Author of the article:
Soldatova Lyudmila Nikolaevna
Candidate of Medical Sciences, Professor of the Department of Clinical Dentistry of the St. Petersburg Medical and Social Institute, Chief Physician of the Alfa-Dent Dental Clinic, St. Petersburg
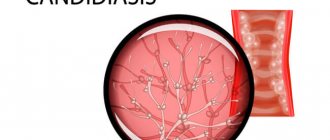
Candidiasis or, otherwise, thrush is an infectious disease, the main cause of which is infection with Candida fungi. These fungi belong to the same species as yeast and are part of the natural microflora of the vast majority of healthy people. The maximum concentration of these opportunistic microorganisms is observed in the intestines, nasopharynx, and vagina; Some fungi can also be found on the surface of the skin.
In a normal, healthy state of the body, the fungus does not cause any unpleasant symptoms. However, when the immune system is weakened and other provoking factors appear, Candida actively multiplies, resulting in discomfort, itching, burning and other manifestations of thrush. This disease can affect various tissues and organs; Candidiasis of the oral mucosa is also common.
Most often, infants suffer from this disease: according to statistics, up to 20 percent of children under the age of one year have suffered from candidiasis at least once. About 10 percent of people over 60 also suffer from symptoms of this infection. It occurs more often in women than in men; very often, signs of the disease appear in smokers. There are many other factors that contribute to the development of candidiasis in the mouth.
Causes of oral candidiasis
The main reason for the occurrence is a decrease in immune status, as a result of which the uncontrolled proliferation of microflora begins. Reduced immunity is observed in older people and infants, in patients suffering from HIV, AIDS and other diseases associated with immunodeficiency, in those who regularly expose the body to excessive stress, neglect the rules of a healthy diet and violate work and rest patterns. Risk factors include reasons such as:
- Use of medications.
Taking antibiotics, immunosuppressants (drugs that suppress the immune system) and some other medications leads to disruption of the immune system and the natural balance of microflora in the body. Oral contraceptives, which affect hormonal levels, have a similar effect. - Pregnancy.
During pregnancy, a sharp and significant change in hormonal levels occurs, which can lead to a surge in the activity of pathogenic and opportunistic microflora. - Radiation and chemotherapy.
Often occurs in patients undergoing drug and radiological treatment for cancer. - Injuries to mucous membranes.
Violation of the integrity of the mucous membranes leads to loss or deterioration of the barrier function, as a result of which the fungus enters deep into the tissues, causing inflammation and other symptoms. Small, but constantly recurring injuries are especially dangerous - for example, when wearing incorrectly fitted dentures or braces. - Overwork and stress.
Prolonged stress of physical and mental forces leads to a deterioration in the protective function of the body. Similar consequences are caused by hypothermia or overheating, regular lack of sleep, insufficient, excessive or simply unbalanced nutrition, abuse of alcohol, nicotine, and narcotic substances. - Hypo- and vitamin deficiency.
May be caused by a lack of nutrients, in particular vitamins B and C. - Somatic diseases.
Frequent companions of candidiasis include tuberculosis, dysbacteriosis and other pathologies of the gastrointestinal tract, diseases of the adrenal glands and other endocrine glands. Candidiasis is a contagious disease. A large number of pathogenic microorganisms are transmitted through kissing and sexual contact, through the use of shared dishes, towels and other household items. Infection can also occur during childbirth (vertical transmission from mother to fetus). In addition, there is a risk of infection through contact with infected pets.
Complication
With timely treatment, candidiasis does not cause any particular harm to health. But the symptoms of candidiasis can cause a lot of discomfort. Long-term, it can lead to damage to other organs, most often the urethra, bladder and kidneys. In particularly severe cases, the progressive disease can affect the reproductive organs, leading to infertility in both men and women. But candidiasis poses the greatest danger to pregnant women, because... the risk of fetal damage is very high.
Types of disease
The clinical picture of oral candidiasis is classified:
- For clinical and morphological.
- With the flow.
- By localization.
Clinical and morphological is divided into:
- Hyperplastic.
- Erosive-ulcerative.
- Pseudomembranous.
- Atrophic.
The clinical picture, classified according to the course, is divided into:
- Chronic.
- Spicy.
By localization:
- Cheilitis.
- Gingivitis.
- Glossitis.
- Stomatitis.
- Tonsillitis, etc.
Based on the clinical picture, oral candidiasis comes in several types:
- Chronic hyperplastic.
- Candida infection.
- Chronic atrophic.
- Acute pseudomembranous.
- Chronic pseudomembranous.
- Acute atrophic.
Advantages and disadvantages
| pros | Minuses |
|
|
Symptoms
Infection of the oral mucosa by Candida fungus can take various forms, each of which has its own characteristics of symptoms. The most common forms of the disease are candidal angulitis, glossitis, cheilitis, and stomatitis. There are both acute and chronic forms of the disease.
- Pseudomembranous acute candidiasis is the most common form and most often occurs in infants and the elderly. This form is characterized by the appearance of severe swelling and hyperemia (redness) of the mucous membranes. In addition, a characteristic whitish coating forms on the surface of the lips, palate, back of the tongue and the inside of the cheeks. If the plaque is scraped off, the surface of the mucous membrane underneath will be macerated (softened) or ulcerated and bleeding. In this case, patients complain of pain, burning or itching in the mouth; Eating becomes very difficult. Very often the process spreads to the esophagus and pharynx.
- Acute atrophic candidiasis of the oral mucosa usually develops due to the lack of adequate treatment. The upper part of the mucous membranes (epithelium) is exfoliated, the mucous membrane becomes thin, red or, on the contrary, swollen. The patient’s tongue and the corners of the lips also acquire a bright red color; the papillae on the tongue atrophy and smooth out. The plaque is absent or is found only in hard-to-reach places.
- Hyperplastic chronic candidiasis is characterized by the formation of a large number of papules and plaques of irregular or round shape. They are located close to each other on the mucous membrane of the tongue and cheeks and often become soldered and fused. Around each such formation there is a thin rim of reddened, inflamed tissue. It is difficult to scrape off or otherwise remove such a plaque. The oral cavity becomes dry and rough; When chewing, speaking, and even at rest, patients experience significant discomfort and pain. It should be noted that this disease most often affects men over 30 years of age.
The main cause of the chronic atrophic type is constant injury to the mucous membranes, for example due to wearing a prosthesis. Symptoms of the disease are localized in the affected area. Redness of the mucous membrane occurs (often along the contour of the lesion), plaque forms, pain and burning occur, and the membranes become dry.
Diet No. 4c: do's and don'ts
Diet No. 4c is not as strict as Diet No. 4. It is believed that a person has already suffered from the disease and is ready to return to normal life, but must do this gradually to prevent additional stress on the body. You can eat different food groups, but stick to restrictions.
You can eat dry
biscuits and cookies, day-old bread, but avoid rich and sweet pastries and pies. You can eat soups with vegetable broth, lean meat and fish, baked, boiled or steamed, but you should avoid sausages and anything fried. The same applies to egg dishes: the diet may include steamed omelettes and protein dishes, but there should be no raw, hard-boiled or scrambled eggs. It is permissible to eat crumbly porridges made from tender cereals and small pasta, as well as boiled vegetables, but they must be cooked in water or with a minimum amount of oil.
Prohibited
dairy and sweet cereals, raw vegetables, large types of pasta, some coarse cereals, fruits and berries with high acidity, whole milk and fermented milk products, sweet carbonated drinks, strong tea, coffee and alcohol, vegetable and vegetable oil. You can replace all these products with more “gentle” analogues: bake apples for sweets or choose fruits with a delicate texture, consume milk only as additives to other dishes, replace fermented milk products with non-acidic cottage cheese or curd paste, drink weak tea or rosehip decoction, you can allow Add a little natural butter to your dishes.
How does the disease manifest in children?
In children, the disease occurs in an acute form and is accompanied by the appearance of redness and swelling in the oral mucosa. The child sleeps poorly, may have no appetite, and becomes tearful.
The disease can occur in children for the following reasons:
- Weakening of the immune system.
- Infection during breastfeeding.
- Transmission of the fungus during childbirth.
- Infection through household items.
If the disease is not diagnosed and treated in a timely manner, a whitish coating resembling cottage cheese will soon appear in the child’s mouth, and in an advanced stage, ulcers will appear, which are accompanied by bleeding and cause severe pain in children.
Mineral deficiency
In case of intestinal diseases, the body receives insufficient minerals, but this deficiency can be replenished with the help of dairy products
. Not only do they contain a lot of minerals, but they are also easily absorbed by the body. Dairy products can provide the body with a sufficient amount of phosphorus and calcium, but one must keep in mind that not all dairy products can be well tolerated by the body in case of intestinal diseases. For example, fresh milk may be too “heavy”, and fermented milk products, due to their increased acidity, can irritate the walls of the stomach.
The most neutral and useful product for intestinal diseases is unleavened cottage cheese.
, as well as unsalted and low-fat
cheese
. These products can be an alternative to kefir and yogurt. It is only important that the products are fresh and natural, without additional spices or flavor enhancers.
Diagnostics
To make an accurate diagnosis, a combination of several methods is used - from a simple examination and questioning of the patient for complaints to laboratory methods, such as culture, microscopic examination of biomaterial, analysis of the degree of contamination of the oral cavity with fungal mycelium.
Oral candidiasis is accompanied by a number of characteristic external signs, in particular the formation of plaque, bad breath, ulceration and hyperemia of the mucous membranes. However, laboratory methods make it possible to accurately determine the type of pathogen and exclude the possibility of a secondary infection, which may affect the nature and duration of treatment.
Differential diagnosis is used to separate cases of candidiasis from aphthous stomatitis, leukoplakia, lichen ruber, streptococcal infection and other infectious pathologies of the oral cavity.
Diet No. 4 for intestinal diseases
People who suffer from intestinal diseases have probably heard or even experienced “ diet number 4.”
" This is a special diet that was developed for the treatment and prevention of intestinal diseases. “Diet No. 4” has several more variations, which are indicated by letters. They are based on the same “diet No. 4”, but with certain relaxations; adjustments are made for the severity of the disease and the stage of its cure.
“Diet No. 4” itself is the most gentle for the digestive tract, and therefore the most strict. It provides a diet low in fat and carbohydrates. The diet should not contain fried, smoked, salted or other hot or spicy foods. Only food that has been steamed or boiled and then pureed is allowed.
A common variation of “diet No. 4” is “ diet No. 4c”
” is prescribed to people who have already suffered an acute stage of intestinal disease and are gradually returning to their usual nutritious diet. “Diet No. 4b” helps to restore weight lost due to illness and involves split meals.
How to treat oral candidiasis?
Treatment is carried out using local and general, specific and symptomatic remedies. Among the main goals of therapy are the elimination of foci of infection in the oral cavity (sanitation), treatment of diseases that accompany candidiasis and are risk factors, and stimulation of the body's defenses. The total duration of treatment is usually at least 7-10 days.
As a means of local therapy, rinses are used - using solutions of boric acid, soda, sodium tetraborate. For a longer and more effective effect, such products can be used in the form of applications - moistening a cotton swab or bandage with the solution.
Nystatin for oral candidiasis is used to combat the main cause of the disease - a fungal infection. Treatment of candidiasis in the mouth may also include the use of other antimycotic (antifungal) drugs - for example, levorin ointment. The best effect is achieved by using several drugs, alternating them for several days.
Antifungal drugs are also prescribed for systemic therapy - in this case, medications for oral candidiasis and other infections such as Lamisil, Diflucan, Levarin, Nizoral, etc. are taken orally. In the most severe cases of the disease, the treatment regimen includes taking immunomodulatory drugs, as well as the use other agents that have a stimulating effect on the immune system and help strengthen the body’s own defenses.
An equally important task is to protect against additional fungal and bacterial infections that can join the Candida infection and complicate the course of the disease. For this purpose, rinses with antiseptic solutions - fucorcin, iodinol and others.
As an alternative, you can use ASEPTA antiseptic mouth rinse, which contains the active ingredients chlorhexidine and benzydamine. Both of these substances have broad antimicrobial effects. Regular use of ASEPTA rinses also has a pronounced anti-inflammatory effect and helps not only eliminate unpleasant symptoms, but also reduce the risk of complications.
Intestinal candidiasis
Ph.D. Yu.O. Shulpekova
MMA named after I.M. Sechenov
In recent decades, opportunistic infections caused by opportunistic fungi have occupied a special place in the practice of clinicians of various specialties.
Paradoxically, this is partly due to the successes that modern medicine has achieved in the treatment of cancer and in the fight against pathogens of serious infections. In addition, it is obvious that in recent decades there has been an increase in the intensity of the impact on the human body of external factors that cause the development of immunosuppressive conditions. In addition, the end of the 20th century was marked by a significant spread of the fatal disease HIV infection.
Pathological conditions caused by the influence of fungi of the genus Candida on the human body also belong to the category of opportunistic mycoses.
Characteristics of the pathogen
Members of the genus Candida are yeasts related to Ascomycetes.
The genus Candida includes various species (Candida spp.), among which the main ones as causative agents of candidiasis are: Candida albicans, Candida tropicalis, Candida parapsilosis, Candida glabrata, Candida dubliniensis, Candida lusitaniae, Candida krusei.
Candida spp. They are a component of microflora that is symbiont for humans. In 10-25% of the population who do not have clinical signs of fungal infection, Candida spp. are inconsistently detected in the oral cavity, in 65-80% in the intestinal contents. Candida spp. are found in the detritus of gastroduodenal ulcers in approximately 17% of cases.
According to modern ideas, under normal conditions the main “habitat” of Candida spp. in the human body is the intestines. The proportion of these fungi in the intestinal microbial population is negligible. Growth of colonies of Candida spp. in the human body it is partly regulated due to the work of the immune system. The main place in this process is occupied by the links of nonspecific immunity: mononuclear phagocytes (monocytes/macrophages) and polymorphonuclear leukocytes [1,3].
Intestinal symbiont bacteria also play a very important role in limiting the growth of the Candida population. The normal microflora inhabiting the lumen of the gastrointestinal tract produces substances with antibacterial activity (in particular, bacteriokines and short-chain fatty acids), which prevent the introduction of pathogenic microorganisms and excessive growth, the development of opportunistic flora. Escherichia coli, enterococci, bifidobacteria and lactobacilli have the most pronounced antagonistic properties.
The term candidiasis implies a pathological process, the basis of which is the excessive growth of Candida primarily in the gastrointestinal tract and secondarily in other areas (on the mucous membrane of the genitals, bronchi, in parenchymal organs) [1,3,5].
Candida virulence factors
Fungi of the genus Candida are adhesive to epithelial cells. Attachment to the mucous membrane is one of the conditions for further invasion of the microorganism into the underlying tissue. The adhesion capacity of different Candida species varies considerably; this ability is highest in C. albicans, C. tropicalis, C. dubliniensis; the smallest in Candida glabrata, Candida krusei. Mucin, a glycoprotein of the cell wall of epithelial cells, plays an important role as a protective barrier that prevents the microbe from attaching to the mucous membrane.
Factors of aggression of these microorganisms include proteases and glycosidases that can intensively break down mucin.
The ability to rapidly form filaments of pseudomycelium is also considered as a virulence factor; this feature is most pronounced in C. albicans.
The virulence of microorganisms is subject to intraspecific variability, depending on the genotype [1,3].
Risk factors for developing candidiasis
As general factors predisposing to the development of candidiasis of the digestive organs and subsequent lymphohematogenous dissemination of fungi, as in the cases of other opportunistic infections, are conditions in which there is a lack of immune defense of the body. These include:
1) Physiological immunodeficiencies (newborn period and early childhood, senile immunodeficiency, pregnancy, stress conditions).
2) Congenital immunodeficiencies (DiGeorge, Nezelof, Shediac-Higashi syndrome, etc.).
3) Infection with the human immunodeficiency virus in the terminal stage (acquired immunodeficiency syndrome). Mycoses make up 70% of the clinical manifestations of HIV infection.
4) Oncological diseases (including hematological malignancies); chemotherapy of malignant tumors, accompanied by severe granulocytopenia (<1x109 granulocytes per l). The development of candidiasis during antitumor therapy is usually associated with suppression of the functions of the immune system, observed as an undesirable effect of treatment. At the same time, there are suggestions that cytostatics and radiation therapy inhibit the protective functions of the intestinal epithelium and promote the translocation of Candida to other organs. During chemotherapy, the percentage of fungal microorganisms adhering to enterocytes increases.
5) Autoimmune and allergic diseases, especially when prescribing glucocorticosteroids.
6) Organ transplantation (use of immunosuppressants in the post-transplant period). More than half of patients scheduled for bone marrow transplantation have a picture of systemic candidiasis even before transplantation.
7) Endocrinopathies (decompensated diabetes mellitus, autoimmune polyglandular syndrome).
 Other diseases and conditions (shock conditions, anemia, hepatitis, cirrhosis of the liver, chronic infections, malabsorption syndrome, etc.). In pathological conditions accompanied by a decrease in blood supply to the intestine, the translocation of fungi into other tissues increases. Digestion and absorption disorders are accompanied by excessive growth of microorganisms in the intestinal lumen.
Other diseases and conditions (shock conditions, anemia, hepatitis, cirrhosis of the liver, chronic infections, malabsorption syndrome, etc.). In pathological conditions accompanied by a decrease in blood supply to the intestine, the translocation of fungi into other tissues increases. Digestion and absorption disorders are accompanied by excessive growth of microorganisms in the intestinal lumen.
9) Antibiotic therapy (usually long-term use of broad-spectrum drugs). The introduction of antibacterial drugs can lead to an imbalance in the microbial biocenosis of the intestine, as a result of which excessive development of the candidal population in the intestine is possible. Prescription of tuberculostatic drugs for 3-4 months. accompanied by the development of intestinal candidiasis in 58-62% of cases. The risk of developing idiopathic antibiotic-associated diarrhea depends on the dose of antibiotic administered; this disease usually occurs without fever and leukocytosis in the blood and in the absence of laboratory signs of Clostridium difficile infection. It is believed that in about a third of cases, the development of idiopathic antibiotic-associated diarrhea is caused by intestinal candidiasis.
10) Unbalanced nutrition (deficiency in the diet of proteins, vitamins). Animal experiments have shown that insufficient protein intake into the body is accompanied by a decrease in the phagocytic and bactericidal activity of the macrophage component, incomplete phagocytosis and an increase in the permeability of the intestinal barrier to Candida albicans [1,3,4,5].
According to autopsy data, candidiasis of the duodenum, small and large intestine is found in approximately 3% of dead patients (only macroscopic changes were taken into account). Moreover, half of the cases occur in patients receiving chemotherapy for malignant neoplasms [1].
Pathogenesis of the development of intestinal candidiasis
Research in recent years has largely clarified the patterns of interaction between Candida fungi and the host organism. According to modern concepts, two fundamentally different mechanisms of the pathogenesis of candidiasis of the digestive organs can be distinguished: invasive and non-invasive candidiasis [3].
Invasive candidiasis is caused by the introduction of a filamentous form of the Candida fungus into tissues. The first stage of candidiasis, as an infectious process, is adhesion to epithelial cells, then invasion occurs into the epithelial layer, penetration beyond the basement membrane. These manifestations of microbial aggression macroscopically correspond to erosive and ulcerative defects of the intestinal wall of various sizes and shapes, cracks, membrane deposits (similar to those in pseudomembranous colitis), polypoid or segmental circular formations.
With progressive invasion, the development of lymphohematogenous dissemination of fungi is possible (systemic candidiasis with damage to the mucous membranes of other organs; generalized candidiasis with damage to visceral organs). An experimental model of animals orally infected with C. albicans under conditions of immunosuppression showed the initial occurrence of erosions and ulcers of the mucous membrane in the ileum, colonization of intestinal lymphoid formations, their necrosis and further dissemination. The absence of macroscopic changes should probably not be considered as evidence against invasive candidiasis.
In disseminated forms of candidiasis, multinucleated giant cells containing fungi are found in the lymph nodes and ducts, which probably reflects the phenomenon of incomplete phagocytosis.
Invasive candidiasis is more often observed in organs lined with stratified squamous epithelium (oral cavity, esophagus), and less often with columnar epithelium (stomach, intestines), which is probably due to the peculiarities of local immune defense.
Non-invasive candidiasis is not accompanied by the transformation of the fungus into a filamentous form; There is an excessive growth of its colonies in the lumen of the hollow intestinal organ. It is assumed that the disruption of cavity and parietal digestion, the penetration of microbial components and metabolites into the systemic bloodstream, and the development of a more or less pronounced systemic immune-inflammatory reaction are of important pathogenetic significance.
Based on all of the above, it should be emphasized once again that mucosal candidiasis of extraintestinal localization or generalized candidiasis with damage to parenchymal organs is a manifestation of the translocation of fungi from the intestinal lumen, where the bulk of these saprophytic fungi are represented. Candidiasis of extraintestinal localization (for example, the oral cavity or genitals) is a manifestation of systemic candidiasis, originating from the intestines.
The following is the classification of candidiasis of the digestive organs:
1. Oropharyngeal candidiasis (cheilitis, gingivitis, seizures, glossitis, stomatitis, pharyngitis).
2. Esophageal candidiasis (complications: bleeding, stricture).
3. Gastric candidiasis:
diffuse (specific erosive-fibrinous gastritis);
focal (secondary to gastric ulcer).
4. Intestinal candidiasis:
invasive diffuse;
focal (secondary to duodenal ulcer, with nonspecific ulcerative colitis);
non-invasive (overgrowth of Candida in the intestinal lumen).
5. Anorectal candidiasis:
invasive candidiasis of the rectum,
perianal candidal dermatitis.
Below we describe the main manifestations of candidiasis of the intestine, which, as mentioned above, is the basis for the development of systemic manifestations.
Clinical picture of intestinal candidiasis
The features of the course of intestinal candidiasis are not clearly defined, not well studied and little known to most practicing doctors. It is characteristic that in patients who died from various causes and whose autopsy revealed macroscopic changes in the intestine corresponding to invasive candidiasis, during their lifetime, as a rule, very scanty symptoms from the gastrointestinal tract were noted, and the endoscopic diagnosis was often erroneous. Often, when single ulcerations of the intestinal wall are detected, the doctor finds it difficult to interpret them, and based on the results of a morphological study, a conclusion is given about nonspecific inflammatory changes in the edges of ulcerative defects, while a targeted mycological study is not carried out.
Clinical manifestations of intestinal candidiasis may vary depending on the level of damage.
With diffuse invasive intestinal candidiasis, there are manifestations of enterocolitis: complaints of spastic abdominal pain, flatulence, the presence of pathological impurities in the stool (blood and mucus), there are usually signs of systemic candidiasis (damage to the mucous membranes of the oral cavity, genitals). Endoscopic examination reveals changes similar to fibrinous ulcerative colitis.
With invasive focal intestinal candidiasis, the manifestations of the disease may resemble a persistent course of duodenal ulcer or nonspecific ulcerative colitis, resistant to traditional therapy.
With non-invasive intestinal candidiasis, patients complain of loose stools, flatulence, abdominal discomfort, with positive clinical and laboratory dynamics when treated with antifungal drugs.
With invasive candidiasis of the rectum, symptoms of proctitis (pain, tenesmus, pathological impurities in the stool) may be observed. In some cases, this is accompanied by the phenomenon of perianal candidodermatitis.
Intestinal candidiasis is often accompanied by low-grade fever [1,3,5].
Complications
As complications of intestinal candidiasis, it is possible to develop intestinal perforation, penetration of ulcers into surrounding organs, bleeding, generalization with damage to parenchymal organs, and the development of fungal sepsis.
Damage to parenchymal organs (liver, gallbladder, pancreas, etc.) very often accompanies deep neutropenia (less than 500 neutrophils per mm3 of blood) and is observed in the terminal phase of AIDS [1,3,5].
The mortality rate for invasive candidiasis reaches 25-55%. For some categories of patients (transplant recipients, patients with acute leukemia), invasive mycoses are the main cause of death.
Diagnostics
The issue of diagnosing intestinal candidiasis and determining indications for antifungal therapy is extremely important.
In recognizing mucosal candidiasis, it is necessary to distinguish between physiological “candidiasis” and the infectious process caused by this fungus.
For the diagnosis of candidiasis, the detection of Candida in sterile fluids (cerebrospinal fluid, lavage fluid, peritoneal fluid, etc.) or the detection of fungi in tissues (changes such as granulomas with necrosis are often found) are absolutely informative.
To increase the sensitivity of cultural and morphological methods for diagnosing candidiasis, it is recommended to examine several biopsies of the mucous membrane.
The biopsied tissue is collected in 2 sterile Petri dishes or sterile jars with a screw cap; one sample is filled with a 10% formaldehyde solution and sent for histological examination, the second is used for mycological examination. The material is transported to the microbiological laboratory, protected from direct sunlight. It is necessary that the material be delivered for mycological examination no later than 1 hour after collection when stored at room temperature or no more than 3 hours when stored at +4ーC.
Microscopic examination must be carried out in native and stained preparations.
The CHIC reaction (treatment with chromic acid) or its modification, Gridley staining, makes it possible to identify the pathogen in a tissue or smear by staining the polysaccharide components of the cell wall; To suppress the color of surrounding tissues, a “counter-paint” with light green, methanil yellow, etc. is used. In this case, only invading fungal cells are detected, while at the same time it is impossible to judge the reaction of the surrounding tissues. Therefore, it is also necessary to evaluate preparations “counter-stained” with hematoxylin and eosin.
Pseudomycelium of Candida can also be detected in a smear of the mucous membrane or a smear of the bottom of the ulcer (Romanovsky Giemsa stain).
An imprint is made on the surface of a dense nutrient medium in a Petri dish with a piece of tissue being examined, then sieving is carried out with a loop. The same piece of tissue is placed in 50 ml of liquid nutrient medium (Sabouraud medium, wort) and incubated at +37ーC for 5 days.
Methods for rapid identification of C. albicans are widely used. This species of Candida is capable of forming germ tubes and short filaments of pseudomycelium within 2-4 hours at +37ーC on blood serum, egg white and other similar media. For the species C.albicans, this phenomenon is typical in 90% of cases.
For effective treatment, it is necessary to strive to determine the species of Candida fungi and determine the individual sensitivity of the strain to antimycotic agents; some strains of Candida lusitanlae are resistant to amphotericin, and Candida krusei and Candida glabrata are resistant to fluconazole.
Detection of Candida in the blood allows a diagnosis of generalized candidiasis to be made only in combination with appropriate clinical symptoms (repeated detection of Candida in the blood is especially informative). It should be remembered that in 70-80% of patients who actually suffer from generalized candidiasis, fungi cannot be detected by blood culture.
The value of serological methods consists mainly in identifying patients with probable invasive mycoses. False-positive results of serological tests are possible with mycocarriage and in healthy people sensitized by fungal antigens; false-negative tests can occur in immunodeficiency.
Original procedures for the detection of antigens and antibodies of some metabolites of fungal cells are proposed; special diagnostic kits have been created. An example is Pastorex Candida, for the determination in the latexagglutination reaction of repeating oligomannose epitopes of antigenic structures expressed on a large number of fungal macromolecules. The Platelia Candida kit can be used to detect Candida antigen-mannan, for example, in the blood serum of a patient with the organism circulating. Using the first kit, the threshold for determining antigenic structures is 2.5 ng/ml; using the second in conjunction with the method, the threshold for determining antigenic structures is 0.5 ng/ml.
In the diagnosis of non-invasive intestinal candidiasis, in which there is no tissue biopsy material for mycological examination, it is proposed to use the following criteria as a diagnostic standard: growth over 1000 CFU/g Candida spp. when inoculating intestinal contents taken under sterile conditions, in combination with symptoms of intestinal dyspepsia and positive clinical and laboratory dynamics during treatment with antimycotic drugs [1]. Unfortunately, proper collection of intestinal contents for culture is technically challenging; The widespread method of stool culture for dysbacteriosis in our country cannot serve as a basis for assessing the actual composition of the intestinal microflora [1,3,5].
In diagnosing any form of candidiasis of the digestive organs, it is important to take into account the presence of predisposing risk factors in the patient. The incidental detection of candidiasis should serve as an incentive to search for such a background factor. It is important to remember that candidiasis can act as an early manifestation of common diseases accompanied by the development of immunodeficiency.
Considering the above, it would probably not be entirely correct to formulate the diagnosis briefly as “Candida” without indicating the underlying condition.
The differential diagnosis of invasive intestinal candidiasis (if macroscopic changes in the intestine are detected) must be made with chronic inflammatory bowel diseases, antibiotic-associated diarrhea due to C. difficile infection, malignant lesions, and ischemic colitis. The non-invasive form of candidiasis should be differentiated from a wide range of enteritis and colitis of other etiologies. Indirect evidence in favor of the presence of intestinal candidiasis may be extraintestinal systemic manifestations of candidiasis.
Treatment
It should be emphasized once again that the mere detection of fungi of the genus Candida during bacteriological analysis of feces (according to the accepted method in Russia), regardless of the presence or absence of symptoms of intestinal dyspepsia, cannot serve as an indication for prescribing antifungal drugs to the patient.
To treat intestinal candidiasis, it is necessary to prescribe drugs that are not absorbed from the intestinal lumen.
Today there are a variety of antimycotic agents. Drugs such as amphotericin B, itraconazole, ketoconazole, fluconazole have a systemic effect and can be used topically, orally and intravenously. When administered orally, these drugs are almost completely adsorbed from the upper gastrointestinal tract and do not reach the level of the ileum, where the main population of fungi is concentrated. In addition, the use of systemic antifungal drugs is often accompanied by side effects, in particular, the development of toxic hepatitis.
Practically non-absorbable antimycotic agents include levorin, nystatin and natamycin (Pimafucin). The prescription of levorin and nystatin with a fairly high frequency is accompanied by the development of side effects (dyspeptic symptoms, allergies, toxic hepatitis).
Pimafucin (natamycin) is a broad-spectrum antifungal polyene antibiotic. Has fungicidal potential. Pimafucin binds sterols of cell membranes, disrupting their integrity and functions, which leads to the death of microorganisms. Most pathogenic yeasts are sensitive to natamycin, most notably Candida albicans. Pimafucin is more effective than nystatin. There have been no cases of natamycin resistance in clinical practice; with repeated use of this drug, its minimum inhibitory concentration against C. albicans does not change. Pimafucin tablets act only in the intestinal lumen and are practically not absorbed from the gastrointestinal tract.
When using tablets in the first days of treatment, dyspeptic symptoms such as nausea and diarrhea are possible, which do not require discontinuation of the drug and resolve independently during treatment. The only contraindication to the use of Pimafucin is hypersensitivity to the components of the drug. Pimafucin can be prescribed during pregnancy and lactation, as well as newborns.
To treat intestinal candidiasis, a course of treatment with non-absorbable antifungal drugs is required for 710 days. Nystatin is prescribed 250,000 units 68 times a day (daily dose up to 3 million units) for 14 days. It is prescribed 100 mg (1 tablet) 2-4 times a day for 710 days [1].
Based on the above provisions and clinical experience, we have to admit that the tactics of treating candidiasis of the mucous membranes of extraintestinal localization only with local antifungal agents or systemic drugs absorbed from the gastrointestinal tract are inherently erroneous. Since the source of lymphohematogenous spread of virulent Candida strains that cause systemic candidiasis is the intestine, without suppressing the growth of fungi in its lumen, antifungal therapy is ineffective or only a short-term unstable effect is observed. For systemic candidiasis, the dose of nystatin can be increased to 46 million units/day, while a locally active antifungal agent is prescribed. For systemic candidiasis, Pimafucin is used in the same dose while simultaneously prescribing a locally active antifungal agent. In severe cases, drugs with systemic action are added to complex therapy [1,5].
Timely recognition and treatment of intestinal candidiasis is especially important as a prevention of systemic and generalized candidiasis in patients at risk, which primarily include patients receiving antitumor radiation and/or chemotherapy, anti-tuberculosis drugs, and patients preparing for planned operations on the abdominal organs. In these situations, it is most preferable to prescribe non-absorbable antifungal drugs, since their long-term and repeated use does not significantly affect the pharmacodynamics of other drugs.
The main criterion for the effectiveness of therapy is not obtaining a negative culture result for fungi, but, first of all, the disappearance of the main manifestations of the disease, normalization of the number of fungi according to mycological research (if adequate culture of intestinal contents is possible). To achieve an effect, it is often necessary to resort to repeated courses of treatment [1].
This article aimed to expand the understanding of practitioners about the flexibility of interaction between the human body and symbiont microflora, and about the pathogenic potential that the harmless intestinal commensal Candida has. Internists and specialists in medical mycology are faced with the urgent tasks of clearly determining the prevalence and clinical significance of fungal infections in clinical practice, developing a diagnostic algorithm and indications for treatment of intestinal candidiasis.
Literature:
1. Zlatkina A.R., Isakov V.A., Ivanikov I.O. Intestinal candidiasis as a new problem in gastroenterology. // Russian Journal of Gastroenterology, Hepatology, Coloproctology. 2001. No. 6. P.3338.
2. Danna PL, Urban C., Bellin E., Rahal JJ Role of Candida in the pathogenesis of antibiotic-associated diarrhoea in elderly patients.//Lancet/1991.Vol.337.P.511514.
3. Prescott RJ, Harris M., Banerjee SS Fungal infections of small and large intestine.//J.clin.Path.1992.Vol.45.P.806811.
4. Redmond HP, Shou J, Kelly CJ et al. Proteincalorie malnutrition impairs host defense against Candida albicans.//J.Surg.Res.1991.Vol.50.P.552559.
5. The Merck Manual. Sixteenth edition. Copyright (c) 1992 by Merck&Co., Inc.
Published with permission from the administration of the Russian Medical Journal.
Disease prevention
Preventive measures are aimed at improving the condition of the microflora. These include:
- Proper oral hygiene.
- A thoughtful diet with a high amount of protein foods and reduced consumption of foods containing glucose.
- Quitting smoking and alcoholic beverages.
- Timely examination by the attending dentist for the prevention, diagnosis and treatment of the disease.
- Avoid taking medications, such as antibiotics, without first consulting your doctor.
- If the patient has dentures, then one of the preventive measures will be their regular treatment in a special solution.
Sources:
- The role of anti-inflammatory rinse in the treatment of periodontal diseases (L.Yu. Orekhova, A.A. Leontyev, S.B. Ulitovsky) L.Yu. OREKHOVA, Doctor of Medical Sciences, Prof., Head of Department; A.A. LEONTIEV, dentist; S.B. ULITOVSKY, Doctor of Medical Sciences, Prof. Department of Therapeutic Dentistry of St. Petersburg State Medical University named after. acad. I. P. Pavlova
- Report on clinical trials to determine/confirm the preventive properties of commercially produced personal oral hygiene products: mouth rinse "ASEPTA PARODONTAL" - Solution for irrigator." Doctor of Medical Sciences Professor, Honored Doctor of the Russian Federation, Head. Department of Preventive Dentistry S.B. Ulitovsky, doctor-researcher A.A. Leontiev First St. Petersburg State Medical University named after academician I.P. Pavlova, Department of Preventive Dentistry.
- Study of the clinical effectiveness of treatment and prophylactic agents of the Asepta line in the treatment of inflammatory periodontal diseases (A.I. Grudyanov, I.Yu. Aleksandrovskaya, V.Yu. Korzunina) A.I. GRUDYANOV, Doctor of Medical Sciences, Prof., Head of Department I.Yu. ALEXANDROVSKAYA, Ph.D. V.Yu. KORZUNINA, asp. Department of Periodontology, Central Research Institute of Dentistry and Maxillofacial Surgery, Rosmedtekhnologii, Moscow
Products that regulate bowel function
Various intestinal diseases can be accompanied by different and sometimes even opposite symptoms. For example, a person may suffer from diarrhea or, conversely, suffer from constipation. You can improve intestinal function with the help of certain diets and eating foods that have a laxative effect or weaken intestinal function.
To natural “ laxatives”
” include dried fruits, kefir, legumes, oatmeal and buckwheat.
They are recommended for use by people suffering from periodic constipation, even if it is not caused by intestinal diseases.
Mashed porridges, slimy soups, and foods high in tannin help the stomach work
Reviews and results
A diet for candidiasis is really necessary, as many reviews confirm. If you adhere to such a diet constantly, there will never be exacerbations of candidiasis. At the same time, maintaining immunity and avoiding stress is of no small importance. Many note that it is difficult to adhere to it due to the lack of sweets and therefore frequent “breakdowns” occur, which in some cases nullifies the treatment.
- “... My husband has been living with candidiasis for six years. She has been taking antiretroviral therapy for a year and a half, and loading doses of fluconazole several times a year, and for prevention, 150 mg every week. The hardest thing is to follow a diet. He tries to follow the nutritional recommendations and I must say that it has become easier - there are fewer manifestations in the mouth and there is no diarrhea. For company with him, I have to eat like this”;
- “... I came to the conclusion that diet is an effective treatment. It is enough to completely give up sugar, confectionery and starch - the effect is felt after the first week. I had intestinal candidiasis after taking antibiotics, but not severe. After the examination, the doctor said that I could try to improve everything with a diet and probiotics, and I would always have time to take the pills. That’s how it all happened: after three days the bloating stopped, and after a week the stool returned to normal”;
- “... I was diagnosed with this, and I began to eat properly during the treatment. Additionally, I introduced garlic, barberry, cloves, and cinnamon. It turned out that eating is good not only for health, but also for weight loss. Of course, if you remove bread, all pastries and sweets. I lost 7 kg in 3 months and my intestines improved. I also drank Narine for good flora. Of course, the diet is strict, but it’s worth it.”