53209
Crooked, unhealthy teeth can ruin the appearance of an otherwise attractive person. Oral health is important not only for our attractiveness, because the main function of teeth is to grind food. The condition of the stomach and intestines depends on this, which directly affects health and life expectancy .
How is the bite formed?
The process of bite formation is long - from birth to adolescence. There are 5 periods.
- Initial (up to 6 months): no teeth, the upper jaw is larger in size than the lower jaw. At this time, an active feeding process is extremely important for the proper development of the jaw apparatus.
- Emerging temporary bite (6 months - 3 years): baby teeth and a bite appear, but it is still temporary. This stage is accompanied by inflammation of the gums, a rise in temperature, often grinding of teeth (bruxism), and emerging teeth may be crooked. It is important to maintain hygiene without taking any orthodontic measures.
- Formed temporary occlusion (3 - 6 years): baby teeth have erupted and can close in different ways, jaw growth continues. This is the time of active use of teeth. Characteristic wear of temporary teeth is considered normal before the upcoming change.
- Changeable dentition (6-12 years): jaw growth, loss of baby teeth and appearance of permanent teeth. Often new teeth, especially the lower ones, erupt unevenly. During this period, it is necessary to decide on a plan for further correction of the bite.
- Permanent dentition (12 - 15 years): replacement of milk teeth with permanent ones, all 28 teeth are visible, no wisdom teeth. The period is most favorable for orthodontic treatment.
In order for the bite to form correctly, there must be careful attention to teething, oral hygiene, and a timely plan to correct emerging problems.
Features of correct bite in a child
If we consider this problem in terms of age, then the characteristics of the correct bite at any period of a person’s life will be similar. The only exceptions we can put aside are children, in whom only after changing their baby teeth can we say with 100% probability that they have a correct or incorrect bite.
In fact, an adult bite is no different from a child’s bite from an anatomical point of view.
The correct arrangement of the dentition is comparable at any age, as is the structure of the jaw. But still, it is worth paying attention to the state of the bite of children more often due to the rapid growth of all parts of the chewing apparatus and the gradual replacement of milk teeth with primary ones.
The bite is formed from birth, and the process lasts up to 15 years. Development occurs in stages, from the moment the first primary incisors appear. After changing all the elements, the bite becomes permanent. Its formation is directly influenced by both hereditary and external factors.
In childhood, it is important to pay increased attention to the prevention of the development of correct bite, so that the jaw bones and teeth alignment correspond to the physiological norm.
For proper development of the bite, it is necessary to: keep the child breastfed from birth; Try not to accustom your baby to a pacifier and pacifier. If this is difficult to achieve, you need to use rubber as little as possible; prevent the development of bad habits such as sucking fingers and toys. During sleep, the child's mouth should be closed and the head should not be thrown back. From the beginning of the growth of baby teeth, it is necessary to include solid foods in the diet.
You should consider visiting an orthodontist after teething.
If necessary, the specialist will prescribe a comprehensive examination and radiography to identify the causes of dental pathologies. Then you should get advice from doctors in related fields. Specialists will determine contraindications, the likelihood of complications and assess the condition of the baby’s entire body.
Based on the data obtained, the orthodontist will draw up a treatment plan for approximately 2 years with monthly clinic visits.
There are several risk factors that may indicate that your child needs to correct his bite: deformation of the spinal column, a genetic predisposition to pathologies of the development of the dental system, difficulty breathing through the nose, diseases of the central nervous system and bad habits (grinding teeth, pushing the lower jaw forward or swallowing, clicking jaw joints, etc.). But only a doctor can give an accurate conclusion on the issue of correcting the bite.
Therefore, it is best to contact myofunctional centers, which unite orthopedists, pediatric dentists, orthodontists and osteopaths. The joint work of specialists guarantees accurate diagnosis and successful resolution of the issue.
In modern dentistry, there are various devices for correcting malocclusion in children, designed to achieve the following goals:
- prevention of bad habits;
- expansion of the jaw arch;
- correction of speech defects;
- normalization of the functioning of the masticatory muscles;
- tongue position control.
Correct teeth bite
An ideal orthognathic bite implies the presence of the following features:
- The upper dental arch is slightly inclined forward and has the shape of a semi-ellipse, the lower, in the shape of a parabola, is slightly backward.
- When the jaws close, each upper tooth contacts the opposite tooth below.
- There are no obvious gaps between the teeth.
- The upper teeth overlap the lower teeth by about a third of their height.
Despite the fact that there are the above parameters for a perfect smile, the question “What should be the bite of the teeth?” cannot be answered unambiguously. In addition to the orthognathic bite, modern orthodontics allows for several options for the normal structure of the dentition and the location of the jaws.
Orthognathic
The upper row of teeth overlaps the lower one by 30% of the height, there are no gaps between the teeth or spaces between the rows.
Biprognathic
The dentition is slightly directed towards the vestibule of the mouth.
Progenic
The lower jaw moves forward slightly.
Straight
When the jaws close, the upper teeth come into contact with the lower cutting edges.
Restoration of anterior teeth before and after photos
However, each medical procedure has its own contraindications and limitations that the patient needs to be aware of.
Malocclusion of teeth
Look at your reflection in the mirror. If you notice an excessively protruding upper or lower lip, teeth that “overlap” each other, or gaps between the dentition when the jaws are closed, this is a clear reason to consult a specialist. Descriptions of dental anomalies and photographs of teeth with malocclusion pathologies are presented in the table below.
Distal (prognathic)
In a distal bite, the upper jaw is more developed than the lower jaw.
Mesial (medial)
With a mesial bite, the lower jaw is pushed forward.
Cross
In a crossbite, the rows of teeth intersect in the manner of scissors when the jaws close.
Deep
In a deep bite, the upper teeth significantly overlap the lower teeth.
Open
The presence of pronounced gaps between the dentition when the jaws are closed indicates an open bite.
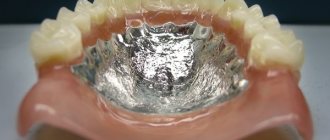
Bite in the absence of teeth
A person without teeth has problems with the functioning of the temporomandibular joints, facial aesthetics deteriorate, and wrinkles appear due to loss of skin tone. To avoid unpleasant consequences, it is necessary to restore the bite using a complete denture made using a special technique.
Bite restoration with complete dentures
- The central ratio of the jaws is determined - the position of the lower jaw in relation to the upper in three planes: vertical, sagittal and transversal. The role of the dentition is played by wax rollers.
- Measurements are taken using a device consisting of an external facebow-ruler and an intraoral plate with a flat frontal part and curved distal parts.
- The plaster model marks the boundaries of the future structure, the line of the middle of the alveolar process, the tubercles of the upper and lower jaw, and the midline.
- Artificial teeth are placed in such a way that when you smile, the part of the prosthesis that imitates the gum is not visible.
Bite after wisdom tooth removal
Some doctors are convinced that wisdom teeth are an atavism and must be gotten rid of. In ancient times, they were used to chew tough foods, such as raw meat. With the development of civilization, the human diet changed, his jaw began to gradually decrease - and the “eights” turned out to be superfluous. Most often, before starting to correct the bite, wisdom teeth are removed. This frees up space for the correct formation of rows, and the result of teeth alignment will be much better.
What affects the bite of teeth?
The negative impact of defects in the dental system on the condition of the entire organism has been repeatedly proven by scientists. The list of identified health risks is impressive even for ardent optimists.
- Due to improper distribution of the chewing load, tooth enamel wears off faster, teeth begin to react painfully to cold and hot, their necks become exposed, and noticeable gaps form between the teeth.
- Diseases of the temporomandibular joints occur, accompanied by headaches and a characteristic clicking sound when the jaws move.
- The aesthetics of the face suffers: its proportions change, wrinkles form, teeth become crooked, and the smile becomes unattractive.
- It becomes difficult to bite food, chewing functions are disrupted, causing diseases of the gastrointestinal tract.
- Speech defects appear, facial expressions are distorted, and self-esteem decreases.
- Crowding and crooked teeth cause accelerated tooth decay due to frequent chipping and carious lesions.
- The oral mucosa is injured - cheeks, gums, tongue, and the tissues of the oral cavity become inflamed.
- The quality of breathing deteriorates, which leads to diseases of the nasopharynx, trachea, and hearing aid.
Periodontitis
Periodontitis in its final form is a serious infection that damages soft tissue and destroys the bone that supports the teeth. Periodontitis can not only lead to tooth loss, but worse, it can cause an increased risk of heart attack or stroke and other serious health problems.
Periodontitis is a common disease, but largely preventable. Periodontitis is usually the result of poor oral hygiene. Brushing at least twice a day, daily, and regular dental checkups can significantly reduce the chance of developing periodontitis.
Symptoms
You may find that you have gingivitis:
- Swelling of the gums (edema)
- Bright red or purple gum color
- Gums sensitive to touch
- Gum that “pulls away” from your teeth, making your teeth appear longer than usual
- Pus from under the gums
- Bad breath
- Bad taste in mouth
- Movable teeth
There are different types i.e. severity of periodontitis. Periodontitis is characterized by a chronic course, with exacerbations occurring.
When to see a dentist
Healthy gums are firm and pale pink in color. If your gums are puffy, dusky red and bleed easily, or show other signs or symptoms of periodontal disease, see your dentist as soon as possible. The sooner you seek medical help, the better your chances of reversing the damage from periodontal disease, potentially preventing other serious health problems.
Causes
Periodontitis is thought to begin with plaque, a sticky film made primarily of bacteria. Plaque forms on teeth when sugar starches in foods interact with bacteria that are normally found in the mouth. Brushing and flossing remove plaque. But plaque re-forms quickly, usually within 24 hours.
Constant inflammation eventually leads to pockets between the gums and teeth that become filled with plaque, tartar, and bacteria. Over time, these pockets become deeper and bacteria accumulate, moving under the gum tissue. This deep inflammation is the cause of bone resorption. If too much bone is destroyed, you may lose one or more teeth.
What can cause periodontitis?
Factors that may increase the risk of developing periodontitis include:
- Gingivitis
- Heredity
- Insufficient oral hygiene
- Tobacco use
- Diabetes
- Elderly age
- Decreased immunity, such as leukemia, HIV/AIDS or chemotherapy
- Poor nutrition
- Some medications
- Alcohol or drug abuse
Complications
Some complications associated with gum disease include:
- Complete loss of teeth
- Coronary heart disease
- Stroke
- Problems with pregnancy, low birth weight
- Poorly controlled diabetes
- Breathing problems
- Rheumatoid arthritis
- Asthma
Some research suggests that the bacteria responsible for periodontitis can enter the bloodstream through the gum tissue, affecting your lungs, heart, and other parts of your body. For example, bacteria can travel in the arteries to the heart and cause inflammation of the heart muscle, which contributes to heart attacks.
Treatment of dental malocclusion
How to change the bite of teeth? Pathologies of the dental system can only be eliminated through orthodontic treatment. An exception is the correction of a low bite, when the height of the teeth decreases with age due to their wear. In such cases, the bite is corrected by dental prosthetics with crowns or veneers, as well as by implantation. Other anomalies of teeth and bite can be removed at any age with special orthodontic structures or through surgical intervention.
However, maxillofacial operations are performed only in case of serious deviations from the norm. Usually, to correct dental malocclusion, doctors suggest correction with braces or aligners.
Now that you know about all the health risks that can cause pathologies of the dental system, and how to correct your dental bite, all that remains is to take specific actions. Even if at first glance it seems that your teeth are straight, make an appointment with an orthodontist. Diagnosing the condition of the dentition will help maintain the health of other organs and systems. And timely orthodontic treatment will make your smile more attractive and significantly reduce the number of future visits to the dentist.
Gingivitis
Gingivitis is a common and mild form of gum disease that causes inflammation, irritation and redness. Because gingivitis can be mild, you may not be aware that you have inflammation. But it's important to take gingivitis seriously and act quickly. If you do not undergo careful treatment, gingivitis may eventually develop into a more serious disease – periodontitis. Ultimately, this can all lead to complete tooth loss.
The most common cause of gingivitis is poor oral hygiene. Good habits such as brushing, flossing at least twice a day, and regular dental checkups can help prevent gingivitis.
Symptoms
Healthy gums are firm, painless and pale pink in color. If your gums are puffy, dark red, and bleed easily, you may have gingivitis. Because the disease is rarely painful in its early stages, you may have gingivitis without even knowing it.
Signs and symptoms of gingivitis include:
- Swollen gums
- Soft, plump gums
- Sensitive gums
Gums that bleed easily when you brush or floss.
Redness or pinkishness on the brush or toothpick is sometimes seen.
- Changing the color of your gums from a healthy pink to red
When to see a dentist
Most dentists recommend regular exams to screen for gingivitis, tooth decay, and other dental diseases. The doctor eliminates the causes of the disease - treating only the symptoms of the disease at home can lead to more serious problems. If you notice any signs and symptoms of gingivitis, it is recommended that you make an appointment with your dentist. The sooner you seek medical help, the better your chances of reversing the damage from gingivitis and preventing it from progressing to periodontitis.
Causes
The most common cause of gingivitis is poor oral hygiene, which contributes to plaque formation. Plaque is invisible - it is a sticky film consisting mainly of bacteria. Plaque forms on teeth when starches and sugars in foods interact with bacteria normally found in the mouth. Brushing your teeth at least twice a day and flossing every day are recommendations from any dentist. Plaque requires daily removal because it forms quickly, usually within 24 hours.
Plaque that remains on the teeth for longer than two or three days can harden under the gums into tartar. Tartar can also develop as a result of minerals in saliva. Tartar makes plaque more difficult to remove and creates a protective shield for bacteria. You usually can't get rid of tartar by brushing or flossing—you need ultrasonic teeth cleaning to remove it.
The longer plaque and tartar remain on your teeth, the more they irritate the gums around the base of your teeth. Over time, your gums become swollen and bleed easily. It can also lead to tooth decay.
Risk factors
Gingivitis is common and anyone can experience this condition. Many people first experience gum problems during puberty and then to varying degrees throughout their lives.
Factors that may increase your risk of developing gingivitis include:
- Insufficient oral hygiene
- Tobacco use
- Diabetes
- Elderly age
- Decreased immunity due to leukemia, HIV/AIDS
- Some medications
- Some viral and fungal infections
- Dry mouth
- Hormonal changes that are associated with pregnancy, the menstrual cycle, or the use of birth control pills
- Poor nutrition
- Alcohol or drug abuse
- Unsuitable dental restorations
- Poor quality prosthetics
Complications
In its chronic form, gingivitis can progress to gum disease that spreads to the tissue and bone of the jaw, which can lead to tooth loss.
Periodontitis and poor oral hygiene in general can also affect your overall health. Also, today it is not entirely clear whether this is true, but the disease may be associated with:
- Heart attack
- Stroke
- Lung disease
- Premature birth or the birth of a child with low body weight or other pathology
Tests and diagnostics
Dentists usually diagnose gingivitis based on complaints and an examination of your teeth, gums, mouth and tongue. Your dentist will look for plaque and tartar on the teeth and check the gums for redness, swelling and bleeding - this will help him make an accurate diagnosis and determine the form and extent of the disease.
If it is not clear what caused your gingivitis, your dentist may recommend that you get a physical examination to check for underlying health conditions.
Procedures and drugs
Prompt treatment usually reverses the symptoms of gingivitis and prevents it from progressing to more serious gum disease and tooth loss. Effective treatment requires professional care followed by oral hygiene at home.
Professional prevention includes:
- Initial assessment and thorough teeth cleaning to remove all traces of plaque and tartar
- Instructions for effective home flossing
- Regular professional inspections and cleanings
- Special cleaning in places where crowns and fillings are attached, implants installed
Your initial professional cleaning will include the use of dental instruments to remove all traces of plaque and tartar.
Uneven teeth or poorly fitting crowns, bridges or other dentures can irritate your gums and make at-home plaque removal more difficult. If problems with your teeth or dentures are contributing to gingivitis, your dentist may recommend correcting these problems.
Lifestyle and Home Remedies
Steps you can take at home to prevent and reverse gingivitis include:
- Regular professional dental cleanings on a schedule recommended by your dentist.
- Using a soft toothbrush—replace it at least every three to four months.
- Using an electric toothbrush, which may be more effective at removing plaque and tartar.
- Brushing your teeth twice a day, or better yet, after every meal.
- Use toothpicks at least once a day.
- Use an antiseptic mouthwash if recommended by your dentist.
If you are consistent with your home hygiene, you should see the return of pink, healthy gum tissue within a few days or weeks. You will need to practice good oral hygiene every day.
Prevention
The best way to prevent gingivitis is a good oral hygiene program that is followed consistently throughout your life. Brushing and flossing for three to five minutes is as much a daily ritual as eating.