4137
It is still believed that the best implants for bone surgery are autogenous (taken from the patient himself) bone. However, due to its limited nature and pronounced resorption, this material still cannot be considered ideal.
A good alternative is bone substitutes obtained from animal bones. The Bio Oss biomaterial produced by Geistlich Pharma, intended for use in dentistry, contains all the main advantages of bone substitutes.
General overview
Bio Oss is obtained from cattle bones. The material has several dosage forms, allowing you to choose the optimal method of delivery to the surgical wound:
- Granules packaged in bottles (Bio-Oss Spongiosa). Universal form, suitable for any type of operation.
- Granules in a syringe (Bio-Oss Pen). Thanks to the specially shaped tip, Bio-Oss Pen is especially convenient in cases where the operating area is in a hard-to-reach place.
- Blocks (Bio-Oss Block). Used when filling significant defects is required.
- Combined preparation Bio-Oss Collagen, 90% consisting of Bio-Oss granules, 10% porcine collagen. Thanks to the latter, it has increased adhesive, manipulation and regenerative properties.
Geistlich Pharma also produces Geistlich Bio-Gide Membrane, an auxiliary material used to create a barrier between the bone and the sinus. The use of Bio-Gide accelerates tissue regeneration and wound healing.
Geistlich Bio-Oss is recommended for use in all types of bone grafting - in dental surgery, implantology, periodontology, and maxillofacial surgery.
In terms of its regenerating and healing properties, it is not only comparable to autogenous bone grafts, but in individual components it is superior to them.
Besides:
- Bio-Oss can be used alone or in combination with autogenous bone.
- Bone substitute effectively stabilizes the blood clot, preventing alveolar bleeding.
- High hydrophilicity, caused by the presence of many micro- and macropores, promotes uniform and rapid impregnation of the material with saline solution and the patient’s blood.
- Stability and preservation of the volume of the resulting bone tissue is a winning point from the point of view of ensuring the aesthetics of facial tissue.
- The multiplicity of forms and good handling characteristics make it possible to use Bio-Oss in a wide variety of clinical cases, including complex ones.
The technique for using Bio-Oss depends on the clinical situation and the dosage form used. The following points are common:
- Soaking the material with saline solution or the patient’s blood.
- It is supplied to the operation area and distributed over the defect.
- Closure of the surgical wound with a flap of the patient's soft tissue, followed by suturing and/or application of a Bio-Gide membrane.
Let’s find out together how long the temperature lasts after dental implantation, and in what cases the help of specialists is needed.
Come here if you are interested in the benefits of dental implants.
At this address https://www.vash-dentist.ru/implantatsiya/metodiki/o-prieme-antibiotikov-posle-zubov.html we will tell you why antibiotics are prescribed after dental implantation.
Main advantages
Bio oss bone material has been successfully used by leading dentists for many years, in particular, by specialists at the A-Medic clinic. Its advantages include:
- blood clot stabilization;
- slow resorption of granules (it makes it possible to maintain the volume of the augmentation over a long period of time);
- high hydrophilicity. It is ensured by a unique system of macro and micro pores, which guarantee uniform saturation of the granules with blood;
- osteoconductive properties. They are a guarantee of reliable regeneration. The granules are integrated into the formed bone and become its frame;
- guarantee of soft tissue aesthetics. This is due to the formation of a high-quality base of hard tissue.
Indications and contraindications
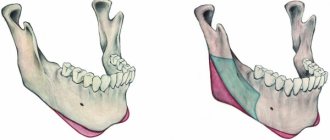
In orthopedics, Bio Oss is recommended for use in all cases where it is necessary to maintain or increase the volume of the bone of the alveolar process or jaw:
- Filling the hole after tooth extraction to maintain the normal volume of bone tissue if implantation is planned in the future.
- Bone augmentation , performed simultaneously with tooth implantation to fill the gaps between the bone and the implant.
- Filling fenestrations and dehiscences (discrepancies and holes) in the bone after implant placement.
- Sinus lift.
- Filling cavities in the bone tissue of the jaw or alveoli formed as a result of cystectomy.
Due to the affinity of Bio Oss with human bone tissue, the biomaterial has virtually no contraindications. The only limitation is that it cannot be used to fill infected wounds.
Why are biomaterials needed for immediate implantation?
If we are talking exclusively about tooth extraction and implant installation, then, frankly speaking, most often they are not needed. Especially when you consider which teeth most often have to be implanted immediately:
The picture shows that immediate implantation in an aesthetically significant area is not carried out as often as it might seem at first glance. It’s just easier to film it - that’s why all specialized sites are filled with work in the area of the frontal group of teeth, but there are very few cases of immediate implantation in the lateral part of the dentition.
However, immediate implantation in the lateral part of the dentition is carried out much more often than in an aesthetically significant area. And, most often, it is not necessary to use any materials to augment the socket when installing an implant - in most cases, the structural features and blood supply of the alveolar bone in these areas make it possible to avoid significant atrophy.
In the photographs shown, it is noticeable how the linear dimensions of the alveolar ridge have changed from the moment of removal of 26 and installation of the implant, until its integration (compare the thickness). But this is not so critical, and allows you to get a good prosthetic result:
However, if one of the goals of implantological treatment is the maximum preservation of the tissues surrounding the tooth, then it is unlikely to be possible to do without the use of biomaterials. In the photo below: it seems that immediate implantation was carried out, but subsequent atrophy of the alveolar ridge completely ruined the aesthetic result of the treatment.
Not only the frontal group of teeth requires attention from an aesthetic point of view - some patients want the tooth in the lateral area to be indistinguishable from the real one. And in these cases, we also use biomaterials to keep the bone walls of the socket in place and obtain a good aesthetic and functional result:
Considering that the implant (with rare exceptions) is always smaller than the extracted tooth, we need to fill the space vacated by the tooth with something in order to keep the tissues surrounding the hole in place. Otherwise, subsequent atrophy may negate the aesthetic results of implant treatment:
Agree, it’s not very pleasant when the implant begins to show through... and no crown, even the coolest one, can compensate for this.
So, to prevent this from happening, we need biomaterials and grafts, in particular. By filling the space between the implant and the alveolar wall, we keep the latter in its place, preventing changes in the linear dimensions of the alveolar ridge in the implant area. Of course, some degree of atrophy is still present, but it is much less pronounced and almost unnoticeable than in those cases if we did nothing.
Physico-chemical characteristics
Animal bones consist of 25% organic matter (collagen), 65% inorganic matter (calcium phosphate) and 10% water.
Organic matter other than collagen is present in small quantities - lipids, polysaccharides, proteins. In addition to calcium, there are ions of some other elements.
During the production of Bio-Oss, the organic component is removed from raw materials (cattle bones). All that remains is the mineral base (calcium phosphate), abundantly permeated with microcapillaries and microtunnels.
In its morphology, chemical composition and ultrastructure, Bio-Oss is very close to human bone, which determines the patient’s body’s positive reaction to it. Compared to other natural materials that have larger crystals, Bio-Oss integrates very well with native bone .
The topography of their surface is important for implanted biomaterials. Smooth materials integrate less well than rough ones. Bio-Oss has a pronounced rough surface , which promotes active adhesion and proliferation of osteoblasts and rapid matrix synthesis.
The area of the internal surfaces of the implant material is no less important. The larger it is, the more intensely the blood vessels grow into it, the more active and faster the integration and healing of wounds takes place. Histomorphometric studies carried out on 12 samples of bone materials showed that the internal surface of Geistlich Bio-Oss is about 80 m2/g, which is approximately 5 times greater than that of the other samples studied.
Safety
Biomaterial obtained from cattle bones may contain prions, special infectious agents that can cause dangerous diseases in animals and humans. The first have “mad cow disease” (TSE, spongiform encephalopathy).
People are at risk of getting Creutzfeldt-Jakob syndrome, kuru and some other types of infections.
The safety of the Bio Oss biomaterial is ensured by two factors - the high quality of raw materials and processing technology, which involves multi-stage cleaning and sterilization.
When choosing raw materials, the country of origin is taken into account in terms of the effectiveness of veterinary control and precautionary measures taken against “mad cow disease”.
Geistlich Pharma purchases bone raw materials for Bio-Oss in the USA, where veterinary control is very effective. So far, not a single case of spongiform encephalopathy has been recorded.
To further guarantee safety, raw materials are obtained only from 3 slaughterhouses under constant USDA supervision.
The second factor ensuring the safety of the material is the multi-stage purification of raw materials aimed at inactivating prions. The bones are exposed to temperature for at least 15 hours.
Additionally, chemical purification of raw materials with alkaline compounds and treatment with gamma irradiation are carried out. This technology guarantees the complete safety of the biomaterial.
results
Recently, my colleague Andrey Karneev posted on Facebook a photo of one work at the final stages of prosthetics:
I'm proud to have taken part in it too.
It all started with inflammation, fistula and tooth extraction:
Then, we prepare the hole and check the positioning of the implant:
Then we augment the hole. It is very convenient to use implant analogues for Bio-Oss Collagen packaging:
Installing the XiVE implant (Dentsply Implants):
Immediately on the implant - temporary crown:
which three months later, by the time the implant is integrated, looks completely different:
Well... by the time the permanent crown is installed, we have retained the natural contour of the adjacent gum.
Which, in fact, is what we needed to do.
Biological properties
Osteoplastic materials are divided into three groups:
- osteoinductive , directly affecting the formation and growth of bone tissue;
- osteoconductive - play the role of a bone frame on which new bone tissue is formed;
- osteoneutral , acting as a bone filler.
Bio Oss belongs to osteoconductive biomaterials, i.e. it functions as a scaffold on which new bone tissue is formed and differentiated.
The high osteoconductive properties of the material are determined by the large internal surface area, high absorption of proteins and the activity of heterodimeric proteins (integrins), which ensure cell adhesion to the matrix.
The microstructure is characterized by the presence of large free internal space. This makes the material an optimal scaffold for newly formed bone tissue.
After the operation, rapid and deep growth of blood vessels into the implanted material occurs, trophism is activated, and osteoblasts, young bone tissue cells involved in matrix synthesis, actively migrate from the patient’s tissues to the defect area. Further, during the regeneration process, osteoblasts are transformed into osteocytes - mature bone tissue.
On what day are sutures removed after dental implantation and the reasons for their separation.
This article provides detailed information about anterior dental implants.
Here https://www.vash-dentist.ru/implantatsiya/metodiki/o-sdache-analizov-pered-zubov.html read what tests you need to take before dental implantation.
Bio-Gide Collagen Membrane
Bio-Gide is the standard collagen membrane for the restoration of soft tissue and bone after dental surgery. This is a highly purified natural product that contains pork collagen. Soft tissues contain a large amount of collagen fibers, so the collagen membrane is used in the restoration of bone and periodontal tissue. The use of Bio-Gide helps the surgeon achieve the best and most predictable results and provides excellent wound healing. Bio-Gide has high therapeutic safety, which is highly valued by all leading surgeons.
The excellent qualities of Bio-Gide are achieved thanks to its three-dimensional, natural matrix structure and high biocompatibility. The structure of the Bio-Gide membrane is very similar to human collagen. The photo above shows human collagen under a microscope and below is the Bio-Gide membrane. The natural structure of collagen helps in the healing process - blood vessels grow through the collagen fibers.
The membrane performs several important functions in the regeneration process: protective, stabilizing, and is the basis for soft tissues.
Bio-Gide membrane has a two-layer structure, one side is smooth and the other is rough. The smooth top layer guides soft tissue healing, which occurs more easily and with better aesthetic results. The rough side of the Bio-Gide membrane helps growing bone cells.
There is no need to remove the membrane. The breakdown of the membrane into natural amino acids occurs without side effects, without tissue irritation.
Expected effect of application
The high integration of Bio-Oss with native bone tissue has been established by numerous histological studies. It was noted that already 15 days after surgery, osteoblasts formed mature collagen fibers on Bio-Oss.
It took about 6 weeks to form an extensive matrix network - collagen fibers woven into the biomaterial frame. Histological sections revealed organic substances that regenerated independently inside the implantation tissue or got there from the patient’s blood.
Thanks to its slow resorption, Bio-Oss serves as a stable scaffold for regenerating tissue and slows down the resorption of the graft. Studies have found that implantation material made from a mixture of substitute and native bone is more stable than implants in which autogenous bone chips are used as the only component.
In the case of the use of Bio-Oss, constancy of bone volume was noted throughout the observation , while the use of one autogenous material was accompanied by a decrease in the volume of implant material.
Histomorphometric analysis of tissues subjected to restoration using Bio-Oss showed that the volume of the mineral component in the regenerated bone is higher than in native bone tissue.
This may explain the high stability of implants containing Bio-Oss in combination with autogenous bone.
The adhesion strength of implants in the sinuses after sinus lift was also studied. It was found that 3 months after surgery, materials with Bio-Oss had 45% greater fixation strength than implants made from autogenous bone.
The video provides instructions on how to use the material.
With severe atrophy of the alveolar process in the area of the bottom of the maxillary sinus, when the height of the bone tissue is less than 4 mm, a sinus lift (SL) is usually required [3]. To increase the height of bone tissue in the area of the bottom of the maxillary sinus, a large number of materials are used. Autografts have a more pronounced regenerative potential than any other implantation materials [7, 9]. However, the need to harvest a significant amount of bone tissue and the presence of an additional surgical field significantly limit the use of autografts [5]. In this regard, implantation osteoplastic materials are often used to raise the floor of the maxillary sinus. The implantation material must be non-toxic, have osteoconductive and osteoinductive properties, be resorbed, and not cause immune reactions. The goal of targeted bone engineering is to regenerate bone that is morphologically and functionally identical to native bone tissue [2]. In world practice, positive results have been obtained in restoring bone tissue in the area of the floor of the maxillary sinus using cell grafts [14].
The purpose of this study is to comparatively evaluate the effectiveness of bone tissue formation using two materials used in LS: implantation material “Bio-Oss” and a tissue-engineered construct (TEC) based on multipotent stromal cells (MSCs) of adipose tissue (AT), predifferentiated in osteogenic direction. The clinical study was carried out on the basis of the Federal State Institution “TsNIIS” of Rosmedtekhnologii jointly with JSC “ReMeTex”.
Material and methods
Characteristics of patients.
Clinical observations are based on the examination and treatment of 25 patients with secondary adentia and severe bone deficiency in the upper jaw.
The height of the alveolar process to the bottom of the maxillary sinus, according to computed tomography (CT), ranged from 0.9 to 4.8 mm, the age of the patients was 29–60 years. All patients were somatically healthy, all underwent open SL: in 14 patients, the height of the alveolar process was increased using TIC of adipose tissue MSCs predifferentiated in the osteogenic direction (observation group) - Fig. 1
Figure 1. CT scan before TEC transplantation and after 4 months.
- and 11 - by introducing the implantation material “Bio-Oss” (comparison group) to the bottom of the sinus - Fig. 2.
Figure 2. CT scan before TIC implantation and after 6 months.
In patients with TIC VT transplantation, intraosseous implantation was performed 4 months after increasing the height of the alveolar process, and in those who were implanted with Bio-Oss, after 6 months. The timing of intraosseous implantation was justified by a previously conducted experimental study, which studied the timing and stages of bone tissue regeneration using TIC VT and Bio-Oss [1]. When forming the implant bed, a 2 mm diameter trephine was used instead of a pilot drill to obtain core biopsies.
To create TECs, a culture of MSCs from the stromal vascular fraction (SVF) of VT was used. VT SVF was isolated from lipoaspirate. Lipoaspiration was performed according to standard techniques under local infiltration anesthesia in the area of the anterior abdominal wall. The lipoaspirate was washed with Versene solution and disaggregated by incubation in Versene solution with the addition of 0.25% trypsin at 37 °C for 1.5 hours. The cell suspension was centrifuged for 10 min at 1100 rpm, the sediment was diluted with growth medium (DMEM/F12 1: 1 with the addition of autologous serum up to 10%, amikacin up to 500 mg/l), transferred to Petri dishes and incubated under standard culture conditions (37 °C, 5% CO2). The growth medium was changed every 3 days. For directed osteogenic differentiation, cells were seeded on 90 mm Petri dishes and, upon reaching 80% of the confluent monolayer, the growth medium was replaced with differentiation medium (DMEM with 10% autologous blood serum, 100 μg/ml amikacin, 50 mg/l L-ascorbic acid, 10 mmol). l sodium β-glycerophosphate and 10 nM 1,25-dihydroxyvitamin D3). The medium was replaced with fresh one every 3 days.
Preparation of platelet-rich plasma (PRP).
Blood was collected into a Vacuette® type vacuum system with sodium citrate. The blood was centrifuged at 1000 rpm for 10 min, the top layer (without red blood cells) was collected and centrifuged at 3600 rpm for 10 min. Most of the supernatant was removed, and the settled platelets were resuspended in the remaining plasma.
Preparation of TEC for transplantation.
Osteomatrix in the form of blocks and bone chips (Conectbiopharm LLC) was used as a carrier material. After washing the blocks and crumbs with Hanks' solution (PanEko) with cefazolin (JSC Sintez) (1 g/l), PRP containing 7 106 cells per 1 cm3 was carefully layered on them, and a thrombin solution (PZ Cormay) was added dropwise ") 50 U/ml in a 10% solution of calcium chloride (JSC Dalkhimfarm) before polymerization.
TEC transplantation.
All interventions were performed in a sterile operating room under local anesthesia. An increase in the height of the alveolar process in the area of the bottom of the maxillary sinus was carried out according to the standard method of performing open SL with access to the sinus in the area of its anterior wall: a horizontal incision was made along the top of the alveolar ridge in the area of missing teeth; skeletonized the alveolar process; a bone “window” was formed in the area of the anterior wall of the sinus until its mobility was achieved; the mucous membrane of the sinus was peeled off and, together with the bone fragment, it was displaced upward and inside the sinus; the resulting space in the maxillary sinus, as well as the formed bone window, was filled with TIC in the form of bone blocks and bone chips; The mucoperiosteal flap was placed in place, and the wound was sutured tightly.
Implantation "Bio-Oss".
Intraoperatively, osteoplastic material was mixed with autologous platelet-rich plasma, polymerized into a clot, and placed into the floor of the maxillary sinus as described above. The wound was sutured tightly.
X-ray research methods.
X-ray examination was carried out on a New Tom cone computed tomograph, slice interval - 2 mm, as well as on a digital orthopantomograph (ORTHOPHOS XG 5 DS).
Histomorphological study.
To study the characteristics of the bone regenerate, a histological examination was performed 4 months after transplantation. Tissue samples in the form of columns were taken with a trephine with a diameter of 2 mm, before forming a bed for installation of a dental implant and immediately after extraction, they were fixed in 10% neutral formaldehyde (Biooptica, Italy) for 48 hours. After washing in running water, the biopsy material was decalcified in a saline solution. formic acid (Biooptica, Italy) for 8 hours. Next, the samples were subjected to standard histological processing and embedded in paraffin (Histomix Extra, Biovitrum). Histological sections were obtained on a microtome (Leica, Germany) with a step of 7 μm. Sections were stained with hematoxylin and eosin according to Bock and Masson-Goldner. Morphometric analysis was carried out using the stereomorphometry method [10] in our modification and consisted of determining the proportion (in%) of bone tissue (BV/TV), material (MatV/TV), loose fibrous connective tissue (RfV/TV), coarse fibrous connective tissue tissue (FbV/TV), VT (FTV/TV) relative to all tissues in the regenerate. The normality of distribution of variants in the group was determined by the Shapiro-Wilk test. If the variant distribution corresponded to normal, one-way analysis of variance was used to establish intergroup differences, followed by Newman-Keuls testing and t-testing (for pairwise comparison of data from the control and experimental groups). If the distribution of the variant in the group did not correspond to normal, the Kruskal-Walliss rank analysis of variance was used, followed by Mann-Whitney testing (for pairwise comparison of data from the control and experimental groups). A 5% significance level was selected for all comparisons.
Results and discussion
The height of the alveolar process when using TIC VT was 0.9-3 mm, when using Bio-Oss - 1.0-4.8 mm, the height of the alveolar process after transplantation, according to CT data, was 10-16 and 9- respectively. 15 mm.
According to the CT study, the average increase in the height of the alveolar process during transplantation of TIC VT was 10 mm, with implantation of Bio-Oss - 8 mm, while the minimum height of the alveolar process before transplantation in the 1st group was 0.9 mm, in 2nd - 1.0 mm.
Histological examination 4 months after TIC transplantation showed that the bone regenerate consisted predominantly of particles of mature lamellar bone tissue, oriented in space like beams of cancellous bone. The proportion of bone tissue (BV/TV) is on average 46.6%. The interbeam space is filled by 31% with loose fibrous connective tissue (RfV/TV). Among the cancellous bone beams, material inclusions (MatV/TV) were determined - 2.9%, which were in close contact with the newly formed bone tissue and were often included in its architectonics. Loose fibrous connective tissue (FCT) filled the entire interbeam space and contained a significant number of vessels. No significant infiltrative, giant cell or inflammatory reactions to the material were detected (Fig. 3, 5).
Figure 3. Bone regenerate 120 days after TIC VT transplantation.
Figure 5. The ratio (in %) of parts of the regenerate 4 months after transplantation of VT TEC.
According to histological examination 6 months after Bio-Oss implantation, the bone regenerate consisted mainly of particles of immature bone tissue, oriented in space along the surface of the material and sometimes merging with each other. The proportion of bone tissue (BV/TV) is on average 33.6%. The interbeam space was filled by 41% with coarse fibrous connective tissue (FCT) (FbV/TV). Among the fields of fibrous tissue, inclusions of material (MatV/TV) were determined - 20.7%, which were in close contact with the newly formed bone tissue. A significant number of giant cells were detected both around the material and in the interbeam space (Fig. 4, 6).
Figure 4. Bone regenerate 180 days after Bio-Oss implantation.
Figure 6. The ratio (in%) of parts of the regenerate 6 months after Bio-Oss implantation.
To increase the height of the maxillary sinus floor, osteoinductive materials based on calcium phosphate of one origin or another are traditionally used, primarily because they are inexpensive and effective materials for directed bone regeneration.
Morphological studies conducted in the long term show that during implantation, for example, “Bio-Oss”, the proportion of bone tissue on average fluctuates about 30% [4, 12], while with autotransplantation it is 40-60% [8, 13 ]. Since obtaining an autograft requires an additional surgical field and donor areas are limited, cell grafts can become a worthy alternative to autografts. Thus, during transplantation of living bone tissue equivalents, the proportion of bone regenerate is comparable to that during autotransplantation [6, 11].
In addition, our study revealed marked differences in the course of the regenerative process during TEC transplantation and Bio-Oss implantation. If the interbeam space after TEC transplantation was mainly filled with loose fibrous connective tissue, rich in blood vessels, then in the samples after hydroxyapatite implantation a significant amount of coarse fibrous connective (scar) tissue was detected, which indicated pathological regeneration. Severe infiltration by osteoclasts and macrophages in combination with sclerotic changes indicated a negative reaction of the body to the osteoplastic material “Bio-Oss”.
Prospects
Today, bone transplantation mainly uses autogenous materials and PRP (platelet-rich plasma). The latter is a gel containing blood plasma and platelets, which play a major role in tissue regeneration and healing.
Apparently, the time is not far when surgeons will have autogenous biomaterials grown outside the body at their disposal.
However, for any implantation materials, regardless of their origin, a carrier is required that ensures effective tissue regeneration and meets a number of requirements, including:
- high cell adhesion;
- saving space;
- positive effect on bone morphology;
- support cell differentiation.
And from this point of view, bone substitutes like Bio-Oss, capable of working together with PRP, can be considered as very promising materials.
Alternatives to extensions
The implantologists of the Smile-at-Once clinic are fluent in modern dental implantation techniques, so we are pleased to offer our clients treatment protocols that allow us to do without additional extension procedures.
Atrophy is a limitation for only two-stage implantation with delayed loading. If we are talking about restoring one tooth, especially in the smile area, then building up the cancellous bone and using two-component implants is really justified.
One-stage implantation with immediate loading
But in the absence of a large number of teeth, as well as with complete edentia, bone augmentation along the entire row, firstly, will be a rather expensive procedure, and secondly, it will be overly complex and time-consuming. That is why in these situations, implantation methods with immediate loading are recommended - they allow you to rehabilitate the bone and return the patient to a full life almost immediately.
This protocol uses specially designed implants that are attached both to the cancellous bone and to the basal region, cortical plate, and in some situations, the zygomatic bone and buttresses are involved. They are instantly loaded with the prosthesis, so the jawbone receives the usual load and natural metabolic processes are launched inside it. Cell nutrition is normalized, they receive enough oxygen, actively grow and tissue is restored. Therefore, bone atrophy in this situation is not an obstacle to comfortable and complete treatment, as well as reliable fixation of implants.
Read more about the technology of one-stage implantation with immediate loading >>>
1 Lars Schropp, A. Wenzel, L. Kostopoulos, et al. Bone Healing and Soft Tissue Contour Changes Following Single-Tooth Extraction: A Clinical and Radiographic 12-Month Prospective Study. 2 Based on materials from the portal studopedia.ru. Biochemistry of bone tissue.
conclusions
The use of natural biomaterials in maxillofacial surgery is becoming increasingly popular. Their developed internal surface has a positive effect on the adhesion and differentiation of cells in the defect area.
Low resorbability increases volume stability. The natural structure of the carriers, close to human ones, creates favorable conditions for the regeneration of new bones. All this promises materials like Bio-Oss to be in high demand in surgery.
If you find an error, please select a piece of text and press Ctrl+Enter.
Tags bone materials
Did you like the article? stay tuned
Previous article
Root canal obturation – prolonging the life and full functions of the tooth
Next article
When is the use of the Persin apparatus for the correction of malocclusions justified?
Features of surgery
Typically, bone restoration and implant placement are performed simultaneously. To form new bone, the defect is filled with Bio-Oss biomaterial, and for directed regeneration, a Bio-Hide membrane is applied to the wound.
After surgery, slight swelling and swelling may occur, which can be eliminated with a cold compress. During the first 10-14 days, while brushing your teeth, you should avoid trauma to the operated area and use an antibacterial rinse. If severe pain occurs, the doctor may prescribe a pain reliever. At the same time, it is important to regularly see a dentist, even if nothing is bothering you and healing is proceeding well.