Jaw cancer is a malignant neoplasm that affects bone tissue. The disease has no age restrictions; it is characterized by rapid growth, metastasis, and pronounced pain. The structural features of the maxillofacial region, proximity to important vessels and nerve centers further complicate treatment.
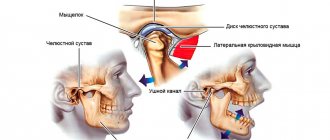
Anatomical structure
The oral cavity is the initial section of the digestive tract, in which food is chewed and saliva is produced to digest food. It is involved in the process of breathing, swallowing, articulation and speech.
The composition of the oral cavity includes:
- vestibule (lips, front side of teeth, inner surface of cheeks);
- gums;
- the bottom on which the tongue lies;
- two thirds of the tongue;
- teeth;
- retromolar triangle - the space on the lower jaw behind the third molar;
- hard and soft palate.
Detection of pathology
Detection of tumors of the lower jaw is based on a thorough study of the course of the disease, as well as morphological and radiological data. The diagnosis is made by x-ray, since x-rays can detect destructive changes in the bone early.
In the initial stages of sarcoma or jaw cancer, x-rays show bone loss. Its changed area does not have clearly defined boundaries; they are blurred. If jaw cancer is localized in the area of the alveoli, then the cortical plates of its walls are destroyed, and an extensive zone of destruction of the spongy substance is visible around the circumference. If the process has spread, then the radiograph shows complete destruction of a certain part of the bone.
Histological analysis of the tissues of the surface of the extracted tooth during its mobility is informative. It is always necessary to strive to establish the cause of loose teeth. If the mucous membranes of the mouth have ulcerations and the area is clearly visible, a cytological analysis of the mucosa is performed to confirm the diagnosis.
Classification
Oral cancer is divided into three types:
- papillary. The nodule in the mucous membrane increases in size and hangs into the oral cavity. The neoplasm progresses slowly;
- infiltrative. The seal on the pinkish mucosa is distinguished by a whitish color, clear contours and shape, and thinning of the membrane around it. On palpation from the side of the cheek, a dense infiltrate is felt. The tumor tends to grow rapidly. The patient complains of unbearable pain;
- ulcerative The most common form of the disease. Ulcers on the mucous membrane do not heal, they grow, and the border around them turns red. The outline is torn and its edges are bleeding.
Tumor metastases appear quickly. Malignant cells grow into the mental, submandibular, and deep jugular lymph nodes. This process is influenced by the thickness and depth of the tumor. Thus, when the tumor deepens by 4-5 mm, metastases occur in 98% of cases. At the T1 stage of oncology, metastasis is detected in half of the cases, and when the T4 stage is reached, distant spread of cancer cells is observed in 85% of cases.
After operation
Communication after tracheostomy
If you have had a tracheostomy, you may not be able to speak when you first wake up after surgery, but you will be able to communicate in writing. The nurse will give you a pencil and paper. You can also answer yes or no questions by nodding or shaking your head. You may also be given a tablet to facilitate communication. The tablet comes with an app to help you communicate your needs. Your nurse will teach you how to use the tablet.
Compression boots
You will be wearing compression boots while you are in bed. These boots put gentle pressure on your calves, which prevents blood clots. They will be removed when you are able to get out of bed and walk. If you have surgery without a free flap, you will be able to get out of bed and walk the day after surgery. If a free flap was used during surgery, this will occur somewhat later, depending on the location of the free flap. Every day your physical activity will increase.
Nutritional tube
If you find it too difficult to eat and drink, you may have a feeding tube placed after surgery. Depending on the surgery, you may be unable to eat for a week after surgery. Your healthcare provider will provide you with more information.
Anesthesia
You will experience pain after surgery. Be sure to ask your nurse for painkillers. You may initially receive it through an intravenous (IV) drip. Later, you may take medications by mouth (by mouth) or through a feeding tube if you have one. As you heal, you will need less pain medication.
Drainage tubes
If lymph nodes in the neck are removed, drainage tubes will be placed in the neck. You may also have them installed in the area of the free flap, if one was used. Drainage tubes are usually removed when the amount of discharge decreases. Most likely, all of these tubes will be removed before you are discharged from the hospital. If you are discharged from the hospital with tubes in place, your nurse will teach you how to care for them. For more information, read the pre-surgery guide About Neck Dissection Surgery.
Oral hygiene
Your nurse will teach you how to use the oral irrigation and care kit. This kit will help keep your mouth clean and speed up healing. After you leave the hospital, you will need to rinse your mouth with an irrigation kit. It is especially important to rinse your mouth after eating. After you eat, there should be no food particles left in your mouth. For more information, see Oral Irrigation
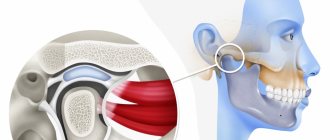
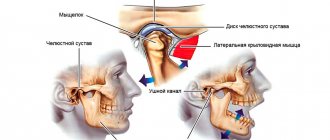
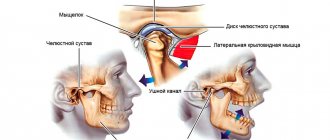
How to prevent spasms of the masticatory muscles
Spasm of the masticatory muscles is the inability to open the mouth. During recovery after surgery, it is very important to prevent spasm of the masticatory muscles. Your nurse will teach you exercises to help prevent this side effect, which are described in How to Prevent Masseter Muscle Spasms.
to come back to the beginning
Causes
The prevalence of oral cancer is growing and is currently diagnosed in 2% of patients among the total number of cases. Since 2009, the incidence has increased by 25%, with mostly squamous cell carcinoma being detected and only in isolated cases adenocarcinoma.
Most foci of oncology are observed in the tongue. Slightly less malignant formations on the floor of the mouth. Cancer of the soft and hard palate, gums and cheeks is detected in 20% of cases. Much less frequently diagnosed is damage to the alveoli of the lower jaw - 4%, the arches of the palate, retromolar region and vestibule - 3%.
Based on practice, men are more susceptible to oral cancer than women. This is due to bad habits, for example, the abuse of cigarettes or chewing tonic mixtures increases the production of saliva, which washes away beneficial elements from the mucous membrane. The risk group includes patients with HPV, elderly people, workers in hazardous industries, patients with lichen planus, people whose oral mucosa is systematically injured by fillings, prostheses, and metal objects.
Forecast criteria
The survival rate of patients with maxillary sinus cancer averages about 40% over 5 years.
At an early stage, when treated in European oncology clinics, tumors have a cure rate of up to 80%.
Patients with unresectable tumors treated with radiation had a survival rate of less than 20%. Survival rates have now improved slightly due to advances in skull base surgery.
In patients with squamous cell carcinoma of the nasal cavity or maxillary sinus, better survival outcomes are achieved when patients receive adjuvant radiation therapy, adjuvant chemoradiotherapy, or neoadjuvant therapy in addition to surgery.
In patients with sinonasal adenocarcinoma, better disease-free survival was associated with surgery followed by radiation therapy compared with surgery alone, for all tumor stages (T1-T4).
Symptoms
A malignant ulcer from ordinary stomatitis in the mouth can be identified by swelling and swelling of the cheeks, pain and constant discomfort even at rest. You should be wary of prolonged non-healing of the wound and its bleeding.
As the disease progresses, the symptoms intensify:
- swelling increases and spreads to the neck;
- the red or white spot on the oral mucosa intensifies;
- discomfort when chewing and swallowing;
- difficulty speaking due to friction of the mucous membrane on the teeth when moving the jaw;
- the appearance of bad breath;
- feeling of a foreign object in the throat;
- anemia of the mouth.
In the late stages of cancer, teeth fall out and body weight rapidly decreases.
Discharge after surgery
Your surgeon will tell you when you can return to work and normal activities. It depends on the surgery you underwent and the speed of recovery.
In most cases, patients can cope with daily activities at home without additional help, but the nurse will discuss this with you before leaving the hospital. If you need help, your nurse or case manager can help arrange visits from a visiting nurse or home health professional.
Call your healthcare provider if you have any of these signs or symptoms of infection:
- temperature 101°F (38.3°C) or higher;
- increased redness around the incisions;
- increased discharge from the incisions;
- discharge that has an unpleasant odor;
- increased pain that does not go away after taking a prescribed pain reliever or acetaminophen (Tylenol®).
to come back to the beginning
Diagnostics
At the initial consultation, the doctor examines the oral cavity, examines ulcers, erosions, damage to the mucous membrane, and then takes a smear for examination. To confirm the inflammatory process, the patient is sent for a general and biochemical blood test.
The diagnosis is confirmed by the results of the examination:
- MRI and ultrasound of soft tissues of the neck. The images reveal the localization of the pathology, the depth of germination and the structure of the tumor, compaction from blood and lymph, decomposition of the cortical layer of the bone;
- if metastases are suspected, a fine needle aspiration biopsy of the lymph nodes under the chin, under the jaw and in the upper third of the neck is performed;
- positron emission tomography. Shows the depth of the tumor, as well as early metastases;
- osteoscintigraphy. Skeletal bones are examined to look for displaced cancer cells;
- CT scan of facial bones with contrast. The images show the tumor growing into the neck vessels, jaw or base of the skull.
Metastasis
The process of metastasis of pathology occurs through the lymphogenous route. Most often, metastases are observed in the submandibular zone and fuse with the lower jaw quite early, after which they infiltrate the skin.
If jaw cancer is in an advanced form, then metastasis to the spine, liver and other distant organs is noted. But often metastasis to the cervical lymph nodes and distant organs is not present. In the case of sarcoma of the lower jaw, metastasis to distant organs rarely occurs, and they, as a rule, do not form in regional lymph nodes.
Secondary (metastatic) tumor formations are detected much less frequently compared to primary ones, and they are more often observed in women. Pathological metastases occur in lung, breast, thyroid, and stomach cancer.
In case of metastases, they are resected together with excision of the cervical tissue: if there is one metastasis in the submandibular region, then an upper fascial-sheath excision of the neck tissue is performed on one side; if metastases are present at the site of the branching of the common carotid artery, then a Krail operation is performed, if necessary, fascial-sheath excision cervical tissue.
Treatment
The choice of treatment tactics depends on the stage and extent of the tumor. When the tumor grows rapidly, treatment methods are combined.
Operation
The doctor determines the principle of surgical intervention after determining the stage of the tumor and its spread. If cancer cells have penetrated the periosteum and surrounding tissues, a wedge-shaped, planar or sagittal resection of the jaw is performed. If the examination reveals the growth of cancer cells directly into the bone or the defect is noticed during surgery, segmental resection of the lower jaw is performed. The doctor assesses the lesion on site and determines the thickness of the excised layer.
The next stage of the operation is partial or complete excision of the cervical lymph nodes to prevent metastases if the thickness of the tumor is more than 4 mm or the location of the tumor in the floor of the mouth or on the tongue. If the tumor is located in the midline, then the cervical lymph nodes are excised on both sides. The operation ends with the immediate replacement of damaged tissue.
After removal, the tumor is sent for histological examination. Its size, thickness, depth, edges are assessed. Further treatment is affected by cell growth beyond the boundaries of the capsule of the removed lymph node, and the spread of cancer cells to neighboring organs.
Radiation therapy
Radiation after surgery is prescribed when diagnosing T3, T4, N2, T3 stages of the disease no later than six weeks after tumor removal. The need for radiation therapy increases with perineural invasion of the lymphatic vessels. The total focal dose for all sessions is 60 g, and the single focal dose for one session is 2 g. When metastases are detected on the neck, the SOD increases to 66 g, and if there is no risk of metastasis, the SOD decreases to 50 g.
As the main treatment, radiation therapy is used in a total focal dose of 60-70 g. The procedure is performed five days a week and is combined with chemotherapy. Every three weeks, 100 mg of cisplatin is administered.
Chemotherapy
Anticancer drugs are prescribed before surgery or along with radiation therapy to reduce the size of the tumor. Sometimes therapy is prescribed simultaneously with surgery.
Treatment involves the use of a 5-fluoroacyl regimen together with cisplatin or other agents - carboplatin, methotrexate, bleomycin. They cause a number of side effects, for example, vomiting or nausea, hair loss, decreased appetite, and increased bleeding. Symptoms disappear after treatment, but permanent hearing loss is sometimes observed after taking cisplatin.
The prognosis of oral cancer depends on the stage at which the disease is detected. If treatment is started at stage zero, the disease will stop. It is worth noting that smoking provokes relapse or degeneration of the tumor, so repeated surgery or radiation may be required. Surgery at the first stage increases survival rate to 80-85%, and the combination of radiation therapy with surgery at the second stage by 60-80%. Already at subsequent stages of cancer development, the survival rate is no more than 50%, and all three treatment methods are used simultaneously.
Dispensary observation
Since the tumor can recur and metastasize, after completing the course of treatment the patient is registered with the oncology clinic. The first year you should visit a doctor every month, the second year a preventive examination is carried out every 4-6 months, and then once a year or in case of any ailments. The examination involves an examination - ultrasound and contrast MRI of the soft tissues of the neck, PET, osteoscintigraphy. Consultation with an otolaryngologist, dentist and oncologist is required. The doctor may shorten the period of medical examination if there is a high risk of relapse.
List of references on the topic:
- Gantsev Sh.H. Oncology – M, 2012 – P.204-205.
- Golovin D.I. Errors and difficulties in diagnosing tumors, D.: Medicine. Leningr. department, 2015 305 pp.
- Selected lectures on clinical oncology/Ed. IN AND. Chissova, S.L. Daryalova. – M., 2010
- Matyakin E.G., Alferov V.S. Chemotherapy of head and neck tumors // Mat. 2nd Ros. oncol. conf. “Current trends in the development of drug therapy for tumors” December 8–10, 2016 – M., 256 p.
- Tumors of the head and neck: hands/ A.I. Paches. - 5th ed., add. And revised - M.: Practical Medicine, 2013. -478 p.
- Shine A.A. Oncology. M – 2014 365 pp.
- Encyclopedia of Clinical Oncology/Ed. M.I. Davydova. – M., 2014 –P.140-179.
- Bityutsky P.G., Kitsmanyuk Z.D., Trofimov E.I. Diagnosis and treatment of cancer of the oral mucosa // Medical consultations. - 2014. - No. 1. - P. 23-27.
- Byakhov M. Yu. Options for combined and complex treatment of locally advanced cancer of the oral mucosa and oropharynx: Dis. Dr. med. Sci. - M., 2013.