special healing pastes, professional toothbrushes, dental floss).
By providing thorough daily oral care and learning to visit the dentist regularly, you can avoid this sore and prevent worsening if it progresses.
Treatment methods for generalized severe periodontitis
Chronic periodontitis, the course of which has moved to the last, most dangerous stage, requires not only careful conservative therapy, but also surgical intervention. Indeed, at this stage, tissue destruction is pronounced, and conventional antibiotics are not enough. You will need to undergo a number of procedures aimed at restoring the affected areas and replacing teeth. Depending on the overall picture, the following types of surgical interventions are prescribed:
- removal of teeth with a high degree of mobility;
- vertical dissection of the gum wall in order to scrape tissue that has undergone pathological changes;
- horizontal excision of the pocket wall together with the affected gum (if the depth of the periodontal pockets is more than 4 mm);
- flap surgery (coronal displacement, lateral, therapy, transplantation, etc.);
- abscess incisions;
- plastic surgery in the frenulum of the tongue, lips.
An important role in the treatment of this form of the disease is played by the use of anti-inflammatory drugs, vitamin compounds, and drugs that strengthen immune function. The prognosis of the disease at this stage is unfavorable, since exacerbation does not entail remission and lasts almost constantly. In addition to tooth loss and gum decay, there is the possibility of systemic complications.
What to do to avoid complications
To avoid complications, it is necessary to recognize the disease in the early stages and take measures for adequate treatment. All this will allow you to achieve stable and long-term remission and preserve the functions of your teeth and gums. In order for the dental system to be healthy, it is necessary not only to observe the rules of personal hygiene, carrying out regular care procedures, but also to periodically visit a specialist who will perform professional cleaning in order to remove minor dental deposits.
General symptoms of the disease
In the initial stages, the patient suffers from severe bleeding gums. They become loose and swollen. The patient feels itching, throbbing, severe burning, pain when he chews food. An unpleasant odor begins to emanate from the mouth. Dental pockets at this stage are shallow, they are located mainly in the interdental spaces. At the initial stages, the teeth are motionless and not displaced anywhere. The patient's general condition is normal.
The clinical picture of the developing disease is somewhat different. In addition to the above symptoms, the patient may experience:
- displacement of teeth and their loosening;
- high sensitivity of teeth to external irritants (temperature fluctuations);
- problems chewing food;
- disturbance of general well-being (typical of severe forms of pathology), accompanied by weakness, malaise, and increased body temperature;
- an increase in the size of regional lymph nodes, which in addition become painful;
- during a dental examination, the doctor observes signs of diffuse gingivitis;
- Plaque and deposits accumulate abundantly on the teeth;
- tooth loss, fistula, abscesses (signs are characteristic of advanced stages of the disease).
In the case of a chronic form of the disease, the gums have a pale pink tint. There are no dental deposits, manifestations of pus or blood. There is a possibility of exposure of the roots of the teeth. X-ray does not show signs of bone resorption.
Chronic generalized periodontitis: from pathogenesis to treatment
L. M. Tsepov
Doctor of Medicine, Professor, Head of the Department of Therapeutic Dentistry, Smolensk State Medical Academy, Roszdrav
N. A. Goleva
Assistant at the Department of Therapeutic Dentistry of the State Educational Institution of Higher Professional Education "Smolensk State Medical Academy" of Roszdrav
M. M. Nesterova
Assistant at the Department of Therapeutic Dentistry of the State Educational Institution of Higher Professional Education "Smolensk State Medical Academy" of Roszdrav
“Clinicians are trained by their profession to perceive the disease as a given, to assess the compliance of the observed syndrome with a known standard, and to identify the presence of diagnostic criteria. The search for the source of the disease often fades into the background. This has become the main reason for the predominance of a syndromic approach to treatment, refined diagnosis and even classification of diseases” (p. 61) [27].
According to WHO data [29], the prevalence of periodontal diseases in people aged 35-44 years worldwide is 94.3%. Periodontal diseases are a diverse group of predominantly inflammatory
diseases accompanied by the destruction of tissues of the periodontal complex, including the collagen base of the periodontium and the bones of the alveolar process [49]. Some authors [16, 28] believe that chronic generalized periodontitis (CGP), despite the sufficient monomorphism of the main clinical manifestations, is an etiologically and pathogenetically heterogeneous disease, and this may determine the features of treatment tactics.
Oral microflora is a vital necessity, but its development should not lead to the emergence and development of a clinically obvious disease [55]. In the oral cavity, there is normally a balanced ratio of microorganisms (more than 400 species) and protective factors of the macroorganism, and only a violation of this balance leads to the development of a pathological process in the periodontium [41, 42, 52]. “Bacteriological etiology” of inflammatory periodontal diseases was initiated by the works of some foreign authors [51, 56] and is still supported by domestic researchers [25]. It should be noted that some authors [32] more cautiously assess the role of microflora, pointing only to “the leading group of microorganisms involved in
in the inflammatory process (pathogenesis! - L. Ts. et al.) in diseases of periodontal tissues” (p. 73). The fact of the presence of periodontal pathogens in healthy periodontal tissue indicates rather more in favor of a multifactorial model of the etiopathogenesis of periodontal diseases [14, 54]. Therefore, the absolute role of “dental” plaque in the development of inflammatory periodontal diseases should be questioned [47]. The presence of bacteria is a necessary, but not the only condition for the occurrence of periodontitis [5]. It is possible that the leading role in the genesis of periodontitis in different countries may belong to different types of microbes [43]. The role of each periodontal pathogen and their interaction in the development and course of inflammatory periodontal diseases remains controversial [12].
It has been established [17] that the composition of the microflora of periodontal pockets (PC) is polymicrobial (aerobic-anaerobic-fungal associations) in nature and it is almost impossible to predict the most likely “pathogens” of periodontal inflammation. According to some authors, this is the presence of highly virulent subgingival pathogens (mainly Act. bacillus actinomycetemcomitans and Campilobacter rectus), capable of bypassing intermediate protective mechanisms, activating and producing substances that contribute to the destruction of the epithelium and collagen of the dentogingival attachment (this is pathogenesis!
). Another path of tissue damage to the periodontal complex is associated with the activation of macrophages, monocytes, fibroblasts, interacting with intermediate systems and humoral factors (kinin, immune), involved in inflammatory-destructive reactions and leading to the steady, progressive destruction of the connective tissue structure of the periodontium and increased resorptive effect in the bone tissue [23]. Ultimately, the cause of the pathology will lie in the property of the organism, and not in the factor that in a particular case acts as the “causative agent” of the pathology [2].
Despite the fact that the etiology of CGP is still unclear, there is no doubt that in the development of CGP (that is, in the pathogenesis
of this disease), genetic, infectious, immunobiological, environmental and other factors play an important role. Genetic and non-genetic factors influence each other, and their effects are not always clearly distinguishable [5]. The role of the central nervous system, psychoemotional state and psychovegetative disorders is not denied [31], which gives the authors grounds to assert the connection between the stress reaction and CGP. Lipid peroxidation is directly related to the pathogenesis of periodontitis. The combination of 4-5 provoking factors indicates their extreme variability in the development of CGP.
In the light of modern concepts, CGP is considered as a multifactorial disease, thereby emphasizing the absence of a specific etiological factor [6, 29, 37]. The emergence and development of inflammatory-destructive periodontal disease are determined not only by the cumulative effect of various periodontal pathogens, but also by the “assistance”/counteraction to them by the tissues, organs and systems of the body. Features of the structure and functions of the periodontium are apparently the key to understanding the multicomponent, “multi-story,” complex, systemic pathogenesis of CGP [35, 40, 41].
The pathogenetic basis of periodontal damage with its generalized nature at the level of tissue metabolism (disturbed as a result of genetic predisposition), according to some authors, is: a shift in the acid-base balance; increased metabolic acidosis; destruction of the proteoglycan matrix [3].
On the exposed and initially rough surface of the cementum of the tooth root, as a result of a pathological process that began with tissue damage in the gingival sulcus area by periodontopathogenic agents, a so-called dental plaque is formed. Within 4-8 hours, the first foci of mineralization appear on the inner surface of the microbial biofilm, and by the 14th day a full-fledged “tartar” is formed [11]. Gram-negative anaerobic or facultative anaerobic bacteria located in the biofilm and associated with the subgingival surface cause and maintain an inflammatory reaction in the periodontium with the subsequent production of large amounts of cytotoxins.
Loss of attachment is one of the most important signs of the active phase of periodontitis. It is indicated [8] that during a clinical examination using probing, it is almost impossible to judge whether a periodontal pocket has formed or not, since the only criterion for such a conclusion may be a morphological assessment of the condition of the dental-gingival junction, which is inaccessible to clinical methods. The morphofunctional substrate of the PC is: deepening the space between the tooth root and the gum; destruction of the periodontal junction; formation of granulation tissue in the bottom and wall of the PC with strands of epithelium vegetating in it. The result of pathogenetic processes is the progressive destruction of tissues of the periodontal complex. Progressive
periodontal damage is a destructive process in periodontal tissues, occurring unevenly, with periods of exacerbation and chronicity. In this case, the interdental bone tissue is affected earlier and more often than on the buccal, lingual or interradicular side. There is a constant loss of collagen under the sulcular epithelium with simultaneous fibrosis of the connective tissue of the gums, the absence of fibroblasts, and an extensive inflammatory and immunological reaction of the tissue. The sulcular epithelium, proliferating and moving in the apical direction, turns into the epithelium of the PC, which is formed under the influence of periodontopathogenic factors. Deep periodontal pockets usually serve as biological markers of the pathological process in the periodontium. In the phase of progressive inflammation, collagen tissue elements are destroyed and active bone resorption occurs [11]. In this case, granulation tissue at the bottom of the periodontal pocket plays a crucial role as a destructive factor that determines the nature and structure of pathogenetic changes in CGP [7]. Supragingival and subgingival “calculus” is considered as an attempt by the body to inactivate periodontal pathogenic bacteria through mineralization [36].
The main paradox in pathogenesis
periodontitis is the absence of differences in the clinical picture associated with alteration of periodontal tissues and fundamentally different mechanisms of this alteration, which are determined by the type of human reactivity [19].
What should a dentist do when establishing the fact of chronic inflammation (which can be infectious, immune, autoimmune, etc.). How can he determine the nature of inflammation in an outpatient setting? What about prescribing treatment?
Pathological changes that occur in the gums and can lead to periodontal destruction (i.e., periodontitis) require the expansion of pathogenetic therapy and gingivitis
, and periodontitis [7], since the experience of the past century has shown that neither prevention nor etiotropic therapy has led to a radical solution to the problems of “classical” infectious pathology. Pathogenetic therapy is based on knowledge of the mechanisms of disease development. Some authors [9] try to pathogenetically substantiate, for example, the use of the antibiotics clindamycin and amoxiclav in the treatment of periodontitis. At the same time, there are concerns that antibacterial drugs (antibiotics and antiseptics) used for inflammatory periodontal diseases can cause pronounced dysbiotic disorders in numerous environmental niches. After the “destruction” of some bacteria, the free niche is quickly filled with others. Unfortunately, so far the principle of comprehensive individualized treatment for each patient, even those suffering from gingivitis, remains largely declarative, which is associated not only with organizational and financial problems, but also with the lack of objective tests to assess the functional state of periodontal tissues before, during and after treatment.
No one questions the need for complex therapy
CGP. According to some authors [44], less than half of the data in the “Medical records...” of such patients contains a record of the need for treatment or consultation with any specialist other than a dental therapist. Unfortunately, the complexity of treatment is interpreted differently and carried out in an arbitrary order, without clear planning and control of effectiveness, due to the lack of methods for such planning and effectiveness criteria [4].
The negative impact of both removable and fixed dentures on the marginal periodontium was noted in 64% of cases. This effect (“prosthetic” periodontitis) is caused not only by the direct impact of prostheses, but also by medical manipulations throughout all stages of orthopedic treatment (tooth preparation, gum retraction, taking impressions, etc.) [33, 34; opening certificate, reg. No. 440 dated February 12, 2008, diploma No. 350].
In this regard, the main goal of therapy for actively ongoing CGP is not “destruction of its pathogens,” but the elimination of negative consequences
effects of periodontal pathogens on periodontal tissue.
Various methods of antibacterial therapy
make sense only when performing microbiological diagnostics to correct the treatment of the disease in a particular patient [48]. Moreover, the effectiveness of antimicrobial therapy for inflammatory periodontal diseases in each individual patient significantly depends on the individual qualitative and quantitative composition of the oral microflora and the severity of individual protective factors [22].
When using both manual and automated curettage
high efficiency of mechanical treatment of tooth root surfaces is achieved only if there is appropriate motivation of the patient and sufficient practical experience of the doctor [53].
The main disadvantage of resorbable membranes
is their relatively early loss of barrier function [50]. If the membrane loses its barrier function too early, active growth of epithelial cells begins, and the regeneration of connective tissue stops.
Positive results in the treatment of CGP can be obtained after the use of surgical methods (curettage, flap surgery) and additional corrective therapy with metabolic
actions [21].
Despite the obvious successes in studying the etiology and pathogenesis of CGP, we must admit that tangible success in treatment cannot be achieved. The effectiveness of orthopedic and surgical treatment methods, including dental implantation, is significantly reduced due to complications of a purulent-inflammatory nature [18]. In dental practice, there is a growing belief in the need to include orthopedic methods
into complex therapy of CGP [24]. Unfortunately, in everyday practice, prosthetics is neither the initial nor the final stage of complex therapy for periodontal diseases, especially in adolescents and young people [1], although it is well known that orthopedic treatment as a component of complex therapy for CGP is aimed at immobilizing teeth, eliminating functional overload, stabilization of dentition.
With age, in the structure of inflammatory periodontal diseases, the proportion of periodontitis that occurs with greater intensity increases, especially in men [15]. Treatment prognosis
CGP becomes unfavorable when: the patient’s age is more than 45 years, the duration of the disease is more than 10 years, the periodontal Russell index is more than 5, the depth of periodontal pockets is more than 4 mm, and the persistence of the inflammatory infiltrate in the gums. Unfortunately, the late stages of CGP are characterized by a decompensated nature of the process [13].
The presented data give reason to believe that periodontology in our country has come a long way from private semiotics to oriented pathogenetic treatment. At the same time, it should be recognized that scientific and experimental research on pathogenesis and treatment in periodontology remains relevant. We can agree with the opinion of some authors [20] that more work is needed on the diagnosis, treatment and prevention of especially early stages of periodontal diseases.
Substantiation of the pathogenetic aspects of the relationship between periodontal diseases and systemic pathology will make it possible to create new algorithms for the approach to diagnosis and treatment, which will help improve not only dental, but also general human health, as well as the quality of life of the population [45]. The introduction of complex treatment and preventive programs into clinical dental practice can not only effectively inhibit the progression of inflammatory periodontal diseases, but also significantly improve the condition of the periodontium [26].
Thus, the treatment of CGP is too complex a combination of preventive, therapeutic and rehabilitation interventions to currently be able to talk about any benchmarks or standards. Most likely, this is a complex of the most necessary medical manipulations, carried out at the earliest possible stage of the development of the disease in certain combinations and sequences and, of course, with the persistent efforts of the doctor to penetrate into the root cause of the disease, without missing the slightest detail that could affect the effectiveness of therapy of this multifactorial disease [38]. Optimally, a patient suffering from CGP should be treated by a periodontist. Only the “old” multidisciplinary approach with the coordinating role of the periodontist will prevent the progression of the disease, thereby avoiding negative consequences [39]. The fullest effect of treatment can be obtained only at an early stage of the disease [10]. In any situation with periodontal pathology, an indicator of the effectiveness of treatment is the interruption of the progressive loss of supporting tooth structures, their reparation as a result of etiotropic and pathogenetic therapy, specific for each nosological form of periodontal disease. A successful outcome of treatment can be considered the regeneration of the periodontal structure, amounting to more than 50% of the original volume of the periodontal defect, elimination of pathological mobility and restoration of tooth function [46].