Trophic ulcers are a complication of varicose veins, which is why they are sometimes called varicose veins. Occurs in eight out of ten patients with chronic venous insufficiency of the extremities. In terms of the general population, every thousand people suffer from ulcers due to varicose veins on the legs. In Moscow, with a population of 12.5 million people, at least 12,000 residents have varicose ulcers (the same number of residents in Suzdal).
Once a trophic ulcer occurs, it constantly progresses and without proper treatment leads to a persistent decrease in living comfort. In advanced cases, it can lead to disability and loss of limb.
Causes of formation of varicose ulcers
The main reason for the formation of ulcers on the legs with varicose veins is a violation of the trophism (nutrition) of tissues. The veins cannot cope with their work and expand under the influence of excess blood pressure. Blood stagnates, tissues do not receive oxygen and nutrients. Gradually, the process spreads, nerve fibers atrophy, and sensitivity is impaired.
Trophic ulcers in varicose veins are divided into primary (true) and secondary. True ones form on the wall of the dilated vein. The triggering factor is the rupture of a varicose vein and a violation of the integrity of the skin.
Secondary ones arise above the affected vein, where tissue trophism is significantly impaired. Any damage to the legs can trigger a dangerous process - an abrasion, scratch, chafing, bruise or scratch.
The situation can be aggravated by a sedentary lifestyle, prolonged sitting, working on your feet, frequent hypothermia of the feet, heavy lifting and even smoking. Complications can also arise from wearing tight or narrow shoes.
Stages of development of ulcers with varicose veins
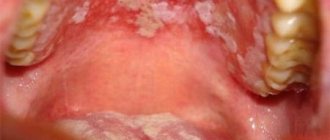
Varicose ulcers of the extremities develop gradually. First, the skin over the varicose vein changes color to intense pink, and then purplish-red. Later, the skin becomes shiny, smooth, thin and dry, and begins to itch and flake. Microcracks appear, which soon transform into erosion. Without treatment, they progress, growing in depth and breadth, gradually capturing subcutaneous fat, muscles, tendons and even the periosteum. Ulcers with varicose veins on the legs look scary and are prone to suppuration. The developing infectious process aggravates the patient's condition.
Get an online consultation
right now.
Get
Pre-ulcerative stage of varicose veins . With intact skin, a place with reduced sensitivity is detected. The area of skin over varicose veins reacts little to pain, cold or heat, pressure and injections. At the same time, tingling and twitching sensations (convulsions) periodically appear in the area of the legs and feet. A little later, part of the skin of the leg, where the varicose veins are, becomes smooth and shiny. This is caused by further trophic disorders, swelling of the subcutaneous adipose tissue. As the veins continue to dilate, the pressure increases, the skin, experiencing strong tension, stretches and becomes thinner. The affected area first turns pale, then becomes bluish, and then turns red. The patient experiences burning and itching. On a red background, you can see dark dots (exudate sweating) and necrotic pale spots.
Stage of formation of trophic ulcers . In place of whitened spots and microtraumas, ulcers are formed - round-shaped erosions with a tendency to spread. They “grow” both in depth and in breadth. They can unite and merge into a common wound surface. There is a high risk of bacterial infection.
Purification stage . Ulcers on the legs deepen and take on a characteristic shape with jagged edges. The skin around them rises due to swelling, becomes bright purple, and peels off. A bloody exudate with an unpleasant odor is released from the wound surface. If an infection occurs, the discharge becomes purulent and can be very copious. Sometimes additional defects appear nearby - the trophic ulcer spreads, affecting neighboring areas.
Necrotic stage . The process is progressing. The ulcers merge into one necrotic, smelly wound. The infection spreads and general intoxication occurs. Body temperature rises to 39ºС, headache, chills occur, lethargy and weakness increase. Necrosis involves muscles and bones. The person experiences severe pain. There is a high probability of developing wet gangrene, which almost always ends in amputation of the limb. Otherwise, the patient faces death.
Complications arise from untimely medical care, in advanced cases. These include:
- gangrene - tissue necrosis that spreads quickly,
- sepsis - "blood poisoning"
- thromboembolism - the formation of a blood clot in the affected vein and its separation with drift into the vessels of the heart, lungs or brain.
All these complications of varicose veins are deadly. They can be avoided by consulting a doctor in time, identifying the disease and undergoing a full course of treatment.
Diagnosis of ulcers in varicose veins
Phlebologists deal with the problems of varicose veins. Where there are no phlebologists, surgeons help with varicose veins of the extremities. Trophic ulcers on the legs with varicose veins look so characteristic that the doctor makes the diagnosis during an examination of the patient. Additional research methods are used to clarify the stage of the disease and assess how deep the varicose ulcer is. For this purpose, angiography, venography and, in some cases, magnetic resonance imaging (MRI) are used. Clinical and biochemical blood tests allow us to assess the general condition of the body in order to plan appropriate therapy.
To fully treat trophic ulcers, the doctor collects a complete “dossier” of the disease: he specifies the time of the first signs of leg disease, what treatment methods were used and how they helped. The doctor is interested not only in the immediate location of the pathology, but also in the general condition of the body. After a thorough examination, an examination is prescribed. How wide it will be depends on many factors. After the doctor collects the necessary data, a final diagnosis will be made and a treatment plan drawn up. The doctor will discuss the target dates, when approximately the ulcers on the leg should clear and heal.
How to remove scars from acne and chickenpox -
Acne and chickenpox scars are atrophic (minus tissue), although keloid scars can sometimes occur after severe forms of acne. Scars after acne (as well as scars after chickenpox) are defects of the dermis and, accordingly, methods affecting the dermal layer of the skin will be used to correct them. According to the accepted international classification, all atrophic scars are divided into 3 main types -
- “ice pick” type scar,
- rolled scar,
- carriage-shaped scar.
The division of scars into types has clinical significance, because Different treatment methods show different effectiveness when dealing with different types of atrophic acne scars. Ice pick scars are narrow, deep, sharply defined scars, the bottom of which can reach deep layers of the dermis or even subcutaneous tissue. Rolled scar (also called groove-shaped) - has the appearance of a deep, long groove with a width of 4 to 5 mm.
Carriage-shaped scars are round to oval-shaped depressions with sharply defined vertical edges. According to statistics, “ice pick” scars make up about 60-70% (of the total number of acne scars), carriage-shaped scars - about 20-30%, knurled - about 15-20%. Chickenpox scars are exactly the same as acne scars and will be treated accordingly. Below we will focus on the most effective methods, but first we will list methods that are definitely not worth wasting time and money on.
Useless and of little use methods -
- special creams for scars such as contractubex or any other (just zero effect),
- cosmetics with retinoids and vitamin C (can only be used as a preparatory stage for hardware methods),
- filler injections (expensive, and the effect is temporary).
Conservative treatment
During treatment, trophic ulcers are treated with antiseptic and antibacterial agents: solutions, gels, ointments, dressings. In case of infection, antibiotics are prescribed in tablet or injection form.
After cleansing the ulcerative bottom, the trophic ulcer is treated with agents that enhance regeneration and restore trophism. To improve the tone of the veins, elastic bandaging is used. Maintenance therapy is prescribed: vitamins, venotonics, restoratives. Physiotherapy in this case is an auxiliary method that helps improve blood microcirculation and tissue nutrition. The most commonly used are laser therapy, magnetic therapy, and infrared radiation.
The wound must be clean
In a purulent wound there may be scabs, necrosis, crusts, fibrin (this is yellow dense tissue on the wound), then such a wound must be cleaned. Cleansing can be achieved using Neofix FibroGel AG, IntraSite Gel and IntraSite Conformable hydrogels. The main purpose of these gels is to moisten necrosis and crusts, loosen them, which facilitates easier removal of necrosis during subsequent dressings. Hydrogels are applied directly to the wound in sufficient quantities so that the wound is completely covered with hydrogel; the hydrogel layer must be at least 5 mm. Next, the wound must be covered with a film dressing, for example OpSite Flexigrid, or one of the postoperative dressings OpSite Post-Op, PRIMAPORE, NEOFIX Post. On top of the gels, you can use absorbent dressings Allevyn Adhesive or Allevyn Sacrum, which are preferable and more convenient to use in the treatment of bedsores, since these dressings have a sticky edge and a soft spongy pad. After a maximum of three days, it is necessary to bandage, remove the hydrogel from the surface of the wound, and along with it the softened necrosis and crusts. If there are areas of necrosis or stupa remaining in the wound, then it is necessary to use the hydrogel more than once until the wound is completely cleansed. The advantage of using the antimicrobial hydrogel Neofix FibroGel AG for these purposes is that this hydrogel contains silver. This antimicrobial component fights any infectious agents in the wound. As a result of the use of hydrogels, the wound is cleaned. Dressings must be carried out at least once every 1-3 days, and preferably under the supervision of the attending physician.
Surgery
For life-threatening complications of varicose veins, the presence of a large area of skin ulceration, or a deep wound, surgical treatment is used. The ulcer is cleaned mechanically using curettes (wound curettage), vacuuming or VAK therapy. In severe cases, the affected area is excised and the defect is covered with a skin graft from the patient's thigh. Sometimes additional blood vessels are inserted to not only remove the defect, but also restore blood supply. After the operation, the patient undergoes a course of rehabilitation, after which he returns to his normal life.
Laser facial resurfacing –
There are a huge number of types of lasers that can be used to correct acne and chickenpox scars, but we will try to systematize this information. All lasers for scar correction can be divided into 2 main categories (each of which in turn is divided into two more):
- ablative (traditional and fractional),
- non-ablative (traditional and fractional).
a) The best ablative lasers –
Ablative lasers seem to evaporate the surface layers of the skin, but at the same time they also affect the dermis, stimulating the formation of collagen in it. Those. The term “ablative” means that the laser action involves permanent damage to the surface of the skin. Traditional ablative CO2 lasers are extremely effective for correcting atrophic scars (50–80% improvement in scar condition is achieved after only 1 procedure), but such lasers have a high risk of complications and side effects.
This is due to the fact that traditional ablative lasers operate in continuous resurfacing mode (i.e., total damage to the entire surface of the skin in the treated area occurs). Due to the large number of side effects and long rehabilitation period, fractional type ablative lasers were developed. Their peculiarity is that they damage the skin fractionally (fragmentally), i.e. Between the damaged areas of the skin, intact areas remain, which will contribute to much faster healing.
One of the best ablative fractional CO2 lasers can be called “AcuPulse” (Lumenis, Israel), it operates with a wavelength of 10,600 nm. There are also ablative fractional erbium lasers (Er: YAG) - with a wavelength of 2940 nm. The effectiveness of CO2 and Er:YAG lasers is almost comparable, however, both of them may require 2-3 procedures (while a traditional ablative laser may require only 1 procedure).
I would like to note that the ablative fractional laser “AcuPulse”, if necessary, can also work in the mode of total resurfacing of the skin flap (i.e., act not as a fractional laser, but as a traditional one).
a) Non-ablative lasers (traditional and fractional) –
Non-ablative lasers (unlike ablative lasers) cause thermal damage only to the dermis and deep layers of the epidermis, and no damage to the superficial stratum corneum of the epidermis occurs at all. They stimulate the formation of new collagen in the dermis - as a result of which the scar rises to the surface. We have already said above that non-ablative lasers are also divided into traditional and fractional.
When we talked about the treatment of post-inflammatory erythema, we already talked about pulsed dye lasers (585 or 595 nm), KTP lasers 532 nm, and Nd:YAG lasers 1064 nm. They are precisely non-ablative traditional lasers. But besides them, it should also include Nd:YAG lasers 1320 nm, as well as diode lasers 1450 nm. Absolutely all of these lasers have approximately the same efficiency, which is quite modest.
Clinical studies show that after 1 treatment, the condition of scars improves by only about 20-30%. This means you may need 3 to 5 treatments to get optimal results. Of course, the effectiveness of non-ablative traditional lasers is much less than ablative lasers (both traditional and fractional). Well, the last type of lasers that we want to talk about are non-ablative fractional lasers, which include, for example, the FRAXEL RE:STORE laser.
Non-ablative fractional lasers differ from traditional lasers in that thermal damage to the dermis and deep layers of the epidermis occurs fractionally (i.e., there will be undamaged areas between the damaged areas). "FRAXEL RE:STORE" is an erbium fiber laser with a wavelength of 1550 nm. Clinical studies show that acne scars improve by approximately 50% after 1 treatment.
FRAXEL: before and after photos
A few important points regarding laser resurfacing -
You should understand that laser resurfacing will show different effectiveness for different types of atrophic scars. The main indications for laser resurfacing will be carriage-shaped and groove-shaped (knurled) scars. For example, if we take the FRAXEL RE:STORE laser, then on carriage-shaped scars it can show an improvement of up to 50% (for 1 procedure), groove-shaped scars - only up to 40%, and on scars of the "ice pick" type - there will be only improvement up to 25%.
The same will apply to any other type of laser, i.e. on scars of the “ice pick” type - any type of laser resurfacing will a priori be less effective. Therefore, you should understand that the number of laser resurfacing procedures that may be required will depend not only on the type of laser, but also on the type of atrophic scars on your skin. Carriage-shaped scars after acne are always easier to correct (as are scars after chickenpox).
Prevention of varicose ulcers after treatment
If the goal of treatment is achieved: blood flow is restored, adequate tissue nutrition is restored and the cause of the disease is eliminated, the risk of complications is minimal. However, the patient should remember that his future fate depends on himself. You need to lead a healthy lifestyle and constantly monitor the condition of your blood vessels. For this:
- take medications prescribed by a doctor,
- eat right (exclude fast food, alcohol, animal fats and simple carbohydrates),
- avoid excessive physical activity,
- perform a complex of physical therapy,
- wear compression stockings on the lower extremities,
- choose comfortable shoes,
- come regularly for medical examinations (twice a year),
- undergo specialized sanatorium-resort treatment.
Compliance with the doctor-prescribed regimen, nutrition and physical activity will help avoid relapse of a trophic ulcer. By contacting the A. Begma Medical Center regarding varicose veins, you can get a detailed consultation with a phlebologist, clarify the condition of the veins, get rid of trophic ulcers and make sure they never bother you.
Using the Dermapen device or mesoscooter –
Dermapen works great where there is “minus tissue”, i.e. with atrophic scars. This is a fractional device that, using the mechanical movements of a nozzle with needles, causes microdamage to the skin. And the skin naturally reacts to damage by regeneration, i.e. collagen synthesis is stimulated. Depending on the number, depth and type of atrophic scars, the course of treatment may require from 3 to 6-8 procedures.
The first results can be seen 6-8 weeks after the first procedure, and the final result can be assessed only 3 months after the last procedure. The same applies to any other methods (for example, laser resurfacing). This is due to the fact that stimulation of collagen production in response to skin damage is delayed in time and increases gradually.
Dermapen: before and after photos
The mesoscooter is a cheaper alternative to the Dermapen device. It works on the same principle - it leaves microdamages in the skin, but the damage is no longer applied strictly vertically, but at a changing angle (since the mesoscooter drum with needles rotates). This is not very good and can lead to roughening of the skin due to the production of abnormal scar collagen. Below you can see photos before and after 3 procedures performed at an interval of 4 weeks.
Mesoscooter: before and after photos
How to increase the effectiveness of these methods -
The effectiveness of using a dermapen or mesoscooter can be increased if you undergo special training. Clinical studies have shown that if the patient used topical retinoids for at least 1 month (optimally 2-3 months), the effectiveness of the method increased significantly. As retinoids you can use: products with pure retinol (at least 0.3-0.4% and up to 1%), as well as tretinoin 0.025%.
Products with the L-form of ascorbic acid with a concentration of 15% (instead of retinoids) can also be used, because they also stimulate collagen production in the skin. Another preparation option is injection mesotherapy in a cosmetologist’s office. In this case, several procedures are first carried out using nucleotides (DNA-RNA complexes) - an excellent Italian drug for this is “Plinest”. After this, several injection procedures with complexes containing matrikin peptides (they stimulate collagen production).
After such an injection preparation of 4-6 procedures, we move on to the dermapen or mesoscooter itself. We hope that our article: How to get rid of acne spots, acne scars and chickenpox was useful to you!
Sources:
1. Textbook of dermatology “Fitzpatrick's Dermatology” (8th edition), 2. American Academy of Dermatology (USA), 3. National Library of Medicine (USA), 4. “Cosmetic dermatology” (Bauman L.). 5. Clinical studies published at https://www.ncbi.nlm.nih.gov/.