Spending a long time in the cold or severe hypothermia can lead to inflammation of the dental nerve. The dental nerve can also become inflamed in hot weather, for example, if the window in your car is open. Inflammation of the dental nerve is an unpleasant disease; it may be indicated by symptoms such as the appearance of painful pulsation, constant aching pain in the tooth. If these symptoms are present, it means you have the nerve of the tooth is chilled. The very first thing to do is to understand which tooth is damaged.
Healthy teeth do not react in any way to temperature changes; usually we do not notice it at all. But if any pathological processes occur inside the dental shell, then from a long walk in the cold you may feel severe toothache. The most correct decision in this situation is to seek help from a dentist.
What to do if the nerve in the tooth has caught a cold - symptoms, treatment and prevention
After a long stay in the cold, your tooth may ache. In this case, aching pain with twitching usually occurs - this is a direct sign of a cold nerve. If your teeth are in perfect order, they should not give any reaction to temperature changes. But if there is a pathological process, including a hidden one, it can worsen as a result of hypothermia. Further in this article we will talk about what to do if the nerve of the tooth has caught a cold, and how to quickly get rid of toothache and prevent the development of complications.
Treatment methods
Experts practice removal of wisdom teeth in case of carious lesions or in cases where extremely problematic eruption is observed for people of any age. Pain and inflammation indicate a serious problem. If it is not resolved in a timely manner, complications cannot be avoided.
Easy removal
The doctor decides what to do in each specific situation based on the research results obtained. This can be either a simple removal or a rather complex multi-stage operation.
Before the procedure, the specialist must make sure that the patient is not allergic to the medications that will be used during the procedures. First, the soft tissue around the tooth and the nerves are numbed. After the anesthesia has taken effect, the tooth is removed using forceps. The duration of the entire procedure does not exceed 10 minutes.
Difficult removal
If the crown of a tooth is destroyed, it has large branched roots, and also if the “eight” has not erupted at all, and the entire jaw is involved in the inflammatory process, complex removal is practiced. During the intervention, the dental surgeon makes one or more incisions, removes the tooth, washes the wound surface, and then applies sutures.
It is also worth mentioning the procedure for excision of the hood. If it is the wisdom tooth that hurts at the time of eruption due to inflammatory processes of the mucous membrane, the doctor removes fragments of “excess” tissue. There may be situations when the wisdom tooth is not removed, but only soft tissue correction is performed. This is true if the tooth itself does not hurt and is located correctly in the socket.
Where is the nerve located in the tooth?
The visible part of the tooth is called the crown - it is covered on top by a layer of enamel, under which there is dentin. Below it is a central part filled with pulp. We are talking about a neurovascular bundle located in the cavity and passing into the internal structures of the root system. The pulp is penetrated by many nerves and vessels. In this case, the number of nerves corresponds to the number of roots. The largest nerves are directly connected to the root processes, while the small ones are concentrated in the pulp chamber.
The photo shows the structure of the tooth
When acute painful sensations occur in a tooth, most often this indicates the development of a pathological process in the pulp. A natural consequence of nerve inflammation is pathologies such as pulpitis and periodontitis. In the initial stages of the disease, there is always a chance to save the pulp and the tooth itself. If the pathology is too advanced, depulpation (pulp extraction) or even tooth extraction may be required.
The main reasons associated with the unpleasant phenomenon
What happens to a person when he gets hypothermia, gets a strong wind, or catches an infectious or viral disease accompanied by inflammation of the ear-nose-throat area? His body temperature rises, a cough and runny nose appears, and all surrounding tissues swell. Against this background, pain arises, which most often covers the entire head, often radiating to the jaw and teeth - this is one of the main reasons why there is a feeling as if the teeth were blown. But there are other factors that lead to this phenomenon. Let's consider them further.
Exacerbation of existing dental pathologies
With hypothermia, as well as any diseases of the body, the immune system sharply decreases, which means that pathologies that already existed before but were not treated become aggravated and progress. For example, caries, chronic pulpitis and periodontitis. Against the background of decreased immunity, untreated caries can very quickly become complicated by pulpitis and periodontitis[1].
On a note! This unpleasant phenomenon is typical for people with weakened immune systems: children, the elderly, women during pregnancy and breastfeeding.
During this period, a cyst or granuloma may make itself known, which gradually grew and remained undetected for a long time. And periodontitis often leads to the appearance of a lump on the gum, filled with pus and periodically breaking out through the fistulous tract. Also, some people, just after they have been blown by a strong wind or in a draft, discover that they have flux and all the accompanying symptoms: their cheek and face swell, their body temperature rises, and, naturally, their teeth hurt badly.
“In our office the air conditioner is always on, which once gave me a very serious blow. Against this background, my jaw began to ache. Later I noticed that the teeth under the fillings also hurt. When I recovered, it still continued to hurt under one filling. I had to go to the dentist... At the appointment they said that there was periodontitis, which developed due to poor-quality treatment of caries and incomplete filling of the canals. This was an unpleasant surprise! As the doctor said, under the influence of a cold, the sore, which had not manifested itself in any way before, became aggravated and worsened..."
Tanika, review from the dental portal gidpozubam.ru
2. Features of the treatment of viral and infectious diseases
Both in case of normal hypothermia, and ARVI, influenza, sore throat, herpes virus and other pathologies of a similar nature, the patient is prescribed to drink plenty of fluids in order to quickly remove toxins from the body, support the immune system and avoid dehydration. The following drinks are often consumed for this purpose: rosehip decoction, tea with lemon, fruit drinks and compotes with berries - they all contain large amounts of vitamin C, which has a destructive and irritating effect on the enamel.
Consequence: the enamel becomes hypersensitive, reacts to the temperature of food and any mechanical stress. Due to the abuse of such drinks, erosions appear on hard tissues, and their resistance to cariogenic bacteria drops sharply.
To avoid this problem, doctors advise thoroughly rinsing your mouth with plain water after drinking acidic drinks.
Poor oral hygiene
After hypothermia and infectious viral diseases, many feel severe weakness and malaise, and therefore stop performing thorough daily oral hygiene. Some people completely forget about the brush and toothpaste, which is why plaque quickly accumulates in the mouth, which is the best breeding ground for bacteria that cause caries and other dental diseases.
On a note! After you have recovered, it would be a good idea to purchase a new brush, since the old one may retain pathogenic bacteria that can provoke an inflammatory process in the oral cavity.
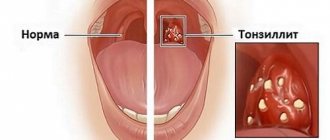
ENT diseases
With otitis media, tonsillitis, sinusitis and sinusitis, strange symptoms sometimes occur, for example, the ear and teeth may hurt at the same time. This is again due to the fact that in a sick person, not only the organs where the pathology occurs swell and become inflamed, but also all adjacent areas. In this case, the pain often does not have a clear localization, radiating to the head, jaw, and eyes.
When ENT diseases are neglected or treatment tactics are incorrect, bacteria spread from the affected tissues to healthy ones, penetrate with blood and lymph into the oral cavity, provoke the development of the same caries, inflame the nerve of the tooth (pulpitis occurs) and periodontal tissue.
On a note! The opposite situation also happens: diseased teeth contribute to the development of ENT pathologies. For example, units of the upper jaw affected by deep caries, pulpitis, periodontitis and cysts can lead to the development of odontogenic sinusitis.
Inflammation of the facial nerve
This nerve has branches that cover all areas of the face. Therefore, when it becomes inflamed, the jaw and teeth may become sore. Often the pain has no clear localization. Pathology, again, can occur against the background of hypothermia, impaired blood circulation in the tissues, as well as various dental and non-dental diseases.
What is the true cause of nerve inflammation
Various factors lead to inflammation of the neurovascular bundle. Among the most common causes of the development of a pathological condition, experts in the field of endodontics identify the following phenomena:
- advanced untreated caries, turning into pulpitis,
- injuries, chips, fractures,
- poor quality treatment leading to relapse of the disease,
- filling using low-quality composites and medications,
- medical errors made during the treatment of the crown before prosthetics,
- other dental diseases accompanied by infection of dental tissues.
Pulpitis can cause inflammation.
As for whether it is possible to catch a tooth nerve, too much exposure to the cold can indeed provoke acute symptoms of inflammation. In such cases, they usually say that the tooth is blown or caught a cold. But in fact, an acute reaction is only a consequence of already existing problems, and the cold is only a kind of trigger.
Why might this happen?
The reasons are obvious:
- Dental nerves are sensitive to cold.
- Prolonged exposure to wind on an unprotected face.
- Lack of headwear in cold weather.
- General hypothermia of the body.
Possible provoking factors should also be highlighted
- Development of caries.
- Tooth chips and injuries.
- Tooth infection.
- The use of low-quality fillings in dental treatment.
- Poor quality prosthetics.
How to recognize the problem - characteristic symptoms
With inflammatory processes in the pulp, symptoms inevitably arise, and they are very intense, so it is quite difficult not to notice them. The most common signs of a problem include the following:
- aching, increasing pain, which can be localized both in the tooth itself and in the jawbone area, radiating to the ear or eye,
- often the pain becomes shooting in nature,
- increased sensitivity of the enamel appears, acute reactions occur to cold, hot, spicy and sour, any mechanical irritants,
- Sensitivity may also extend to the eye and forehead area,
- discomfort appears while eating, talking, or when trying to smile.
One of the symptoms is aching, increasing pain in the tooth or in the entire jaw.
The root cause of the problem is always the pathological phenomena already present in the tooth. When pathogenic microorganisms penetrate the pulp, acute pain of a pulsating nature occurs. It becomes especially strong at night. In such a situation, a sudden change in temperature or prolonged exposure to the cold provokes acute symptoms. When the nerve is inflamed, pulpitis is usually diagnosed, but if the inflammation extends beyond the pulp, periostitis (flux) or periodontitis may develop, including the formation of purulent neoplasms.
How does gum inflammation manifest?
The process has three characteristics:
- The gums are swelling.
- Pain appears.
- The inflamed area feels warmer than neighboring areas.
Other symptoms depend on the cause provoking the phenomenon.
Common additional symptoms include:
- Bleeding when brushing teeth, metallic taste in the mouth.
- Separation of pus.
- Increased body temperature in the patient.
- Severe sensitivity of the teeth near the affected area to hot, cold and sour.
- Loosening of the tooth.
- Noticeable bad breath.
- Formation of white plaque on the gums.
Symptoms occur on their own or when eating or brushing your teeth. The gums on both the upper and lower jaws are susceptible to inflammation.
At the first signs, you should see a dentist as quickly as possible - the problem can progress and lead to tooth loss.
You can recognize the process at home. The affected areas turn red and a white coating appears on them. At the same time, there are complaints about the listed symptoms.
What to do if your nerve gets cold
Regarding what to do if there are obvious signs of nerve inflammation and how to quickly relieve severe pain, experts suggest first carrying out antibacterial treatment of oral tissues in order to prevent the further spread of the pathological process. This can be done by rinsing your mouth with Chlorhexidine or, say, a soda-saline solution.
Gargling with a soda-salt solution will help relieve acute pain.
Next, it is imperative to relieve the pain, but in no case should you apply heat to the cheek from the side of the causative element - this will only intensify the acute symptoms and provoke an even greater spread of inflammation. Read on to find out how best to act in such a situation.
Emergency help
If the tooth hurts very badly, before visiting the doctor you need to at least muffle the symptom a little, and in this case you can take a painkiller tablet: “Ketanov” or, for example, “Nalgesin Forte”. For urgent help, you can resort to external agents with an anesthetic effect. These include the drugs “Lidocaine”, “Kamistad gel”.
Drug therapy
If signs of inflammation appear, the first thing to do is immediately go to the doctor. After a visual examination and assessment of the current condition of the causative tooth, the doctor will definitely send you for an x-ray. Having all the necessary data in hand, the specialist will choose a further vector of treatment: conservative therapy, depulpation or even complete removal.
If the doctor chooses a conservative direction, in this case it will be necessary to open the crown, treat the pulp and administer an antibiotic. After a few days, the acute inflammation should subside - then the patient will be sent for a repeat X-ray. If everything is normal, the doctor will place a permanent filling and prescribe appropriate medications. In such situations, painkillers, antiseptic rinses, and special medicinal pastes are usually prescribed. If the case is advanced, the drug "Amoxiclav" or "Ciprofloxacin"1 may be prescribed.
The photo shows the canal treatment scheme
Surgical intervention is resorted to in the last stages of the pathological process - with the development of pulpitis and periodontitis. To ensure that all foci of inflammation are eliminated, the tooth must be depulped, the canals treated and filled. In this case, a tooth without a nerve, in theory, can no longer hurt, although in practice there are relapses of the symptom after removal of the pulp. This happens when the root canals are treated insufficiently, in which pockets of inflammation remain, if fragments of pulp remain in the canals, or if the pathological process has led to the formation of neoplasms in the root area. In all these cases, urgent assistance from a specialist is required.
What does traditional medicine offer?
If acute symptoms develop, you should definitely visit the dentist, and it is better to do this as soon as possible. Only a doctor can choose an adequate treatment that will be effective and at the same time safe. As a maintenance therapy, the use of traditional medicine recipes is allowed, but only after their agreement with a specialist. Below are popular recipes:
- alcohol tincture with birch buds: to prepare the product, you need to take 25 g of raw materials and pour a glass of alcohol into it. Mix the ingredients thoroughly and leave in a cool, dark place for a week and a half. After this time, the solution will be ready for use - just dip a cotton swab into it and then apply it to the affected area,
Birch bud tincture is used in folk medicine - chicory: approximately one tablespoon of chicory should be diluted in a glass of boiling water, then left for several hours to allow the product to infuse. You can then rinse your mouth with it as needed.
- sage: dilute a few spoons in boiling water (one glass). After this, the broth should be left until it cools completely. The product can be used at intervals of 30 minutes until the condition normalizes,
- decoction of willow bark: pour 5 teaspoons of crushed willow root into a glass and pour hot boiled water. Afterwards, cool and use as intended, after diluting a little with warm water.
“Once in the winter I caught a toothache, and such an unpleasant nagging pain appeared. By evening it got worse. I remembered my grandmother’s old recipe - add a piece of lard. You won't believe it, but it worked! The next day, of course, I run to the dentist. It turned out to be caries, which is why the tooth gave such a reaction to the cold. But the lard saved me, I don’t know how, but it’s a fact.”
Olchik, from correspondence on the forum www.32top.ru
Remember: traditional medicine will help only in symptomatic therapy and only as support for the main treatment. With their help, it is impossible to eradicate the disease, and even if all the symptoms disappear, this will not eliminate the need to visit the dentist.
What treatment options can your dentist offer?
Let's consider what the doctor will do if it turns out that hypothermia, viral and infectious diseases have become catalysts for dental problems.
For caries, pulpitis, periodontitis
As a rule, in this case, the patient requires a competent endodontist dentist who will qualitatively clean, treat and seal the root canals of the diseased unit. If necessary, the specialist will also remove the pulp.
Depending on the severity of the pathology, treatment may require 1-3 or more visits to the clinic. So, during the conservative treatment of pulpitis (preserving the pulp) and periodontitis, the doctor will put medications and antibiotics into the canals, cover them with a temporary filling, and repeatedly take x-rays. Only after the source of infection has been completely eliminated will you be given a permanent filling. If a row element has been severely undermined by disease and destroyed, it may need to be strengthened with a pin and inlay, as well as an artificial crown.
Important! Today, better treatment of pulpitis, periodontitis, as well as cysts and other formations is facilitated by the use of modern optical technology, for example, a microscope. Using this device, the specialist sees all the branches of the root canals, completely removes the infection, hermetically seals and carries out highly aesthetic restorations.
For purulent formations
If it turns out that the pain is caused by flux, fistula, cyst, granuloma and abscess, then doctors will dissect the tissue and ensure the outflow of purulent contents using drainage, then apply sutures. During the rehabilitation period, the patient will be prescribed antibiotics, rinses, symptomatic treatment (painkillers, anti-inflammatory, wound healing), and physiotherapy.
For increased sensitivity
Strengthening procedures - remineralization and fluoridation - will help get rid of the consequences of consuming acidic drinks during the treatment of various diseases and eliminate the sensitivity of hard tissues. At home, it is recommended to consume more products with calcium, as well as purchase remineralizing pastes with fluoride, calcium hydroxyapatite, and beneficial natural ingredients (chamomile, propolis).
On a note! If there is increased sensitivity on units with crowns and fillings, then it is important to check the quality of adherence of the structures to the hard tissues and walls of the tooth. It is necessary to make sure that there are no cracks or chips, that the seal is not broken, and that the service life of artificial restorations has not come to an end, otherwise they must be replaced with new ones. It is also important to understand whether an inflammatory process has developed under the filling and crown, because then the product will have to be removed and the root canals treated using endodontics.
What to do is strictly contraindicated
We have figured out how and with what to treat an inflamed nerve, and now let’s move on to the question of what absolutely cannot be done if the neurovascular bundle is damaged. With this clinical picture, the pain can be very severe, and not all painkillers and anti-inflammatory solutions can relieve the disturbing symptom. Relying on self-medication in such a situation is strictly contraindicated. Even if you manage to relieve the discomfort, the pathology will continue to spread and destroy the internal structures of the tooth, which will ultimately lead to the need for its removal.
Under no circumstances should you apply a heating pad to an inflamed nerve.
You cannot self-prescribe antibiotics or any other medications, or use traditional medicine without first talking to your doctor. Also, you should not apply a heating pad to the sore spot - heat will only intensify the pain and provoke further spread of inflammatory processes.
Opening an abscess on the gum
The abscess is always opened. This reduces the risk of spontaneous opening, which can cause complications. The flux is opened under local anesthesia. If the patient has panic or other indications, the doctor may choose a different method of anesthesia.
A small incision is made on the anesthetized gum in the area of the gumboil, no more than 2 cm in length. After the dissection, the doctor completely cleans and sterilizes the purulent cavity and treats it with antiseptics. A crust should not be allowed to form in the area of the incision, as it will interfere with the outflow of ichor and purulent contents. To do this, a drainage is inserted into the incision. After the cavity is cleared of pus, you can begin general treatment, the purpose of which is to eliminate the causes that caused periostitis.
Preventive measures
Most often, the true cause of the problem is advanced caries, when the lesion penetrates deeper into the internal structures of the tooth and captures the nerve. As a result, any mechanical or temperature effect provokes severe pain, and sometimes can even aggravate the situation with complications. If the tooth is completely healthy, it is almost impossible to develop hypothermia due to prolonged exposure to low temperatures.
Preventative dental examinations will help avoid problems.
To protect yourself from problems with dental nerves, you need to treat any dental diseases in a timely manner. Better yet, do everything possible to prevent their development. In this regard, experts strongly recommend adhering to basic hygiene rules: brushing your teeth at least twice a day, using mouth rinses and visiting the dentist at least twice a year - for prevention and prophylaxis. hygiene. Conscientious implementation of these simple rules will help protect against most dental problems, including pulpitis, periostitis and periodontitis.
- Zoryan E.V., Rabinovich S.A., Matveeva E.G. Algorithm for choosing local anesthetic drugs, problems and solutions, 2008.
How to protect the dental nerve from hypothermia?
- During the cold season, use warm hats, scarves and outerwear with a high collar.
- In low temperatures and strong winds, it is advisable to cover your face with clothing.
- Do not use a thermos with hot water. Temperature changes may cause inflammation of the dental nerve and the appearance of an acute painful reaction.
Study the condition and appearance of your teeth, as well as the oral mucosa, regularly on your own. This way you can see suspicious changes in a timely manner.
Anatomy and functions of the trigeminal nerve
The trigeminal nerve belongs to the class of mixed nerves, including both sensory and motor fibers.
It is the largest of the 12 cranial nerves. This name of the nerve is due to the presence of three branches - the orbital, maxillary and mandibular nerves. When one of the branches of the trigeminal nerve is damaged, a sensitivity disorder occurs in the area of innervation. When the trigeminal nerve root is damaged, sensitivity disorder is observed in the areas of innervation of all three branches.