* The price of endotracheal anesthesia is included in the cost of the operation
Some general information about anesthesia methods. Anesthesia can be local or general. Local anesthesia is used for minor surgical procedures. For example, when removing papillomas, wen and moles, or when reinforcing the face. With local anesthesia, the patient is conscious, but the operation area completely loses sensitivity.
General anesthesia is necessary for long and complex operations. During general anesthesia, the patient is immersed in a state of drug-induced sleep, and vital functions - breathing, cardiac activity - are controlled by an anesthesiologist. Anesthesia is always general anesthesia. The terms “local anesthesia” or “general anesthesia” are meaningless, although they can sometimes be found in publications and in everyday speech.
What is endotracheal anesthesia?
There are two types of general anesthesia - intravenous and inhalation anesthesia. In the first case, medications that put a person to sleep are administered intravenously by the anesthesiologist. During inhalation anesthesia, drugs enter the body with inhaled air in gaseous form.
Inhalation anesthesia can be performed using a mask or intubation technique. The mask technique involves the supply of oxygen and anesthesia drugs through a special mask and does not require insertion of a breathing tube into the trachea. With the intubation technique, a tube is inserted into the trachea, through which oxygen and anesthetic substances are supplied, and carbon dioxide is removed.
Endotracheal anesthesia is a technique of inhalation anesthesia, a variant of general anesthesia, in which during surgery the supply of medications and external breathing are carried out through a special tube inserted into the upper respiratory tract, that is, into the trachea.
Combined endotracheal anesthesia is a separate method of general anesthesia, in which anesthesia drugs are administered both intravenously and through the respiratory tract. In other words, it is a combination of intravenous and inhalational anesthesia.
How is endotracheal anesthesia performed?
Preparation for surgery consists of several stages. The preparatory stage is premedication. Before surgery, the patient is given sedatives - tranquilizers, drugs with anxiolytic effect. Taking sleeping pills the evening before surgery is also part of the preparatory phase. Thanks to premedication, a person approaches surgery in a calm and balanced state.
Immediately before the operation, induction anesthesia is performed - intravenous administration of sedatives, which ensures smooth falling asleep before intubation begins. The next stage is muscle relaxation. When the patient falls asleep, he is given a small dose of muscle relaxants - drugs that help relax the muscles. Thanks to muscle relaxants, the tone of the laryngeal muscles is reduced and optimal conditions are created for the insertion of an endotracheal tube.
The fourth stage is the direct insertion of the endotracheal tube and its connection to the ventilator. At this stage, the patient is already sleeping and dreaming, and nothing bothers him.
How cancer and radiation therapy may affect swallowing
Depending on the size and location of the tumor, radiation therapy may weaken the muscles and organs involved in swallowing. They also may not work as well as they did before radiation therapy began. This may make it difficult for you to eat and drink.
Radiotherapy may cause:
- pain when swallowing;
- wounds (inflammation of the mucous membrane) in the mouth and throat;
- dry mouth.
- unusually thick saliva;
- swelling.
- Change in taste sensations
These symptoms usually appear 1-2 weeks after starting radiotherapy. These symptoms may become worse during treatment. Most symptoms will begin to subside approximately 2 to 4 weeks after treatment ends.
Radiation therapy can also cause permanent tissue scarring. The impact of such scars depends on which area is being treated. Some examples of the effects of scarring are described below.
- The muscles that attach to your jaw may tighten, making it difficult for you to open your mouth and chew food. This is called trismus.
- Your salivary glands may not produce enough saliva. This may make swallowing more difficult because your mouth will be too dry.
- The muscles in the tongue and back of the throat may also lose mobility. This may make it more difficult for you to push food or liquid down your throat and open your esophagus.
- The muscles that help protect the airway when swallowing may weaken. They may not be strong enough to prevent food or liquid from entering the airways.
- The esophagus may narrow. For this reason, food may get stuck in the back of the throat.
Not all patients will necessarily have all of these problems. Your treatment will be planned to reduce the likelihood of these problems occurring. Your healthcare team will also teach you techniques that can help you cope with these problems.
Other treatments may also affect swallowing. The surgery may affect areas of the mouth and throat, which may make swallowing difficult. Some chemotherapy drugs can cause sores in the mouth and throat. This can make swallowing painful.
to come back to the beginning
Advantages of endotracheal anesthesia
Maximum safety and complete control over the depth of drug-induced sleep are the main advantages of endotracheal anesthesia. The risk of “waking up during surgery” is eliminated, as is the slightest possibility of disruption of the respiratory and cardiovascular systems. In other words, this is the safest and most reliable type of general anesthesia, during which the anesthesiologist has everything under control!
The advantages of endotracheal anesthesia are explained by the fact that, thanks to intubation, continuous monitoring of respiratory function is carried out. The anesthesiologist constantly monitors adequate ventilation of the lungs, accurately doses the amount of oxygen entering the lungs, and carefully controls the carbon dioxide content in the exhaled air.
From a safety point of view, one more point is important - the risk of tongue retraction, which is present with intravenous and mask anesthesia techniques, is eliminated. In addition, the endotracheal tube completely isolates the respiratory tract from the esophagus, which eliminates the possibility of saliva and stomach contents entering the pulmonary system.
Other features and advantages of endotracheal anesthesia are the possibility of active use of muscle relaxants, the possibility of performing long-term operations with artificial ventilation, and minimizing the risk of postoperative complications from the respiratory and cardiovascular systems.
Treatment of laryngeal injuries
First of all, in case of injuries to the larynx, the patient needs to restore respiratory function; in some cases, anti-shock measures or stopping bleeding may be necessary. If the patient’s condition is stable, therapy is carried out, which consists of relieving the inflammatory process, pain, eliminating swelling, conducting antibacterial, detoxification and infusion treatment.
The patient is advised to rest his voice; if the larynx is poorly obstructed, the patient is fed through a tube. For cartilage fractures, ligament ruptures, extensive injuries, bleeding, stenosis or emphysema, surgical treatment is performed. Surgical treatment includes removal of a foreign body, reconstructive surgery to restore the organ, prosthetics and plastic surgery of the organ and nearby tissues, etc.
After eliminating the clinical symptoms of damage to the larynx, the patient is recommended to be treated by a phoniatrist to restore speech function.
If you receive a laryngeal injury, in order to avoid dangerous complications, you must consult a doctor as soon as possible. Paid services of an otolaryngologist in medical institutions are an opportunity to receive qualified and timely assistance from specialists at any convenient time. You can make an appointment by calling: 8 (812) 322-93-07, 8 (812) 611-08-26.
Endotracheal anesthesia - indications
In plastic surgery, endotracheal anesthesia is used for many operations.
Examples include rhinoplasty, augmentation mammoplasty, abdominoplasty, mastopexy, circumferential facelift and SMAS platysmaplasty. Liposuction can also be performed using an intubation technique, although local anesthesia may be chosen for smaller cases. Endotracheal anesthesia is indicated for all long-term operations accompanied by a violation of the integrity of deep tissues, not only the skin. This is how a general rule can be formulated. Minor surgical interventions are often performed under local anesthesia. Examples are otoplasty for protruding ears, bullhorn (a type of lip surgery) or lipoma removal.
Tonsil removal methods
In modern otorhinolaryngology, there is a wide choice of tonsillectomy techniques.8
Classic method of removing tonsils
Removal of tonsils occurs by bluntly separating the tonsil tissue along with the capsule from the surrounding tissues using a rasp.
The separation of the tonsil is completed using a wire loop. The bleeding is stopped, the vessels are cauterized using an electrosurgical method (electrocoagulation). This operation takes from 15 to 40 minutes.9 Today, this operation is used in ENT practice more often than others. The operation can be performed under general or local anesthesia.
The only disadvantage of this method, unlike others, is the highest risk of bleeding. However, the operation is fairly routine and, relative to the number of operations performed, the risks of complications are low.
Laser method for tonsil removal
When removing tonsils, a laser beam is used to destroy and coagulate tissue. The laser beam coagulates the blood at the incision site and seals the blood vessels, which prevents bleeding. The laser method is less traumatic and has a lower risk of complications. Also, in this way it is possible both complete removal of the palatine tonsils and their partial excision.
Radio wave method for removing tonsils (using the Surgitron device)
Tissue excision occurs using a radio signal, which is transmitted by an electrode and causes the evaporation of intracellular fluid and tissue dissection.
The advantage of this method is that thermal damage to tissue is several times lower than when using laser or electrosurgical methods. There is less tissue injury, as a result of which the patient experiences less pain in the postoperative period; the level of tissue regeneration is maintained. Complete tissue healing occurs without the formation of a rough scar.
Cryodestruction
This method of removing tonsils involves local exposure to liquid nitrogen using a special nozzle.
The nozzle is selected individually, taking into account the peculiarities of the anatomy, since its contact with the palatine tonsil must be especially clear and dense for a more effective effect. Cryotherapy causes microcirculation disturbances, which ensures the absence of bleeding during and after surgery. This method is painless and bloodless, and does not form a rough scar. The method is recommended for patients with an increased risk of bleeding, severe heart failure and pathology of the endocrine system.
After endotracheal anesthesia
The final stage of general anesthesia is the removal of the patient from the state of drug-induced sleep. After endotracheal anesthesia, some confusion is observed, which is explained by the residual effect of sedatives on the central nervous system. Possible headaches, mild dizziness and nausea are associated with this. However, the features of modern anesthesia drugs are such that while the patient may be bothered by their residual effect, he is in a state that resembles euphoria. And when the euphoria wears off, the “echoes” of anesthesia also disappear.
A specific phenomenon after endotracheal anesthesia is a slight sore throat, sore throat, and possibly a cough. These consequences are explained by the fact that the endotracheal tube irritates the mucous membrane of the larynx and trachea. As a rule, the discomfort goes away within a day.
Relief of pain symptoms in children after tonsillotomy
One of the most common diseases of the ENT organs in childhood, diagnosed according to some data in more than 50% of preschool children [1], is hypertrophy of the palatine tonsils. The high prevalence of this condition in children is associated with a high frequency of surgical interventions on the tonsils, in our country this is mainly tonsillotomy. In Russia, tonsillotomy accounts for 25–30% of planned surgical interventions in a children's hospital [2]. According to foreign authors, the share of tonsillotomy (adenotonsillotomy) in those countries where this intervention is practiced in the structure of surgical interventions in otorhinolaryngological departments is more than 55% (for the age group of patients from 1 to 3 years). The main indication for tonsillotomy is obstructive sleep apnea syndrome [3].
Among the most common complications in the early postoperative period during tonsillotomy and other surgical interventions on the tonsils are bleeding and severe pain, which should not be underestimated in pediatric practice. Thus, according to recent studies, complications in the early postoperative period in patients after surgical interventions on the organs of the lymphopharyngeal ring in 48.1% were severe sore throat, and bleeding was noted only in 3.9% of cases. In 29.0% of patients, severe sore throat was the cause of severe dysphagia, and in 4.6% it was clinically manifested by dehydration [4]. In children under 6 years of age, pain in the throat in the early postoperative period is mainly accompanied by nausea and vomiting [5].
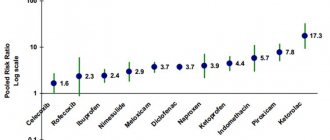
Thus, one of the pressing problems of all modern clinical medicine and otorhinolaryngology in particular is postoperative pain relief. When analyzing previously published materials, one cannot fail to note the particularly great importance of non-steroidal anti-inflammatory drugs in minimizing pain after surgery on the tonsils [6].
The drug lysine salt of ketoprofen, which has anti-inflammatory, analgesic and antipyretic properties, with a rapid onset and duration of action of up to 8 hours, combined with very good tolerability, is of certain interest in terms of pain relief [7]. According to comparative randomized clinical studies of ketoprofen, lysine salt in a dose of 50–100 mg has a stronger analgesic effect than paracetamol/codeine combinations [8].
Taking into account the above problem, a clinical study was conducted at the clinical sites of the Department of Pediatric Otorhinolaryngology of the Federal State Educational Institution of Further Professional Education of the Russian Medical Academy of Postgraduate Education, the purpose of which was to increase the effectiveness of pain relief after tonsillotomy in children.
The study included 140 children aged 6 to 18 years (mean age 9.49 years) after radiowave tonsillotomy under endotracheal anesthesia. As a premedication before surgery, patients received only atropine solution (sublingually). In all patients, tonsillotomy (in 121 patients in combination with adenotomy using the Kozlov-Karpov method) was performed using a radio wave surgery device. A direct incision through the tissue of the palatine tonsil was made using a monopolar needle electrode in the “cut and coagulation” mode. Non-steroidal anti-inflammatory drugs were prescribed to relieve pain in the early postoperative period. All children, according to the sequential number randomization method, were divided into four groups.
Patients of the 1st group (35 people) received the drug ketoprofen lysine salt in the form of an oral solution (OKI drug, produced by Dompe, Italy) 40 mg (children aged 6 to 14 years) or 80 mg (children over 14 years old) and older) if there are complaints of severe, unbearable sore throat with an interval between doses of the drug of at least 8 hours.
Patients of the 2nd group (35 people) received the drug ketoprofen lysine salt in the form of an oral solution (OKI drug, produced by Dompe, Italy) 40 mg (children aged 6 to 14 years) or 80 mg (children from 14 years old and older) 3 times a day (at least 8 hours between doses) for 3 days after surgery.
Patients of the 3rd group (35 people) received ibuprofen orally (Nurofen, syrup 100 mg/5 ml, manufactured by Reckitt Benckiser Healthcare International Ltd., UK) 100-300 mg (child weight 17-20 kg - 150 mg each ; child weight 21-30 kg - 200 mg; child weight 31-40 kg - 300 mg) up to 3 times a day if there are complaints of severe, unbearable sore throat.
Patients of the 4th group (35 people) received the drug ketoprofen lysine salt in the form of a solution for topical use (OKI drug, produced by Dompe, Italy) 4 ml (children aged 6 to 12 years) or 6 ml (children over 12 years old) and older) 2 times a day (morning and evening) for 3 days after surgery. A single dose of rinsing solution was diluted in 100 ml of drinking water immediately before use. The patient performed the first gargling with this solution 3 hours after surgery, regardless of the severity of the pain syndrome.
Control examinations of patients were carried out 3, 6 hours after surgery, on the 1st, 2nd and 3rd days after surgery.
The study did not include children with diseases and conditions that are a contraindication for the prescription of the drug ketoprofen lysine salt in the form of granules for the preparation of an oral solution (for patients of the main groups) and ibuprofen (for patients of the control group), as well as patients with concomitant diseases, changing, in the opinion of the researcher, the natural course of the disease, affecting the result of therapy and/or violating the possibility of subjective assessment of the symptoms of the disease (psychoneurological pathology, diabetes mellitus, blood diseases, oncological diseases, immunodeficiency states, infectious diseases, etc.).
The evaluation of the effectiveness of treatment was carried out by the curator personally, noting the patient’s condition at the agreed time, entering into the primary documentation (inpatient card) the frequency of vomiting, the presence of nausea and the presence of bleeding from the surgical field. If bleeding occurred in the early postoperative period, the doctor carried out a set of measures to achieve stable hemostasis. If a patient vomits more than 2 times and severe nausea, the patient was given a single intravenous injection of metoclopramide solution (based on the patient’s body weight); if vomiting occurs more than 3 times, infusion therapy with glucose-saline solutions was performed.
Starting from the first day after surgical treatment (3 hours after surgery), the patient independently subjectively assessed the severity of pain in the throat and nausea on the basis of a 10-point visual analogue scale, where “0” points were the absence of a symptom, “10” points - maximum severity of the symptom. Patients of the 1st and 2nd groups, when taking the drug ketoprofen lysine salt in the form of an oral solution for the first and second time, assessed the ability to swallow the medicine (they could or not) and the organoleptic properties of the drug (whether they liked the taste or not). Patients of the 4th group, during the first and second gargling with a solution of ketoprofen lysine salt, assessed the possibility of using this form of medication and the organoleptic properties of the drug (whether they liked the taste or not).
The assessment of the safety of therapy was carried out by assessing the patient’s condition in a timely manner, noting in the primary documentation (inpatient card) the corresponding changes in the patient’s condition (the appearance of pathological elements on the skin, diarrhea, nausea, shortness of breath, etc.). On the 2nd day after surgery, all patients underwent capillary blood sampling for a general clinical blood test.
Statistical processing of the results was carried out using the Statistica v.6.0 program. To compare quantitative characteristics, Student's t-test was used, and to compare qualitative characteristics, Pearson's c2 test was used. The difference was considered statistically significant at p < 0.05.
Results and discussion
According to the visual analogue scale (VAS), at the first examination after surgery, patients of all groups had the same severity of sore throat (p > 0.05). This indicator was 6.4 ± 0.3 points in patients of the 1st group, 6.8 ± 0.5 points in the 2nd group, 6.2 ± 0.4 points in the 3rd group, 4th groups - 6.5 ± 0.5 points. Nausea and vomiting were noted in the 1st group in 7 (20%) people, in the 2nd group - in 8 (22.9%), in the 3rd - in 6 (17.1%) and in the 4th group - in 8 (22.9%) people. There was no bleeding in any patient. In the 1st group, 17 (48.6%) patients asked for an anesthetic drug, in the 3rd group - 14 (40%) patients.
During the control examination 6 hours after surgery, the severity of sore throat was 4.2 ± 1.2 points in patients of the 1st group, 1.6 ± 0.8 points in the 2nd group, 1.6 ± 0.8 points in the 3rd group - 4.8 ± 1.4 points, in group 4 - 3.4 ± 1.2 points. There was no statistically significant difference in indicators (p > 0.05). At the second examination (6 hours after surgery), 9 patients of the 1st group and 13 patients of the 3rd group asked for an anesthetic drug. However, none of the patients in groups 2 and 4 asked the doctor for an anesthetic during the follow-up examination.
During a control examination 6 hours after surgery, complaints of nausea and vomiting were reported by 9 (25.7%) patients of group 1 (all did not receive painkillers after the first examination), 1 (2.9%) patient of group 2, 11 (31.4%) patients (8 of them did not receive pain medication at the initial examination) of the 3rd group and 4 (11.4%) patients of the 4th group. 2 out of 3 patients of the 3rd group, who continued to have nausea after taking ibuprofen syrup, noted that a feeling of nausea arose after taking the drug. None of the patients had bleeding.
When examining patients 24 hours after surgery, according to VAS data, the severity of sore throat in patients of the 1st group was 3.5 ± 0.8 points, in the 2nd group - 1.2 ± 0.4 points, in 3 in group 4.5 ± 0.8 points, in group 4 — 3.2 ± 0.6 points. The severity of pain in patients of group 2 was significantly less than in patients of groups 1, 3 and 4 (p < 0.05). The difference between VAS scores for the severity of sore throat between patients of groups 1, 3 and 4 was not statistically significant (p > 0.05). One day after the operation, 1 (2.9%) child from the 1st observation group and 2 (5.7%) patients from the 3rd group complained of nausea. None of the patients had bleeding.
When examining patients 48 hours after surgery, according to VAS data, the severity of sore throat in patients of group 1 was 2.7 ± 0.6 points, in group 2 - 0.8 ± 0.2 points, in group 3 in group 3.6 ± 0.5 points, in group 4 — 2.5 ± 0.6 points. The severity of pain in patients of group 2, as at the previous examination, was significantly less than in patients of groups 1, 3 and 4 (p < 0.05). The difference between VAS scores for the severity of sore throat between patients of groups 1, 3 and 4 was not statistically significant (p > 0.05). No child complained of nausea. None of the patients had bleeding. According to the results of a clinical blood test taken on the second day after surgery, no pathological changes were detected in any patient under our supervision.
When examining patients 72 hours after surgery, according to VAS data, the severity of sore throat in patients of group 1 was 1.4 ± 0.5 points, in group 2 - 0.4 ± 0.05 points, in group 3 in group 1.8 ± 0.5 points, in group 4 — 1.4 ± 0.4 points. The severity of pain in patients of group 2, as at the previous examination, was significantly less than that in patients of groups 1, 3 and 4 (p < 0.05). The difference between VAS scores for the severity of sore throat between patients of the 1st, 3rd and 4th groups is not statistically significant (p > 0.05). No child complained of nausea. None of the patients had signs of bleeding.
According to the results of a follow-up examination of patients 10 days after surgery, not a single patient had complaints of bleeding from the oropharynx. None of the patients complained of discomfort in the throat. A retrospective assessment by patients (or their official representatives) of the ease of use of the drug ketoprofen lysine salt in the form of granules for the preparation of an oral solution (patients of the 1st and 2nd groups) showed that all patients noted the ease of use of this dosage form and only 3 ( 8.6%) patient of the 1st group and 1 (2.9%) patient of the 2nd group described the taste of the drug as “unpleasant”. However, this did not affect the possibility of further use of the drug. A similar survey of patients of the 4th group who used gargling with a solution of ketoprofen lysine salt for pain relief showed that 28 patients (80%) found this form of use convenient, while the remaining 7 patients were also able to use this form of the drug as prescribed by the doctor. Moreover, all 7 patients who noted some inconvenience in using this form of the drug were under the age of 10 years. The organoleptic properties of the rinse solution were rated as “pleasant” by 30 (85.7%) patients.
conclusions
Based on the above, we can conclude that in patients who have undergone radio wave tonsillotomy, a course of ketoprofen lysine salt solution for oral administration in the early postoperative period has an advantage over a single use (in the presence of severe sore throat) of this form of the drug or ibuprofen syrup according to effectiveness in relieving pain in the throat. A course of oral administration of a solution of ketoprofen lysine salt can reduce the frequency of complaints of nausea on the first day of surgery.
The form of the drug solution of ketoprofen lysine salt for gargling with a course of use in the early postoperative period in this category of patients gives an effect in reducing sore throat, comparable to a single oral administration of painkillers used during observation, but is inferior to the analgesic effect of a course of use of a ketoprofen solution lysine salt for oral administration. Also, this form of the drug is not always convenient for use in children under 10 years of age.
None of the patients under observation showed signs of serious adverse drug reactions from the use of the above-mentioned drugs, requiring the patient to be excluded from the study and provided with appropriate medical care. Complaints of a number of patients about nausea and vomiting are probably related to the anesthesia treatment the child underwent, since they were noted in patients of the 1st and 3rd groups, regardless of the fact that an anesthetic was used. However, in some cases, nausea cannot be ruled out as a consequence of taking an anesthetic drug.
The results of our observation in comparison with the available literature data allow us to conclude that a course of use in the early postoperative period of a solution of ketoprofen lysine salt for oral administration in patients who have undergone radio wave tonsillotomy has an advantage over a one-time use (due to severe sore throat) of a similar drug, ibuprofen syrup and ketoprofen lysine salt solution for gargling. At the same time, the subjectivity of a number of criteria for assessing the effectiveness of these drugs determines the relevance of further study of the issue of the peculiarities of the use of non-steroidal anti-inflammatory drugs in the early postoperative period in children after surgical interventions on the organs of the lymphopharyngeal ring.
Literature
- Dashevskaya N. D. Health status of preschool children before entering school. Materials of the IX Congress of Pediatricians of Russia. 2001: 176–177.
- Karpova E. P., Tulupov D. A., Zyabkin I. V., Naumov O. G., Kerchev B. I. On the issue of indications for adenotomy in children // Russian Rhinology. 2010;3:48–49.
- Borgström A., Nerfeldt P., Friberg D., Sunnergren O., Stalfors J. Trends and changes in pediatric tonsil surgery in Sweden 1987–2013: a population-based cohort study // BMJ Open. 2017; 7(1):e013346. DOI: 10.1136/bmjopen-2016–013346.
- Muninnobpamasa T., Khamproh K., Moungthong G. Prevalence of tonsillectomy and adenoidectomy complication at Phramongkutklao Hospital // J Med Assoc Thai. 2012; Suppl 5:S69–74.
- Sidorov V. A., Agavelyan E. G., Mikhelson V. A., Leshkevich A. I., Grabovskaya V. A., Zyabkin I. V., Shcheglov A. O., Korotkova P. V. Modern approaches to conducting anesthesia in pediatric ENT surgery // Anesthesiology and Reanimatology. 2005; 1:4–9.
- Nosulya E.V., Kim I.A. Tonsillectomy: modern possibilities of postoperative pain relief // Medical Council. 2014; 15:36–40. DOI: https://dx.doi.org/10.21518/2079–701X-2014–15–36–41
- Borsa M., Tonon GC, Ronchi C., Zanolo G., Canali S. Pharmacokinetics of a slow-release preparation of ketoprofen lysine in man. // Arzneimittelforschung. 1983; 33(10):1497–1500.
- Messeri A., Busoni P., Noccioli B., Murolo S., Ivani G., Grossetti R., Gallini C., Maestri L., Fedele G., Novellini R. Analgesic efficacy and tolerability of ketoprofen lysine salt vs paracetamol in common pediatric surgery. A randomized, single-blind, parallel, multicentre trial // Paediatr Anaesth. 2003; 13(7):574–578.
E. P. Karpova, Doctor of Medical Sciences, Professor D. A. Tulupov1, Candidate of Medical Sciences V. A. Grabovskaya F. A. Fedotov
Federal State Budgetary Educational Institution of Further Professional Education RMANPO Ministry of Health of the Russian Federation, Moscow
1 Contact information
Relief of pain symptoms in children after tonsillotomy / E. P. Karpova, D. A. Tulupov, V. A. Grabovskaya, F. A. Fedotov
For citation: Attending physician No. 1/2018; Page numbers in the issue: 22-25
Tags: children, tonsils, postoperative period
Complications of endotracheal anesthesia
Any surgical intervention is associated with the risk of postoperative complications. The goal of using endotracheal anesthesia is to minimize this risk. Thanks to the intubation technique for administering medications, the risk of aspiration of gastric contents into the lungs is reduced, the risk of respiratory tract infection, and the risk of respiratory or cardiovascular failure is minimized.
Complications of endotracheal anesthesia, that is, complications caused by the insertion of an endotracheal tube, are extremely rare. These include injuries to the tongue or larynx, which occur during intubation “on the go” before urgent (urgent) operations. During planned surgical interventions, which include all plastic surgeries, there are no complications of endotracheal anesthesia.
Conclusion
Based on the statistical analysis of the comparison of two groups of patients who underwent bilateral tonsillectomy, in patients who received, in addition to the anesthetic drug ketorolac, Arnica Montana C9 (BUARON) for resorption, 5 granules 3 times a day from the 2nd day, the recovery time was significantly reduced . This is indicated, in particular, by a faster time for normalization of body temperature, disappearance of pain and a decrease in the inflammatory reaction in the pharynx after tonsillectomy. This may have a positive effect on the quality of life in the early postoperative period of patients taking the drug Arnica Montana C9 (BOIRON).
The authors declare no conflict of interest.
The authors declare no conflicts of interest.
Endotracheal anesthesia - contraindications
Endotracheal anesthesia has become very widely used in all branches of surgery, largely due to the fact that it has practically no contraindications. Intubation technology allows for complete control of vital functions; it can even be used to perform 16-hour heart surgeries.
In the context of plastic surgery, endotracheal anesthesia has no contraindications. Why? Because intubation cannot be used only for certain conditions in which any operation not related to the elimination of an immediate threat to life is contraindicated. For example, endotracheal anesthesia is contraindicated in case of myocardial infarction or pneumonia, but no one would even think of undergoing plastic surgery.
To learn more about the anesthetic techniques used for a particular plastic surgery procedure, book a free consultation with a Soho Clinic surgeon.
Dietary recommendations
A balanced diet is an important part of cancer treatment. If you have pain when swallowing or have trouble swallowing:
- You may not be able to eat enough food. This may cause you to lose weight or have low energy.
- You may not be able to drink enough fluids. This can lead to dehydration.
Your swallowing specialist, nurse, doctor, and clinical dietitian dietitian will tell you what you should eat and drink during treatment. Your swallowing specialist will recommend foods and liquids that have the right consistency. When you try new foods and liquids, make sure they are the consistency recommended by your swallowing specialist.
Your healthcare team may also recommend that you take a nutritional supplement (such as Ensure®) to increase your calorie intake. You can buy dietary supplements at your local grocery store, pharmacy, or order online.
For more dietary advice, see Eating Well During Cancer Treatment and Guidelines for Puréed and Soft Diets.
Control dry mouth or thick saliva
Try the following tips if dry mouth or thick saliva is bothering you:
- Drink 8–10 cups of fluid per day. Getting enough fluid in your body will help make your saliva thinner.
- Carry a bottle of water or other liquid with you when you leave the house. Take small sips of it often.
- Chew sugarless gum or suck on sugarless hard candies. This may stimulate saliva production.
- Add sauces, gravies and other liquids to food.
- Use a humidifier to help thin your saliva and other secretions.
- Rinse your mouth frequently throughout the day with a mixture of 1 liter (about 4.5 cups) of water, 1 teaspoon of salt and 1 teaspoon of baking soda. You can drink the mixture in small sips, rinse your mouth with it, or gargle.
to come back to the beginning