Alejandro Bertoldi Hepburn Professor, Associate Professor at the Department of Endodontics, School of Dentistry, University of Buenos Aires (Argentina)
INTRODUCTION
Restoring dental function after endodontic treatment using fiberglass pins (FRP) has a number of advantages. The best known of these is the mechanical behavior of the post under horizontal loads, similar to dentin. SWS, like dentin, has the ability to elastically deform, so during operation there are no significant areas of stress concentration in the root. (Baba N & Goodcare C, 2014) (Perdigao, J, 2016).
The root preparation under the SWS is regulated and controlled using canal expanders, which allows you to preserve maximum dentin while preparing the bed for the pin. (Bertoldi Hepburn A, 2011).
Both of these factors: the absence of stress concentration and reduced dentin loss increase the resistance of the root to fracture when using SWS.
Since the SWS is a ready-made pin, it is installed immediately after removal of the endodontic filling. This method allows you to protect the root canal from contamination in the intervals between treatment stages, as often happens when using other endodontic posts, for example, cast metal posts (MCMP). (Bertoldi Hepburn A, 2011).
When the SWS is installed correctly, there is no gap (gap) left between the endodontic filling and the apical part of the pin. Cracks often appear when using LKSHV. This is due to the fact that the production of LKSHV is carried out in several stages, which leads to deviations of varying degrees. The space between gutta-percha and the post can be colonized by bacteria that irritate periodontal tissues through insufficiently sealed areas of the root in the apical region or through open lateral branches of the root canal in the hole for the pin. (Perdigao J, 2016).
Since there is no need to take impressions to place the SWS, it makes it easier to use the rubber dam and seal the surgical area. The rubber dam does not allow contaminants to pass into the pin hole and over the sealed channel. (Goldfein J, 2013).
SDS also have an aesthetic advantage - a translucent structure close to the color of the tooth. This feature helps create a translucent tooth-colored core, which in turn helps achieve a natural-looking crown. (Baba N & Goodcare C, 2014).
SWS are not subject to corrosion, which leads to a change in the color of the dentin of the tooth root or stump and, thereby, affect the restoration of the crown. (Bertoldi Hepburn A, 2011).
SWS also has disadvantages, the most common of which are decementing with the pin falling out of the root canal and destruction of the pin. (Baba N & Goodcare C, 2014) It has been proven that prolapse of the SWS often occurs in those clinical cases where there is not enough friction between the pin and the walls of the pin hole. This is a common situation in the middle third of the length, if the root canal is wide and the volume of remaining crown tissue is small. In such situations, the SRS will not be able to adapt to the walls of the root canal and will lose mechanical retention. (Bertoldi Hepburn A, 2011) (Perdigao J, 2016) If only small remains of the crown are preserved, then sufficient ferrule effect will not be achieved. As a result, the forces acting on the crown will be concentrated on the pin and will cause frequent decementation of the pin-crown complex in the prepared root.
Attempts to solve this problem by bonding the post and dentin of the root canal with dental adhesives and polymer cements show unstable and, in some cases, unsuccessful results. There are many factors that make adhesion in the tooth root difficult for a pin: residues of gutta-percha and endodontic cement that interfere with the bonding process; changes in the dentin of the root canal (collagen degradation, clogging of dentinal tubules, etc.); high C-factor in the tooth root, which leads to stress with limited polymerization shrinkage and much more. (Ferrari M, 2008) (Bitter K et al 2006) (Bitter K et al 2013) (Kahnamouei MA et al 2012).
To ensure proper retention of the pin, it was proposed to achieve sliding friction between the SWS and the walls of the root canal. (Goracci, C 2005) (Ferrari M, 2012) (Manicardi CA et al, 2011) To achieve this, several clinical techniques are recommended: adding a composite or pieces of reinforced composite strips to the pin to make it a customized or modified one for the individual anatomy of the UPS, the use of additional fiberglass pins or, more recently, the use of monolithic, customized CAD/CAM-fabricated slabs. (Perdigao J, 2016).
The destruction of SHS is directly related to their mechanical properties. UHS exhibit different resistance to cracks, depending on their composition and microstructure properties. (Seefeld S, 2007).
A low ratio of fibers to composite (less than 60%), cracks, bubbles, uneven distribution of fibers, and the appearance of large areas with composite are the main reasons for the defective state of pin structures. Premature loss of composite-fiber bonding also weakens the mechanical properties of the pins.
Another factor contributing to poor crack resistance is the way the post is made radio-opaque: the mechanical strength of the SWS is reduced when barium, zirconium and other radio-opaque particles are placed in the matrix, reducing the number of fibers and creating areas of structural laxity. (Seefeld S, 2007).
SWS must be carefully selected based on its mechanical properties, especially when the amount of remaining tissue is small. In such clinical cases, the crown adapts and redirects the forces mainly to the core material and to the SWS, thereby creating an important mechanical load. This situation is less critical if there is remaining crown tissue (ideally 2 mm high, 1 mm thick, 360 degrees around the stump), which can create the so-called “ferrule effect”. (Ferrari M et al, 2012).
The weak “ferrule effect” of the crown must be taken into account when using a low-resistance CVS, since the pin may crack at the mouth of the canal. Although the use of low-mechanical strength SWS often results in post failure, root failure is rare. (Perdigao J, 2016).
It is necessary to select UPS with higher resistance to cracks and fatigue loads, in the absence of a “ferrule effect” or a weakly expressed “ferrule effect”. (Bertoldi Hepburn A, 2011).
Stable but rigid pins (metal or zirconium based) will not deform and can redirect the forces acting on them to the root, which will lead to its destruction. (Baba N & Goodcare C, 2014).
The size of the CVS is also important to improve mechanical properties, but dentin should not be removed in order to use a thicker post. With the help of means that increase pin retention, it is also possible to create a more voluminous structure: individualized / modified for individual anatomy of the UPS, additional UHS, the use of a composite, the use of fiber, etc. (Perdigao J, 2016).
The newly released SWS have proven effective in preventing two common application problems (de-cementing and fracture). The so-called oval SST has an increased taper at the mouth of the tooth, and the geometry of its cross-section gradually changes from round to oval. Because of these geometry modifications, the post takes up most of the space in the expanded post hole and provides friction with the dentin. This enhances the mechanical retention of the pin. At the same time, thanks to its larger volume and higher fiber-to-composite ratio (more than 70%), as well as its ideal structure (no cracks, bubbles, correct distribution of fibers, etc.), the oval SWS becomes an endodontic post with high resistance to cracks.
Despite the increased size mentioned above, the oval post retains a modulus of elasticity similar to that of dentin. Its changes are minimal and do not affect the clinical use of the pin.
What it is
If a person does not treat the tooth in a timely manner, the crown is destroyed. And sometimes this leads to the need for additional support to restore the tooth. A pin is used here if the roots are suitable for prosthetics. Thus, the dentition is not deformed and the jaw structure is preserved.
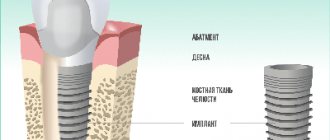
A pin is a structure that is fixed in the root canal. To install it, you need to meet certain conditions - 2 mm thickness of the root walls, it is possible to unseal the canal, completely seal it and give it the desired shape.
general characteristics
A parapulpal pin is a dental rod made of a stainless metal alloy with a polymer coating.
The diameter of the structure is in the range of 0.3 - 1 mm, length - 5 mm. The number of implanted pins is determined by the type of dental elements and the degree of damage. Restoring anterior units involves installing a pin on each corner of the crown. In lateral teeth, the number of parapulpal pins corresponds to the number of missing humps. The distance between products is 5 mm.
The pin is implanted not into the tooth cavity, but into the dentin. Pulp tissues are not affected. The product acts as a basis for the prosthesis, securely fixing it in place and reinforcing the filling.
Kinds:
- Cementable - fixed with a cement composition in a wide passage.
- Friction - implanted into a canal of smaller diameter than the pin.
- Screw-in – screwed into the created channel.
- Combined - use two methods of fixation.
Application in dentistry
A pin is used quite often in dentistry to restore a tooth that has been damaged. But using a pin also:
- build up a tooth;
- prosthetics are used when it is not possible to attach a fixed prosthesis to neighboring teeth;
- reinforce the tooth where the pulp was removed;
- for splinting teeth in case of periodontal diseases;
- to perform replantation surgery.
Examples of work with pins performed at the Family Dental.
Application of a standard titanium anchor pin from Maillefer (Switzerland)
The patient complained of a cracked bridge with worn-out crowns. An examination was carried out, x-rays were taken and a diagnosis was made. The old bridge was removed. It was decided to strengthen the upper canine, which served as a support for the bridge, with a standard anchor pin.
The picture shows the root of the tooth, from the side of the chewing surface, prepared for a standard pin. The root is destroyed above the gum, the walls are thick - all this allows the use of a standard pin with the same reliability as an individual pin, and the cost of a standard pin is lower.
An analogue of a pin is inserted into the prepared root. If necessary, you can take an x-ray with an analogue to ensure that the pin is correctly positioned in the root.
The photo shows the pin next to the analogue.
The pin is inserted into the root, and the position of the pin relative to the opposing teeth is checked.
With the help of a rubber dam, the tooth root is isolated from the effects of saliva, which increases the reliability of operation. You can read more about the use of rubber dam here .
The cement secures the pin into the root of the tooth.
The so-called stump is molded from the restoration material on the pin - the basis for the future crown.
The final view of a tooth prepared for a crown. The tooth is ground with a shoulder, which makes it possible to make a higher-quality and durable metal-ceramic structure. You can read more about this in the section “ Metal ceramics ”. The dark rim around the tooth is a special retraction thread that is placed between the gum and tooth in order to move the gums back and prevent injury to the gums by the bur.
Installation of a dental post
Several procedures are performed here:
- A treatment regimen is determined. The doctor tells how the pin will be installed, what material is best suited for the patient;
- The tooth is being prepared. It is processed and the filling, if any, is removed. In the case of a pin made of fiberglass or carbon fiber, the excess material is trimmed off. The rod is then fixed inside the canal using a composite;
- When the pin is fixed, the cement has hardened, and the part of the tooth that is the crown is restored. If the pin is on the front tooth, then you need to carry out artistic restoration so that it acquires a natural shade.
In what cases is it recommended to install pins?
Indications for the use of anchor pins are tooth destruction of varying degrees of complexity: from simple chips to almost completely lost volume of the tooth surface. Pins are installed when:
- destruction of the crown of the front tooth. The incisors and canines bear a huge load when biting; the corner or cutting edge of the tooth often breaks off;
- the destructive consequences of caries, when the enamel surface is severely damaged and holes appear in the chewing elements;
- consequences of injury, when one or more teeth have lost their integrity.
A prerequisite for the use of a titanium pin is an acceptable layer of dentin between the root and the gum. When the bone tissue is thinning, reliable fixation of the metal rod is impossible, so bone augmentation may be recommended. During extension, the membrane is also fixed with miniature titanium pins.
If a tooth hurts after installation, what should you do?
When a damaged tooth is restored, tissue may be destroyed. Therefore, sometimes the patient feels that the treated tooth hurts. If there was no pain before the procedure, and the tooth has been depulped for a long time, then the pain may arise due to the fact that the canal was entered too deeply. Then it is worth taking an x-ray to determine the cause of the pain.
It happens that pain occurs due to an allergy to a certain material. It can also manifest itself as deterioration of the condition, hyperemia, stomatitis.
Structural elements
The design consists of several elements, each of which is discussed below.
Drill
A product with two cutting edges and a pair of helical grooves for the exit of dentin filings.
For implantation to a depth of 0.2 cm, an immersion limiter is provided. Contact of the device with enamel may cause damage. Therefore, the structure is made of carbon steel.
During the drilling process, the doctor must take into account certain operating points:
- The direction of movement of the drill is counterclockwise.
- Manipulations are carried out carefully and at a slow pace.
- Sharpness of drill edges.
- To prevent clogging of the channel with sawdust and overheating, the drill should be removed.
- Reduced vibration at the tip.
The passage for pin insertion is created at an angle of 90 degrees to the bone tissue. The area intended for the channel is leveled with a coarse-grained bur. Using a spherical fine-grained device, a depression is created.
Kernel
Made from titanium, gold or stainless steel. Products are available with diameters from 0.3 to 0.8 mm. The higher the parameters, the more intense the retention in the bone. Thin modifications are characterized by reduced strength and fragility under load.
The complex configuration of the device helps create retention in the filling and bone tissue. The screw-in rod is inserted to a depth of 1.5 to 2 mm. Cemented models are implanted at a depth of 3–4 mm.
The proportions of the length of the pin inside the filling and inside the dentin are 1:1. Total length – 5 mm.
Dentine
Strong and elastic tissue into which a parapulp pin is implanted. The edges of the product are freely screwed into the canal without damaging the bone.
The distance between the pins is ideally up to 5 mm. The direction of passage must coincide with the dental axis.
When screwed in, the pin rests against the bottom of the canal and puts pressure on the dentin, causing cracking. The special design of the pin with a platform in the center resting on the bone allows you to avoid negative effects. An additional method of protection is to unscrew the rod back a quarter or half a turn.
Seal
Approximately half of the rod is located in the filling composition. The filling falls out due to a weak connection between the rod and the dentin and the filling.
The dentist is faced with the task of making sure that the part of the pin located in the cavity does not touch the walls, and the free space is 0.5 mm.
Pin is not used with amalgam fillings, mineral compounds and composites. Due to the load, the material cracks in the pin area, which leads to the loss of individual fragments.
The clearance for amalgams between the antagonist tooth and the pin should be 1.5 – 2 mm. The use of cement is not recommended.
There is a risk of the pin showing through the composite material. The use of dental compounds will help to avoid this: plastic, gold plating, light-curing coating.
Flaws
With the help of pins, you can restore even a tooth that is almost completely destroyed. But there are certain disadvantages of this design and its application:
- if there are errors in the manufacture of the pin, the tooth may then deteriorate faster and complications may arise;
- If it is necessary to remove the pin, then all materials are removed from the roots. After all, the pin is locked tightly;
- an allergy to the material can provoke a reaction in the body;
- Since the walls of the tooth are subjected to stress, they become thinner. And this destroys the tooth and does not allow it to be restored.
Selecting the type of pin
The choice of the type of pin always remains with the doctor. You cannot choose a pin based on price, as the wrong pin can harm your health. When choosing a pin, the doctor’s specialization plays a role. Thus, the general practitioner may not be aware of the possibilities of orthopedic pinning of teeth with stump inlays, and the orthopedic doctor may use stump inlays more often, even if it is sufficient to install a standard pin. If you want to get the most accurate recommendation, then the best option would be to contact a dentist who has experience as both an orthopedist and a therapist.
Contraindications for installation
Contraindications for the use of pins are related to how damaged the walls and roots are, how thick the walls of the tooth are, how long the canals are, how obstructed they are, and whether there is inflamed, damaged periodontitis tissue. Also, the structure cannot be installed if there are granulomas, cysts, caries, or other diseases.
Before placing a pin, a specialist must examine the tooth that was damaged, clean the canals, and take an x-ray. If the length of the root is less than the height of the dental crown, then such a procedure cannot be performed. The walls must be 2 mm thick, otherwise the load on the tooth will be very large, as a result of which it will simply begin to collapse. In addition, the tooth root must have good stability.
Recommendations for using fiberglass pins
Larisa Lobovkina, Ph.D. , Federal State Budgetary Institution “FCCPI” of the Ministry of Health of Russia, Moscow; Petr Lobovkin , Federal State Budgetary Institution “52 CDC” of the Russian Ministry of Defense, Moscow. When there is significant destruction of the crown part of a tooth, the question often arises: what is the best way to restore such a tooth? Doctors from different dental schools achieve good results, sometimes in completely different ways.3
It is well known that the strength and reliability of restoration often determines not only the future fate of one tooth, but also the effectiveness and service life of a particular orthopedic structure, which significantly increases the doctor’s responsibility for the quality of the work performed.
Unfortunately, it has not been established precisely at what minimum volume of preserved tissue it is necessary to use intracanal pins. The decision made is based primarily on the doctor’s personal experience and intuition. It is obvious that decisions are sometimes made that are not entirely justified.
Many dentists now agree that the amount of remaining hard tissue in the tooth is critical to an end-canal post restoration. In our work we are guided by the following recommendations:
- For anterior teeth and premolars, restoration with pins is required if the crown has only two walls left.
- For molars, if there are two remaining coronal walls less than 3 mm high and there is a flat pulp chamber with insufficient surface area for the retention of an adhesive restoration, this is also an indication for a post construction.1
However, when restoring the damaged coronal part of a tooth using fiberglass pins and artificial crowns, we often hear from our colleagues, orthopedic dentists, that very often such teeth are fractured. This situation can indeed occur when using low-quality fiberglass pins. But this never happens when working with high quality pins.
This fact is confirmed by studies by Mannoci and Ferrari,8 which found 9% of root fractures after restoration with cast structures during the first 4 years and no fractures after restoration with fiberglass pins over the same period.
After analyzing clinical situations and literature data, the authors came to the conclusion that when restoring the destroyed coronal part of a tooth using fiberglass pins, the dentist can make a number of mistakes leading to unsuccessful results, namely:
- Selecting low-quality fiberglass pins. The quality of fiberglass reinforced composite posts varies greatly. It depends on the manufacturing technology, the uniform distribution of fibers in the organic matrix with the most dense packing of the fibers, the strength of the connection of the fibers with the matrix, the degree of polymerization of the organic components and the homogeneity of the structure of the pin.7 The optimal combination of glass fiber and matrix, which in its physical properties would be similar to the structure teeth and at the same time had the strength of metal - it is 75% fiberglass and 25% (up to 42%) composite. The bending strength is 560 MPa. To break a fiberglass pin with a diameter of 1 mm, a force of 160 kg is required.6
- The pin is not fixed to the optimal depth. Previously it was believed that the pin should be fixed at 2/3 of the length of the canal. However, this is not entirely true for fiberglass pins. A sufficient length is considered if the pin extends into the canal by 4–5 mm, but not more than 6 mm, i.e. up to ½ root length! If the pin is too short, the fulcrum increases and so does the risk of fracture. In addition, if the length is too short, the pin does not serve any function in the tooth and its biomechanical value is reduced to zero. If the pin is too long, the risk of fracture increases due to excessive potential bending.
- Weakening of the tooth as a result of excessive removal of cervical dentin. It is necessary to create a primary endodontic access using optimal instruments to preserve as much cervical dentin as possible. When creating a post-channel, also be careful in this area. The more cervical dentin that remains, the longer the service life of the direct or indirect restoration. Creating a large diameter access after 5 years leads to root fracture.2
- Use of adhesives that do not have a dual curing mechanism when fixing pins. This leads to incomplete polymerization of the adhesive inside the channel, which reduces the strength of the structure itself.
- Incorrect choice of material for fixing fiberglass pins. Please note that most fiberglass pins available on the market are not light conductive. Therefore, they need to be cemented only with dual-cure composite cements and not with glass ionomer cements or other materials.
- No silanization step for the fiberglass pin. Today, both silanized and non-silanized fiberglass pins are widely available on the dental market. The fact is that fiberglass itself is inert, so to form a strong bond with dual-cure composite cement, it is necessary to coat the pin with a surfactant. Silanization of the pin is carried out by applying a silane agent to its surface.
CLINICAL CASE
Using this clinical case as an example, a technique for the clinical use of a fiberglass-reinforced root post is presented.
A 53-year-old patient came to the dental clinic to prepare for orthopedic treatment. After consulting an orthopedic doctor, it was decided to carry out repeated endodontic treatment of tooth 33. Subsequently, it was planned to install a fiberglass pin, and then make a metal-ceramic crown for tooth 33.
To restore the coronal part of the tooth and fix fiberglass pins, the Rebilda Post (VOCO) system was chosen, which includes: Rebilda Post fiberglass pins in an assortment, several calibration drills for pins of different diameters, a dual-curing adhesive system Futurabond DC , ceramic bond for silanization of pins and a composite double-curing Rebilda DC , which has a composite consistency of increased fluidity, which allows you to fill all undercuts.
After applying a rubber dam and the initial passage of the Largo Peeso-Reamer canal (which is also part of the Rebilda Post system), the final configuration of the canal was created for the patient using a calibration drill corresponding to the diameter of the selected pin, and the pin was fitted in the canal (Fig. 1).
Rice. 1 After cleaning with alcohol, the pin was ready for fixation. The authors point out that Rebilda Post pins are already silanized, so applying a ceramic bond to them is not necessary. However, after medicinal treatment of the post, some of the silane agent can be removed. Therefore, ceramic bond (Ceramic Bond, included in the Rebilda Post kit) was applied to the post and then air dried (Fig. 2).
Rice. 2. Disinfection of the intracanal space was carried out by irrigating it with a 3% sodium hypochlorite solution, rinsing with distilled water and drying with paper points. The intracanal space and hard dental tissues were treated with the self-etching adhesive of the 6th generation of dual polymerization Futurabond DC, available in the Rebilda Post kit, for 20 s and dried with a stream of air (Fig. 3).
Rice. 3. There are conflicting data on the need for adhesive polymerization in the root canal. However, some authors believe that the adhesive layer should not be cured, since there is a danger that remaining excess adhesive, especially in areas of the root canal that are not accessible to visual inspection, will prevent the fiberglass post from being positioned in the correct final position.7 When using conventional adhesives, there is a high probability of incomplete fixation. polymerization, because the light guide is located at a considerable distance from the root canal, and not all pins have light conductivity, as mentioned above. Only the use of dual-cure Futurabond DC adhesive eliminates this problem, since the material self-cures chemically within 3 minutes.
After adhesive preparation of the root canal, dual-curing composite cement Rebilda DC was introduced into it, which did not polymerize. Then the prepared fiberglass pin was inserted into it and installed in a given position with light rotational movements. This “dip-fill” technique ensures that no air voids are created in the composite layer, thereby achieving maximum adhesion to the canal walls while optimizing bond density.5,7 The entire system was cured within 40 s. After this, the crown part of the tooth was restored using the same Rebilda DC composite (Fig. 4).
Rice. 4. The permissible thickness of the applied layer is 4 mm, therefore, using this system, it is possible to fix the fiberglass pin and restore the tooth core in a matter of minutes.
The authors point out that many dental clinics purchase fiberglass pins and materials for their fixation at a cheaper price of dubious quality (pins with parallel walls, with a low content of glass fibers and a large volume of epoxy resin). As a result of this, a number of complications arise (fracture of the tooth crown, decementing of pins, etc.), all the blame for which lies with the doctors.
In a number of clinical studies, only quality fiberglass reinforced composite root posts with adhesive retention show very promising results.4,8
Thus, composite-reinforced fiberglass posts are a good choice for restoring severely damaged teeth due to their quick and easy application technique as well as their optical advantages.1,4
LITERATURE
- Bruder M. Restoration of severely damaged teeth after endodontic treatment - indications and contraindications. New in Dentistry 2008;6:16–18.
- Buchanan S. Zen and the art of endodontic access. Dental Tribune 2017;2(16)2–6.
- Malanin I.V. The influence of restoration on the prognosis of endodontic treatment. Dentistry Problems 2007;4:10–12.
- Truszkowski R. Restoration of endodontically treated teeth: indications and techniques. Quintessence 2014;1:109–123.
- Biacchi GR, Mello B, Basting RT. The endocrown: an alternative approach for restoring extensively damaged molars. J Esthet and Restorative Dent 2013;25(6):383–90.
- Edelhoff D, Spiekermann H. All about modern root post systems. New in Dentistry 2003;5:44–48.
- Manhart J. Restoration of teeth after endodontic treatment using fiberglass-reinforced composite posts. New in Dentistry 2018;6(234):86–90.
- Mannoci, Ferrari, Watson TF. Microleakage of endodontically treated teeth restored with fiber posts and composite cores after cyclic loading: a confocal microscopic study. J Prosthet Dent 2001;85(3):284–91.
Go to the website of the official distributor of VOCO GmbH in Russia Dental Times 38