Periocoronaritis is a dental disease characterized by inflammatory processes in the soft gum tissues that surround the erupting units (in the vast majority of cases, wisdom teeth). It manifests itself as intense pain, the inability to open the mouth normally, swelling of the gums, as well as an unpleasant odor from the oral cavity. Inflammation develops from the accumulation of plaque in the opening of the gum through which the unit erupts, or due to the difficulty of the process itself. The latter causes pressure on the adjacent unit along with damage to the bone and gum tissue.
The CELT Surgical Department of Dentistry invites you to undergo treatment for pericoronitis in Moscow. Our multidisciplinary clinic has been operating in the paid medical services market for more than two decades and enjoys a good reputation among patients. We have all the necessary certificates and licenses and provide treatment with the conclusion of an official contract and provision of a guarantee. You can find out the price of excision of the hood for periocoronitis or removal of a wisdom tooth by going to the “Services and Prices” section.
Consultation with a dentist-therapist - 1,000 rubles.
Treatment of pericoronitis with medication - 1,000 rubles.
Surgical treatment of pericoronitis (excision) - 2,500 rubles.
At CELT you can get advice from a dental specialist.
- The cost of a dental consultation is 1,000
Make an appointment
Etiology of pericoronitis
Most often (in more than 90% of cases), this disease is provoked by wisdom teeth, which begin to develop on the bulky area of the gums, which is located behind the third molars. The reasons for pericoronitis in this case lie in the fact that the width of the dental arch in modern humans has decreased by ten to twelve millimeters, but the teeth have retained their previous sizes. As a result, there is a lack of space for the eruption of units, which makes it difficult and manifests itself as inflammation.
Another reason lies in the too thick walls of the dental sac around the dental crown and gum mucosa, which also seriously complicate the teething of units. The reduction in growth-forming factors should not be discounted. During tooth growth, its position does not change, but part of its surface is hidden under the mucosa - and it is there that food fragments, pathogens and dental plaque begin to accumulate. Together, they create an ideal environment for the development of specific inflammatory processes, which are maintained due to regular trauma to other teeth during chewing. The result is scarring and an increase in the periodontal gap.
It is worth highlighting separately the factors that contribute to the development of dental periocoronaritis:
- early loss of primary teeth;
- malocclusion;
- abnormal increase in units – macrodentia;
- their complete or partial absence is adentia.
Symptoms of pericoronitis
All of the above factors negatively affect the development and eruption of wisdom teeth, but at the same time, pericoronitis itself is caused by the activity of bacteria that accumulate in the resulting gingival fold. As for the symptoms of the disease, until the wisdom tooth begins to actively erupt, the patient does not feel any concern, however, when performing an orthopantonogram, the risk of pathology can often be predicted. At more advanced stages, wisdom tooth pericoronitis has quite obvious symptoms:
- itching in the area of the wisdom tooth (in the early stages);
- swelling, redness, pain;
- formation of a gingival hood;
- elevated temperature;
- enlarged lymph nodes;
- abscesses, purulent discharge, unpleasant odor.
Symptoms of periocoronaritis
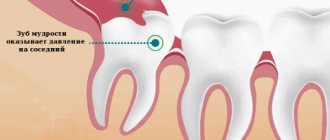
The disease is characterized by intense pain symptoms localized in the area of the unit. Often it radiates to the temporal or ear region. The patient suffers from the inability to chew and swallow food normally, and even to open his mouth normally. As the inflammatory processes develop, they cover the surrounding tissues: pain is most often caused by the involvement of the gum hood, less often by the incorrect position of the growing units. If they are located at an angle, damage to the gum and bone tissue occurs, and there may also be pressure on the adjacent tooth, which often leads to its destruction.
Pericoronitis of the wisdom tooth also manifests itself:
- increased temperature in the affected area, sometimes in the whole body;
- enlargement of regional lymph nodes;
- the appearance of halitosis;
- unpleasant aftertaste when consuming food.
The lack of adequate treatment leads to the development of a purulent focus in the maxillofacial area of the face. The patient constantly secretes pus, the pain intensifies even at rest, and complications of pericoronitis develop, such as purulent melting of the subcutaneous tissue (phlegmon) or osteomyelitis.
Symptoms
The disease is quite pronounced, so it is difficult not to notice it.
- The earliest sign is swelling , redness and a significant increase in the size of the gum tissue. These symptoms may be so severe that they make it difficult to open your mouth. The area of edema can involve not only the affected gum, but also neighboring areas, including the cheeks.
- The next clear sign is pain - sharp, radiating to the ear and temple area, as well as to neighboring areas of the jaw. The pain intensifies when pressing on the affected area, when chewing, brushing teeth, or talking. Often the pain can become so intense that the patient cannot open his mouth.
- Over time, another symptom appears - bad breath , sour taste. Even regular brushing of teeth and the use of rinses and chewing gums does not help get rid of these sensations, since the source of the odor is located under the gum hood, and it is impossible to remove it from there with ordinary means. Smell and taste may occur even at the initial stage of the disease.
- Upon palpation, enlarged submandibular lymph nodes on the affected side are noticeable. As the process spreads, other groups may become involved. The patient's general condition gradually worsens, the temperature may rise, and general intoxication syndrome may develop.
Classification of pericoronitis
Based on the shape of the flow, they are distinguished:
- Acute pericoronitis is typical for the primary manifestation of inflammation, and in the future, in the absence of treatment, for exacerbations of the chronic form;
- Chronic pericoronitis - characterized by repeated inflammatory changes in the mucosa around the erupting unit.
Depending on the clinical form of soft tissue inflammation, the following are distinguished:
- • Purulent pericoronitis in acute form – manifests itself with intense pain symptoms, deterioration of the general condition and an increase in temperature up to 30°C. Upon palpation, the doctor detects an increase in the submandibular lymph nodes. There is swelling of the mucous membrane in the area of the hood, cheeks and soft palate, pus flows from under the hood;
- Acute catarrhal pericoronitis - manifested by pain during chewing, body temperature remains within normal limits (as well as the tissues around the jaw do not swell), the patient can open his mouth normally. At the same time, the hood looks swollen, the entire crown of the tooth is under it, and exudate flows out from under it.
Classification
Pericoronitis is divided into acute, which occurs most often, and a rarer form - chronic pericoronitis. Despite the fact that the latter type is not reflected in ICD-10, it occurs with improper treatment of pericoronitis.
According to the flow, the following types of pericoronitis are distinguished:
- Catarrhal – characterized by slight swelling and pain when touched;
- Purulent - constant pain and the presence of purulent discharge;
- Ulcerative – leads to the formation of ulcerative defects on the gums;
Retromolar is distinguished as a separate form - it is distinguished by its location, which does not allow it to be easily seen and treated, which makes it difficult to combat this disease and increases the likelihood of complications.
Diagnosis of pericoronitis
The diagnosis is made by the dentist after an examination, taking into account the patient’s symptoms and complaints. In order to determine the direction of growth of the unit, an x-ray examination is often required. The main task of the doctor is to determine the form of the disease, its prevalence, nature and severity. In addition, he must identify contraindications to treatment:
- individual intolerance to medications or materials used in it;
- the presence of concomitant pathologies that will complicate treatment;
- inflammation of the tissues and organs of the oral cavity.
Types of pericoronitis
| Type of pericoronitis | Description |
| Catarrhal | The initial form of the disease, in which the inflammatory process has just begun, and the gingival hood has not yet formed. |
| Ulcerative | Noticeable swelling, formation of ulcerative rims, bleeding of the gums in the affected area. |
| Acute pericoronitis | An acute form of the disease, rapidly developing and progressing to more severe stages. |
| Retromolar | Deep inflammation affecting the periosteum and going deep. Visually expressed by severe swelling. |
| Chronic purulent | It affects soft and hard tissues in the area of the wisdom tooth, as well as neighboring parts of the jaw. At this stage, the risk of developing phlegmon and osteomelitis is highest. |
How to treat pericoronitis?
Treatment tactics for pericoronitis are selected by CELT dentists on an individual basis, depending on the diagnostic results and the patient’s indications. It is aimed at:
- pain relief;
- relief of inflammatory processes;
- restoration of the functionality of the dental system;
- excluding the development of complications.
Therapeutic manipulations are carried out on an outpatient basis, taking into account the severity of inflammatory processes, the local and general picture of the pathology and radiographic data. Treatment of the catarrhal form of acute periocoronaritis involves:
- antiseptic treatment of the area under the hood;
- application of antiseptic and anesthetic dressings;
- lifting the hood using a gauze strip soaked in iodine solution.
Pericoronitis
- Caries
- Pulpitis
- Gingivitis
- Periodontitis
- Periodontal disease
- Periodontitis
- Pericoronitis
- Peri-implantitis
- Fluorosis
- Stomatitis
- Tooth cyst
- Pericoronitis
- Treatment
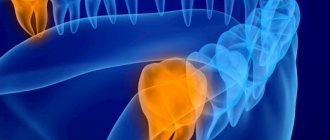
Pericoronitis is the occurrence of inflammation in the marginal part of the gums and periodontal tissue of an erupting tooth. The inflammatory process can cause the eruption of any tooth, but as clinical experience shows, pericoronitis is typical specifically for third molars (wisdom teeth).
Factors of occurrence
The reasons include:
- Formation of a favorable environment for the life of bacteria due to the presence of a recess for the accumulation of food debris formed by the gum tissue above the distal cusps of the erupted molar.
- Development of damage to the mucous membrane in the form of superficial erosions or ulcers.
- Injury to the tissue fold remaining over part of the tooth (for example, hard food).
- Difficulty cutting.
In turn, the reasons for difficult teething may be:
- increased bone density of the alveolar process of the wisdom tooth due to the fact that there was no baby tooth in this area;
- insufficient space for the development of the third molar due to the specific structure of the jaw of modern humans;
- thickening of the mucous membrane over the posterior teeth of the jaw due to the addition of its structure with fibers of the muscle tissue of the cheek and the upper constrictor of the pharynx.
As a result of the influence of these factors, there is a delay in the development of third molars.
Clinical picture
The onset of inflammation is signaled by aching pain in the soft tissues of the affected tooth. Within three days it intensifies. Pain appears when chewing food on the side where the inflammation is located, sometimes when swallowing and opening the mouth. The tissue fold, partially covering the eighth tooth, gradually swells. Touching it provokes shooting pain, radiating to the temple or auricle area. Symptoms are especially acute when the third molar grows at an angle.
The condition of the body as a whole is satisfactory: the temperature may be elevated, but not more than 37.5 degrees, lymphadenitis under the lower jaw is observed, and, less often, a headache. As the disease progresses, purulent exudate is released from the lesion, which is the source of bad breath.
If the patient has endured and ignored treatment for pericoronitis in the acute form, the severity of symptoms may decrease, which indicates the transition of the disease to the chronic stage. The presence of an open outlet for purulent accumulation ensures a quiet course of the disease, falsely reassuring the patient. In reality, the infection gradually spreads to neighboring tissues. This process can be expressed in the form of an abscess or phlegmon. The area of mucosal hyperemia expands to the buccal region and the lingual-palatal arch. In addition, with prolonged inflammation, bone tissue begins to undergo resorption, and when pus penetrates it, osteomyelitis occurs. Deformation of the gum tissue can lead to blocking of purulent outflow, which will be reflected in an exacerbation of the inflammatory process.
The most striking manifestation of pericoronitis will be the formation of ulcers along the edge of the gingival fold, resulting in necrosis of this part of the tissue. Ulceration occurs when the gums become infected with fusospirochetes. A complication may be an ulcerative form of gingivitis or stomatitis.
Surgical methods of treatment
Treatment of pericoronitis is almost always surgical. And if we talk about molars and premolars, dentists choose the tactic of excision of the gingival hood. But treatment in the area of eights is almost always performed by removing wisdom teeth, and further we will explain why.
Excision of the gingival hood opens access to the growing tooth; this measure allows not only to remove excess inflamed tissue and thoroughly rinse the area, but also to help the tooth erupt completely and take its correct place in the dentition. This method has several conditions or indications:
- integrity of the crown and root system of the erupting tooth;
- correct location of the tooth in the bone tissue of the jaw;
- availability of sufficient space for complete tooth eruption in the row.
That is, this approach is used in all cases where the gums are the only obstacle to normal tooth eruption. If a unit of the dentition is not very healthy, for example, caries is observed, the integrity of the crown is compromised, or there are diseases of the root system, then the decision is made individually. If it is advisable to preserve the tooth, the doctor will also perform an intervention and take measures to eliminate the pathology.
Impacted and dystopic teeth, as well as situations in which complete tooth eruption will inevitably lead to malocclusion or displacement of adjacent teeth are indications for a different type of surgical treatment. The doctor may suggest tooth extraction, and in cases of disease above the “eight” level, this is almost always the only option to solve the problem.
The fact is that wisdom teeth do not bear a functional load, very often erupt at an angle, interfere with neighboring teeth and increase the risk of complications, including bite defects. Therefore, it is considered appropriate to remove the “eight” and further measures to eliminate inflammation in the soft tissues.
The only exceptions are cases when the “eight” could potentially be used as a support for a prosthesis or be important in planned orthodontic treatment.
In general, the following cases and features are indications for removal of both the hood and the tooth:
- excision of the hood has already been performed previously, but the inflammation has not gone away and/or has intensified, there is no effect from the treatment;
- the tooth does not have enough space in the dentition;
- impacted, dystopic tooth, the preservation of which jeopardizes the health of neighboring teeth and the oral cavity;
- the gingival hood grows over the erupting tooth again (this rarely happens);
- the tooth is affected by caries/destroyed, its treatment and preservation are impractical.
Since it requires the removal of a tooth that has not yet fully erupted, the procedure is considered a complex extraction. Most often, it requires preliminary dissection of the gums and extraction of the tooth from deep-lying tissues. Therefore, in many cases, sutures will be required on the gums, which will speed up tissue healing.
Surgical treatment of pericoronitis is performed under local anesthesia, so the procedure will not cause discomfort. An obligatory step is washing the mucous membrane with antiseptic solutions.
Removal of tissue hanging over the tooth can be done with conventional instruments or a laser.
Diagnostics
Diagnosis is carried out exclusively by dental specialists based on the examination data provided, including, if necessary, the results of fluoroscopic examinations. Based on the examination data, a clinical picture is drawn up. It serves as the basis for prescriptions for treatment aimed at preventing the possibility of complications. The method of treatment depends primarily on the general condition of the patient, as well as on the nuances and characteristics of the course of the inflammatory process.
Pericoronitis, treatment in children and adults
It should be noted right away that for pericoronitis, treatment at home can only reduce the symptoms of inflammation, but not solve the problem. Therefore, all home methods (rinsing with antiseptics, applying anti-inflammatory ointments, etc.) can only be used as a way to relieve inflammation during the eruption of wisdom teeth and reduce pain - this is a temporary measure before visiting the dentist.
In a dental clinic, in case of complicated teething, treatment will depend on whether the problem tooth should be preserved or whether it should be removed. If preserved, the doctor performs surgical excision of the “hood” under local anesthesia. This eliminates conditions for the accumulation of food and the growth of bacteria, and also facilitates teething. After excision of the “hood,” the patient is prescribed antiseptic therapy (rinses, baths) and, if necessary, antibiotic therapy.
In cases where tooth extraction is indicated due to their incorrect position on the jaw, lack of antagonists, or insufficient space for full eruption, the doctor immediately removes the problematic tooth and prescribes antiseptic therapy to the patient.
In some cases, at the initial stages of the inflammatory process, conservative therapy can be preliminarily applied - local treatment with antiseptic rinses and the introduction of an iodoform tampon into the “hood”. However, local therapy does not always give a positive result; moreover, it is appropriate only at the initial stage of the disease; in other cases, surgical intervention will be required.
When it comes to teething in children, treatment is always aimed at preserving the teeth (except for those cases when dystopia is clearly expressed and the doctor sees that preserving is useless).
Laser treatment
Laser excision of the hood provides better results. The main advantages include:
- lower risk of inflammatory complications, including secondary wound infection;
- coagulating effect of the laser - no risk of bleeding;
- short recovery period;
- reduction of pain after intervention;
- no need to additionally treat intervention areas with turundas and antiseptics.
There are few contraindications for laser intervention, one of them being cancer.
Classification, ICD-10 code, reasons
According to the International Classification of Diseases, 10th Revision (ICD-10), pericoronitis is classified as an impacted or impacted unit. In the first case, the tooth changes its position in the row as it erupts, but there is no obstacle from the neighboring unit. In the second, the change in the position of the unit being cut through is directly related to the collision from the neighboring one.
The most common cause of the condition in question is the incorrect location of the “wisdom tooth” - parallel to the growth line of the row units, and this is what prevents it from taking the correct place. The second possible cause of pericoronitis is incomplete eruption (partial), when the rudiment of the unit is in the bone.
There are several types of condition:
- catarrhal - it all begins with swelling of the soft tissues and their redness, itching and slight pain, burning sensation, tingling;
- ulcerative - the surface of the inflamed gums becomes covered with small ulcers with a whitish coating, tissue necrosis is possible;
- purulent - the pathological process is accompanied by the appearance of serous and then purulent fluid, the pain syndrome is pronounced, characterized by “pulsation”, and a foul odor emanates from the mouth.
The listed types refer to acute pericoronitis. If there is no treatment, the acute form quickly transforms into chronic. The clinical picture becomes mild, but the purulent contents continue to increase, and a passage may form through which the pus flows into the oral cavity. Chronic pericoronitis is periodic relapses, constant intoxication of the body, increased body temperature and fever.
Complications of the disease
In the case when treatment of the gums during complicated tooth eruption was not carried out, serious complications of the inflammatory process develop:
- Periostitis, or flux, is inflammation of the periosteum.
- Osteomyelitis - in this disease, inflammation affects both the bone tissue itself and the bone marrow, gradually leading to bone resorption. This can cause abnormal jaw fractures.
- An abscess when the infection spreads to nearby tissues. Purulent inflammation leads to the melting of muscles and fatty tissues with the formation of a large accumulation of pus.
- Cellulitis is the next stage of a purulent process after an abscess, which does not have clear boundaries. Such purulent inflammation is a serious threat to the patient and is treated in a maxillofacial hospital.
These complications are usually difficult to treat, require a serious systemic approach and can lead to irreversible consequences. Therefore, if a person suspects he has pericoronitis, treatment should begin without delay in order to prevent the condition from worsening. You need to be especially careful if gum inflammation occurs during teething in children, since the children's immune system is still immature, the body's resistance to infections is lower and the process quickly becomes more severe.
What are the possible complications?
Improper teething, accompanied by pericoronitis without treatment, can lead to the following serious complications:
- Formation of necrotic ulcers along the gingival margin. Subsequently, necrosis can spread to other tissues of the oral cavity;
- Damage to healthy neighboring teeth;
- Phlegmon of the perimaxillary spaces;
- Periostitis, which easily spreads to nearby areas;
- Osteomyelitis;
- Abscess formation.
Any of these pathologies can become life-threatening, so treatment of inflammation of the mucous membrane must be timely.
Treatment of pericoronitis is not difficult. A timely visit to the dentist and diagnostics will allow you to immediately carry out the correct treatment. For example, if a tooth initially erupts incorrectly, then removing it at the very beginning of the process will avoid further discomfort.
If for one reason or another it was not possible to visit a doctor on time, then you should come for a consultation when the first signs of inflammation appear. The purulent form is much more difficult to treat and causes more inconvenience. In addition, pus is the main cause of complications.
Excision of the hood over the wisdom tooth
If there is an acute period of the disease or it develops again, the doctor usually recommends a simple surgical operation - excision of the hood. This is the name given to the muco-subperiosteal flap, which partially covers the tooth. A pocket is formed under it, in which food debris accumulates. By rotting, they turn into a nutrient substrate for pathogens. The situation is aggravated by constant mechanical impact on the gums.
Careful excision of the hood over the wisdom tooth allows you to open the surface of the molar and eliminate the source of infection.
Procedure to complete:
- Primary elimination of inflammation with medications.
- Anesthesia (usually local) and excision of the hood with a surgical scalpel.
- Antiseptic treatment.
After excision of the mucous hood is completed, patients are advised to refrain from food and hot drinks for 1-2 hours, as they can cause pain and infection of the wound. To completely eliminate the consequences of the disease, the doctor prescribes anti-inflammatory drugs, rinses, and physiotherapeutic procedures.
Development of acute pericoronitis
Acute Pericoronitis is considered as a type of acute periodontitis with primary symptoms of damage to the gum tissue. Damaged tissues located above the crown of a growing tooth involve in the inflammatory process all areas of the gums located near the resulting lesion. This course of the process is most often observed during the growth and eruption of the third, less often, fourth large molars of the lower jaw.
As a reason, experts consider both the lack of space for the formation of new teeth due to the development of a short jaw, and the abnormal development of the dental crown itself, which has assumed an incorrect location in the dentition.
Prevention
In some cases, especially when it comes to inflammation of the gums during teething in children, preventive measures will help prevent the disease: careful regular oral hygiene, timely removal of tartar and soft deposits, visits to the dentist for diagnostic examinations at least once every six months.
If pericoronitis is caused by the anatomical features of the structure of the dental system and the lack of space for the lower “eights” on the dental arch, preventive measures will only smooth out the course of the inflammatory process (due to timely cleaning of the oral cavity from bacterial plaque and food particles that create favorable conditions for inflammation) and identify the problem in time (subject to regular dental examinations).