Causes of inflammatory damage to the trigeminal nerve
Factors contributing to inflammation of the trigeminal nerve are:
- surgical interventions on the jaw bones;
- fractures of the base of the skull, lower and upper jaws;
- tumors;
- complex tooth extraction;
- hypothermia;
- surgery on the maxillary sinus;
- improperly administered anesthesia;
- incorrectly performed dental prosthetics;
- metabolic disorders;
- the presence of foreign bodies that irritate the nerve trunk or injure nerve endings;
- bacterial or viral infection;
- various types of intoxication of the body;
- hypovitaminosis;
- weakening of the immune system.
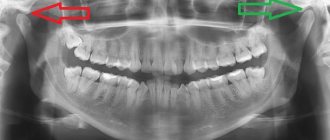
Diagnostics
A disease of the trigeminal nerve is diagnosed by a neurologist who, based on the patient’s complaints and examination results, identifies the cause of the disease. To diagnose trigeminal nerve disease, the neurologist prescribes a magnetic resonance examination, which can help detect vascular damage, as well as computed tomography, which allows you to examine the skull and see what changes are occurring in its bone structure.
Symptoms of trigeminal neuritis
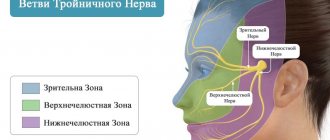
The maxillary trigeminal nerve consists of three types of nerve fibers:
- vegetative;
- motor;
- sensitive.
The symptomatic picture of neuritis may vary depending on which fibers were affected by the inflammatory process.
Damage to sensory fibers
In particular, with inflammation of the sensory fibers, the patient may complain of a tingling sensation, numbness, and weakened sensitivity in the area innervated by the trigeminal nerve.
Damage to motor fibers
When motor fibers are damaged, there is a partial or complete decrease in strength in the innervated muscles, their atrophy and deterioration of tendon reflexes.
Damage to vegetative fibers
When the vegetative fibers are inflamed, the patient experiences cyanosis and swelling of the skin, dryness and thinning of the skin, and the potential risk of developing a trophic ulcer increases.
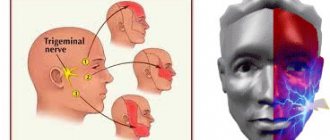
Pain due to inflammation
In addition, a disease such as inflammation or neuritis of the facial trigeminal nerve makes itself felt with attacks of pain of a very diverse nature:
- cutting,
- burning,
- pricking,
- tearing
- shooting, etc.
In this case, the area of pain does not always correspond to the area of innervation and can spread to the lower jaw, cheeks and chin.
Pain may be accompanied by:
- muscle spasms (facial, chewing),
- the appearance of nasal discharge,
- development of hypersalivation,
- increased lacrimation.
Lack of sensation in the tongue, lips and chin
With inflammatory damage to the trigeminal nerve, not only the entire nerve can be damaged, but also its individual branches. This is why numbness and pain can occur in various areas of the face. For example, when the lingual branch of the nerve is inflamed, patients complain of pain and sensitivity disturbances in the anterior part of the tongue, and when the mental branch is damaged, in the area of the lips and chin.
Pain when laughing, chewing, brushing teeth and shaving
Pain due to neuritis of the maxillary trigeminal nerve can intensify with touching, chewing, laughing and with changes in temperature. That is why patients, trying to prevent the recurrence of painful attacks, avoid excessive mobility and prolonged conversations, and refuse brushing their teeth and shaving.
Traditional medicine recipes
To treat the trigeminal nerve, doctors recommend trying special recipes from traditional medicine. Of course, they cannot help everyone and at the same time they will only relieve pain, but will not cure it completely. Therefore, if you experience any pain, you can try to relieve it at home and immediately go to the dental clinic for help.
So, the following recipes can help relieve pain:
- Compresses from boiled beets, which are grated on a coarse grater, add black radish juice and use the resulting mass to make a compress on the trigeminal nerve.
- Make a rinse using an infusion of chamomile and honey. Rinse your mouth with the prepared solution.
- Lotions made from horseradish grated on a coarse grater. You need to wrap the resulting mass in a clean cloth and apply it to the place where the pain occurs.
If pain occurs in the temporal part of the face, you should immediately make an appointment with a neurologist, who can determine the cause of the trigeminal nerve disease and prescribe appropriate treatment.
Treatment of neuritis of the maxillary trigeminal nerve
Therapy
The treatment program for trigeminal neuritis is drawn up taking into account the causes of the disease and its clinical signs. The main goals of treatment are:
- achieving a sensitizing effect;
- fight against bacterial and viral infection;
- increasing the body's immune forces;
- elimination of swelling of the nerve trunk;
- restoration of natural adaptive and compensatory reactions;
- normalization of the patency of nerve impulses.
Healing procedures
The set of procedures aimed at blocking the inflammatory process and eliminating all manifestations of neuritis includes:
- antibacterial therapy;
- antiviral therapy;
- elimination of factors contributing to the occurrence of intoxication;
- removal of tumor-like neoplasms or dissection of adhesions compressing the nerve;
- prescribing vitamin and mineral complexes to the patient;
- stimulation of nerves and muscles;
- acupuncture;
- physiotherapy (electrophoresis, phonophoresis, UHF, ultrasound, paraffin therapy).
People suffering from trigeminal neuritis are advised to regularly visit dental clinics and have their oral cavity sanitized.
Principles of treatment and management of patients with trigeminal neuralgia
Management tactics for patients with NTN should include:
- diagnosis of the disease, including general clinical, otolaryngological, dental and instrumental examinations;
- identification of etiological factors;
- conservative treatment;
- surgery.
The main goals of treatment for NTN are pain relief and prevention of disease relapse.
Conservative treatment involves medication and physical therapy.
In approximately 90% of cases of NTN, the use of antiepileptic drugs is effective. The first of these was phenytoin, but from 1961 to the present day, a more effective drug, carbamazepine, has been widely used, which is rightly considered the drug of first choice for the treatment of patients with NTN. The initial dose is 200–400 mg/day, gradually increased until pain stops, on average to 800 mg/day in 4 divided doses, and then reduced to the minimum effective dose. When treated with carbamazepine, pain can be relieved in 70% of cases.
Second-line drugs are phenytoin, baclofen, valproic acid, tizanidine, antidepressants.
For exacerbations of the disease, phenytoin is prescribed at a dose of 15 mg/kg IV drip over 2 hours once.
Baclofen is taken orally with meals. The initial dose is 5 mg 3 times / day, subsequent increase in dose - by 5 mg every 3 days until the effect is achieved, but not more than 20-25 mg 3 times / day. The maximum dose is 100 mg/day, prescribed for a short time in a hospital setting. The final dose is set so that when taking the drug, a decrease in muscle tone does not lead to excessive myasthenia gravis and does not impair motor functions. For hypersensitivity, the initial daily dose of baclofen is 6–10 mg, followed by a slow increase. The drug should be discontinued gradually over 1–2 weeks.
Valproic acid is prescribed as therapy for adults at an initial dose of 3–15 mg/day in 2 divided doses, regardless of meals. If necessary, the dose of the drug is increased by 5–10 mg/kg/week. The maximum dose is 30 mg/kg/day or 3000 mg/day. In combination treatment, adults are prescribed 10–30 mg/kg/day, followed by an increase of 5–10 mg/kg/week. If a decision is made to switch to intravenous administration of the drug, it is performed 4–6 hours after oral administration at a dose of 0.5–1 mg/kg/hour.
Tizanidine is prescribed orally. The dosage regimen is set individually. The initial daily dose is 6 mg (1 capsule). If necessary, the daily dose can be gradually increased by 6 mg (1 capsule) at intervals of 3–7 days. For most patients, the optimal dose of the drug is 12 mg/day (2 capsules). In rare cases, it may be necessary to increase the daily dose to 24 mg.
Amitriptyline is recommended to be taken orally after meals. The initial dose for adults is 25–50 mg at night, then the dose is increased over 5–6 days to 150–300 mg/day in 3 divided doses. Most of the dose is taken at night. If within 2 weeks. there is no improvement, the daily dose is increased to 300 mg. For elderly patients with mild disorders, the drug is prescribed at a dose of 30–100 mg at night. After achieving a therapeutic effect, switch to minimal maintenance doses – 25–50 mg/day. Amitriptyline is administered intramuscularly or intravenously in a dose of 25–40 mg 4 times a day, gradually replacing it orally. The duration of treatment is no more than 8–10 months. [RU. Khabriev, A.G. Chuchalin, 2006; A.S. Kadykov, L.S. Manvelov, V.V. Shvedkov, 2011].
Vitamin therapy is indicated, mainly the use of B vitamins. Combination preparations have proven themselves well.
Taking analgesics is considered ineffective. In addition, the use of large doses of these drugs, associated with the desire to quickly stop an attack, can lead to the appearance of abusive headaches.
Of the physiotherapeutic methods in the acute period of the disease and during an attack, moderate thermal effects are indicated: a Sollux lamp, an electric heating pad, ultraviolet irradiation of the diseased half of the face. Widely used diadynamic currents have an analgesic and anti-inflammatory effect. The course of treatment includes 6–10 procedures, which are carried out daily. They recommend 2-3 such courses with a break of 1 week. In addition, this procedure is carried out for 2–3 minutes on the area of the temporal artery and stellate ganglion. For persistent pain, procaine, tetracaine, and epinephrine are administered using diadynamic and sinusoidal modulated currents. The anesthetic effect is more pronounced than when using galvanic current. In case of long-term persistent pain syndrome or chronic course of the disease, increase the time of exposure to diadynamic currents to 8–10 minutes. The course of treatment includes 10–18 procedures with a 4-day break after 10 sessions.
For facial pain associated with cervical osteochondrosis and the sympathetic-radicular symptom complex, ultrasound exposure not only paravertebral, but also at the exit points of the trigeminal nerve for 2 minutes at each point every other day has a good effect. As a result of this effect, facial pain did not recur for 1 year after treatment [N.I. Strelkova, 1991]. Contraindications to ultrasound treatment are a tendency to nosebleeds, retinal detachment, acute inflammatory processes in the sinuses, middle ear, and cerebrovascular accidents. During ultrasound treatment, not only pain syndrome is reduced, but also regional and general vegetative-vascular disorders.
In the subacute period, in the presence of trigger zones, endonasal electrophoresis of a 4% procaine solution and a 2% thiamine solution is used, the duration of exposure is from 10 to 30 minutes. In addition, it can be performed in the form of a half mask and a Burgonier mask (for 2-sided nerve damage). Electrophoresis of diphenhydramine, pachycarpine hydroiodide, and platyphylline is also used on the affected side of the face. For arthrosis of the temporomandibular joint, electrophoresis of metamizole sodium and hyaluronidase is performed; for rheumatic etiology of the disease - salicylates; for malaria - quinine; for metabolic disorders - iodine and procaine.
The use of an ultrahigh-frequency electric field in an oligothermic dose is also effective.
In chronic forms of NTN, cervical osteochondrosis with facial pain of a trigeminal nature, facial massage is prescribed for 6–7 minutes daily or every other day. Mud applications on the collar area at a temperature of 36–37°C for 10 minutes have a positive effect. There are 10 procedures prescribed per course. Ozokerite, paraffin or peat are used. Balneotherapy is successfully used: sulfide, sea, radon baths. The beneficial effects of therapeutic exercises cannot be overestimated. Sanatorium-resort treatment in sanatoriums for patients with diseases of the peripheral nervous system is recommended in the warm season for chronic disease and rare attacks. Reflexology (acupuncture, moxibustion, laser therapy) has a positive effect.
If conservative therapy is ineffective or severe side effects of medications are observed, the need for surgical intervention is discussed.
Surgery. In 1884, American surgeon D.E. Mears, with chronic NTN, first removed his ganglion. In 1890, the English surgeon W. Ros and the American surgeon E. Enderus independently developed a special method for removing the Gasserian ganglion, which entered the practice of neurosurgeons at the end of the 19th and beginning of the 20th centuries. Currently, the following surgical methods are used for NTN:
- microsurgical decompression of the nerve exiting the brainstem;
- partial sensory rhizotomy;
- peripheral block or transection of the nerve proximal to the Gasser ganglion;
- neurectomy;
- cryosurgical methods;
- diathermocoagulation;
- high frequency radiation.
The most common modern effective methods of surgical treatment of NTN are microvascular decompression and destructive puncture operations. Among the destructive operations included in the arsenal of surgical interventions for NTN, there are percutaneous high-frequency selective rhizotomy (HFSR), balloon microcompression and glycerol rhizotomy.
The most common destructive method is PHR, which is a controlled thermal destruction of the Gasserian ganglion, which prevents the transmission of sensory impulses and the development of pain paroxysms. The location of the electrode is controlled in relation to the portions of the node. This method is successfully used in leading clinics dealing with the problem of pain [Grigoryan Yu.A., 1989; Broggi G. et al., 1990; Taha JM et al.,1995].
Significant experience with PHR has been accumulated at Mayfield Clinik Chincinati MD John Tew. In this clinic, more than 3 thousand patients were operated on using this method. Good results were obtained in 93% of patients. Relapses of pain within 15 years were observed in 25% of patients. Relapses of the disease during the first 5 years were observed in 15% of patients, before 10 years – in 7%, and from 10 to 15 years – in 3% of patients. There is a direct relationship between the severity of hypalgesia after percutaneous rhizotomy and the frequency of relapses of pain and dysesthesia. When mild hypalgesia was achieved after surgery and observed for 3 years, the frequency of pain recurrence reached 60%, while dysesthesia was observed in 7% of patients. When severe hypalgesia was achieved and patients were observed for 15 years, the frequency of pain recurrence was 25%, the probability of dysesthesia increased to 15%. When complete analgesia was obtained after percutaneous rhizotomy and patients were observed for 15 years, the rate of pain recurrence was observed in 20% of cases, and the number of dysesthesias increased to 36%. Thus, the most favorable option is the second option – achieving pronounced hypalgesia.
Unfortunately, patients with advanced forms of NTN are often admitted to neurosurgical departments, including after numerous destructive procedures. This undoubtedly worsens the functional result of neurosurgical interventions and in some cases requires complex and more dangerous operations at the level of the central nervous system [Ogleznev K.Ya., Grigoryan Yu.A., 1990].
The advantages of PHR: bloodlessness, speed and safety of the intervention, local anesthesia for pain relief and, finally, a high percentage of positive results. FSHR of the Gasserian ganglion for NTN and cluster headaches is a highly effective and safe method of surgical intervention.
Course and prognosis. Exacerbations of the disease most often occur in spring and autumn. In the absence of relapses, the prognosis is favorable.