Recently, there has been a significant increase in the number of chronic diseases of the salivary glands [3, 9, 11-13]. It has been shown that the salivary glands are in close relationship with other organs and tissues of the body. Therefore, it is believed that pathological processes in the salivary glands (sialoadenitis and sialadenosis) and some diseases of the body have common, genetically determined causes and congenital prerequisites [9].
Often the pathological process in the salivary glands becomes chronic, which is accompanied by dysfunction of the salivary glands, dystrophic changes in the parenchyma, and disruption of the blood flow system. In order to establish the picture of pathological changes in the salivary glands, sialography and sialometry are used. The Doppler ultrasound method has great advantages for functional diagnostics, which allows one to evaluate the blood flow of the desired area [8]. Also, for the purpose of diagnosing diseases of the salivary glands, indicators of mixed and/or ductal saliva are used, which most likely at all stages of the examination make it possible to assess the degree of inflammatory reaction in the salivary glands and the effectiveness of the proposed treatment method over time. Obtaining saliva samples, unlike blood plasma, is affordable and does not cause discomfort to the patient. To assess the course of the inflammatory reaction in mixed saliva, they examine exactly those indicators that are characteristic only of inflammation and appear in saliva from blood plasma. These indicators can act as reliable criteria for existing problems in the tissues of the salivary glands.
In 1993 prof. V.V. Afanasyev [1] proposed an optimal treatment regimen for sialadenosis and sialadenitis, based on the pathogenetic mechanisms of the development of the process. It includes: 1) increasing general and local immunity; 2) strengthening the function of the salivary glands; 3) treatment of concomitant diseases aggravating diseases of the salivary glands.
However, in outpatient practice the proposed methods are not always taken into account, and treatment of inflammatory diseases of the salivary glands is carried out according to a standard scheme, using only antibiotics and anti-inflammatory drugs. In some cases, if therapeutic measures are ineffective, surgical intervention is performed, including removal of the salivary gland [2]. Publications on the use of homeopathic medicines in dentistry to relieve inflammation and restore the function of oral tissues have begun to appear more often in the literature [4-7, 10]. Antihomotoxic therapy is also recommended for the treatment of chronic sialadenitis in the initial stage of exacerbation [3]. However, the authors consider the use of Traumeel S injections to be ineffective for sluggish and protracted processes in the salivary glands. Thus, due to the increasing number of chronic forms of diseases of the salivary glands and the ineffectiveness of their treatment, it is necessary to introduce new treatment procedures aimed at preserving the function of the salivary gland and restoring its structure.
Based on the above, the purpose of this study is to evaluate the effectiveness of treatment of the salivary glands with complex antihomotoxic therapy using modern diagnostic models.
Classification of sialadenoses
According to the state of the salivary gland, sialadenoses are defined as interstitial, parenchymal and ductal (depending on the predominant changes detected using private and special examination methods). This disease has three stages of development:
- initial (I degree), in which the salivary glands are not enlarged and have normal sizes;
- the stage of pronounced clinical changes (II degree) is accompanied by a slight increase in the size of the salivary glands, which is determined by palpation;
- late (III degree) is characterized by an increase in the size of the salivary glands, which is diagnosed both visually and by palpation.
In addition, sialadenoses are divided into endocrine, neurogenic, allergic and associated with nutritional disorders. In order to determine the degree of development of sialadenosis, a specialist assesses the size of the major salivary glands, taking into account examination and palpation data.
Reasons for the development of sialadenoses
Sialadenosis can be caused by both physiological reasons and the pathological condition of the patient, namely:
- pregnancy;
- breastfeeding;
- alcohol abuse;
- endocrine system disorders;
- diabetes mellitus;
- menstrual irregularities (hypermenstrual syndrome);
- prostatitis;
- chronic pancreatitis;
- autoimmune diseases (rheumatoid arthritis, systemic lupus erythematosus, scleroderma, psoriasis, Sjogren's disease, Mikulicz's disease, etc.);
- decreased nutrition due to anorexia nervosa.
Patients may also develop allergic sialadenoses when taking certain medications. Sialadenosis may occur after surgery on the salivary gland or after injury to it. The main and most common cause of sialadenosis in patients who suffer from alcoholism is liver cirrhosis. There are also frequent cases of the development of sialadenoses of unknown origin in patients who do not have any systemic diseases. In this case, the patient undergoes an examination to identify a general disease. The mechanism of development of this pathology in medical practice is not entirely clear. But in medicine there are such factors for the manifestation of this disease as:
- neuropathy, which is accompanied by the destruction of nerve fibers;
- disturbances in the microcirculatory system and lipid oxidation, which leads to damage to cell tissue;
- congenital expansion and violation of the architectonics of the ductal system.
These processes cause functional failure and replacement of glandular tissue with adipose tissue.
Symptoms of sialadenoses
Typically, during the development of sialadenosis, patients experience swelling in the area of the salivary glands, which is not accompanied by pain. The enlargement of the salivary glands persists for a long time; their size does not change when eating. With sialadenosis, salivation is often reduced. When examining the patient, a moderate amount of squamous epithelium is observed in the secretion and a change in the configuration of the face, which is caused by symmetrical swelling of the soft tissues. In this case, the enlarged glands have a dense shape to the touch, with a smooth surface. In turn, the manifestation of parenchymal sialadenosis is accompanied by dilation of the excretory ducts. A relative sign of interstitial sialadenosis is narrowing of the excretory ducts. Ductal sialadenosis is accompanied by a stricture of dilated ducts. Sometimes disturbances in the excretory and secretory functions of the salivary glands occur without their visible increase. These conditions are also classified as sialadenoses as a reaction of the parenchyma to various changes in the body: they are manifested by increased or decreased salivation. An increase in the secretion of the salivary glands (hypersalivation) is associated with diseases such as stomatitis, gastric and duodenal ulcers, helminthiasis and even toxicosis during pregnancy. Reduced secretion (hyposalivation) leads to dry mouth, or more precisely to xerostomia. The symptom of dry mouth is often observed in patients with various diseases of the salivary glands and body systems.
Results and discussion
At the time of treatment, patients complained of pain and swelling in the area of the causative salivary gland. In the case of inflammation of the submandibular salivary gland, patients indicated pain when swallowing. From the anamnesis it follows that the day before all patients were exposed to hypothermia. Objectively: in the area of the causative salivary gland, symptoms of edema and hyperemia of the skin were noted, with bimanual palpation - severe pain. Body temperature ranged on average from 37.5 to 38.5 °C. When examined from the oral cavity, swelling and hyperemia were revealed; a small amount of saliva was released from the mouth of Wharton's duct, and in some cases pus mixed with blood; probing was difficult. According to the results of Doppler ultrasound: the gland is enlarged in size, decreased echogenicity, the parenchyma is heterogeneous, the duct is dilated, stones are not detected. Color Doppler mode: diffuse enhancement of parenchymal vascularization. Examination of mixed saliva showed the presence of albumin in an amount of 15.3 ± 6.87 mg/ml and an increase in IgG to 16.5 ± 3.44 mg/ml.
Repeated examination of all patients after the prescribed treatment on the 7th day showed a decrease in pain. This coincided with a decrease in local inflammatory phenomena and a decrease in the size of the salivary gland. The Doppler ultrasound also confirmed the results of the clinical examination in both groups of patients, i.e., a decrease in the size of the examined salivary glands, the excretory ducts are not dilated. During these periods, the echogenicity and heterogeneity of the parenchyma of the inflamed salivary gland remained reduced compared to the contralateral side. In the mixed saliva of patients of both groups on the 7th day after treatment, a significant decrease in albumin level was observed ( p
<0.05). The greatest decrease in the content of this protein in saliva occurred in patients of the 2nd group, for whom antihomotoxic therapy was included in complex treatment (4.24±0.67 mg/ml versus 5.67±0.32 mg/ml in patients of the 1st group ). At the same time, a decrease in the IgG content in saliva was determined to 8.90 ± 2.40 mg/ml in patients of the 1st group and to 9.23 ± 1.23 mg/ml in the 2nd group.
1 month after treatment, 3 (27.3%) patients of group 1 were treated for exacerbation of chronic sialadenitis, which required surgical intervention. In the remaining patients, there was an improvement in the function of the salivary glands over time, and there were no complaints of pain. An ultrasound examination showed that in 5 patients of this group there was still a slight increase in the size of the damaged gland and there was echogenicity and heterogeneity of the parenchyma. Traces of albumin were detected in the mixed saliva of these patients.
Patients of group 2, who took antihomotoxic drugs, had no complaints after 1 month, clinically no changes were detected in the inflamed gland, functional activity was normal, which was confirmed by ultrasound data. Albumin was not detected in mixed saliva, and IgG was detected in trace amounts.
We present a clinical case.
To the specialized department of the Department of Maxillary Surgery of the CS MGMSU named after. A.E. Evdokimov was contacted by patient K.
, 35 years old, with complaints of pain in the submandibular region on the right, the presence of edema and slight pain when swallowing. From the anamnesis: the day before the patient became hypothermic. Objectively: in the submandibular region on the right there were signs of swelling and hyperemia of the skin, with bimanual palpation - severe pain. Body temperature 38.5 °C. Local status: Wharton's duct on the right is swollen and hyperemic, a small amount of saliva was released from the mouth, probing is difficult. The albumin content in mixed saliva is 12.3 mg/ml, IgG 9.47 mg/ml. The patient underwent an ultrasound scan, which resulted in a diagnosis of parenchymal sialadenitis of the submandibular salivary gland on the right (Fig. 1).
Rice.
1. Doppler ultrasound before treatment. Sialadenitis of the right submandibular salivary gland. a — B-mode: the gland is enlarged in size, decreased echogenicity, the parenchyma is heterogeneous, the duct is dilated, stones are not detected; b — color Doppler mode: diffuse enhancement of parenchymal vascularization; c — B-mode: the left submandibular gland is not changed. Treatment: the patient was prescribed standard antibacterial and antispasmodic therapy (enhanced amoxicillin at a dose of 625 mg, 1 tablet 3 times a day, 5 days; drotaverine, 1 tablet 2 times a day, 5 days). On the 7th day after the course of treatment with allopathic drugs, no improvement was noted. The ultrasound results did not reveal positive echographic dynamics in the condition of the right submandibular salivary gland.
In this regard, the patient was additionally prescribed antihomotoxic therapy according to the following regimen: Traumeel C, 1 granule 3 times a day and lymphomyosot, 15 drops 3 times a day for 24 days; spascuprel 1 tablet 2 times a day, 5 days. 7 days after the prescription of antihomotoxic drugs, the patient noted a significant improvement in her health in the form of a decrease in pain and inflammation. Albumin and IgG were detected in trace amounts in mixed saliva. It was recommended to continue antihomotoxic therapy with dynamic ultrasound monitoring, which showed positive echographic dynamics (Fig. 2).
Rice. 2. Ultrasound results after 14 days (a) and 60 days (b) from the start of treatment. B-mode: a — the size of the right submandibular salivary gland has decreased, the duct is not dilated; there remains a decrease in echogenicity and heterogeneity of the gland parenchyma; b — right submandibular gland of normal echogenicity and structure, the duct is not dilated; a slight increase in size remains compared to the contralateral side.
Diagnosis of sialadenoses
During the examination of a patient with suspected sialadenosis, the doctor conducts a survey, examination and palpation of the salivary glands. After which the patient undergoes clinical and biochemical blood and urine tests to study the parameters of carbohydrate metabolism. In order to exclude the inflammatory and tumor process of changes in the salivary glands, the patient undergoes an ultrasound of the salivary glands. This makes it possible to determine their increase, heterogeneity of the parenchyma, increase or decrease in echogenicity. In addition, an X-ray examination is performed. With sialography, the patient can detect dilation or narrowing of the salivary ducts, slowing down the removal of the radiocontrast drug from the gland. A radiosialogram also reveals a decrease in the secretory ability of the salivary glands. In order to detect a bilateral increase in the volume and density of the gland and thereby exclude tumor lesions, the patient undergoes a computed tomography scan.
In addition, to diagnose sialadenosis, sialometry, cytological examination of duct secretions and biochemical examination of saliva are performed. The diagnosis of sialadenosis is confirmed by aspiration or incisional biopsy of the salivary glands. Histological examination reveals an increase in the acini in the patient, the presence of dystrophic changes in them, and the absence of inflammatory infiltration.
In order to determine the nature of the diseases accompanying sialadenosis, the patient may be referred for consultation to specialists. As part of diagnostic measures, other possible causes of enlargement of the salivary glands are excluded: sialadenitis, mumps, tumors and cysts of the salivary glands, stones of the salivary glands.
Material and methods
In the specialized department of the Department of Maxillofacial Surgery (MCS) at the Dentistry Center (DC) of the Moscow State Medical and Dental University (MGMSU) named after. A.I. Evdokimov examined and treated 25 people aged 25 to 50 years with chronic parenchymal sialadenitis. The criterion for inclusion in the study was the presence of chronic parenchymal sialadenitis. The criterion for non-inclusion was the presence of concomitant pathology in the acute or exacerbation stage. The exclusion criterion was the refusal of patients to further participate in the studies. To make a diagnosis, all patients underwent a clinical examination, which included examination and palpation of the altered salivary gland, determination of its size and amount of secretion, and collection of anamnesis about concomitant diseases.
All patients also underwent high-resolution ultrasound (US) in B-mode and color Doppler mapping mode on a Philips iU-22 ultrasound scanner using linear scanning sensors with a frequency of 5-17 MHz. Additionally, mixed saliva was collected from patients for 5 minutes into a sterile plastic tube with a tightly screwed cap. The samples were centrifuged and the content of albumin protein (in mg/ml) was determined in the supernatant of saliva using the spectrophotometric method and the amount of immunoglobulin (Ig) G using the enzyme-linked immunosorbent method. The initial data of ultrasound Dopplerography and mixed saliva were compared with the results of the study on the 7th day and 1 month from the beginning treating patients.
According to the method of the proposed treatment, the patients were divided into two groups. Patients of group 1 ( n
=11) carried out standard antibacterial and antispasmodic therapy
per os
for 5 days with the following drugs: enhanced amoxicillin 625 mg, 1 tablet 3 times a day, drotaverine 1 tablet 2 times a day.
Patients of the 2nd group ( n
= 14), along with standard therapy, were prescribed
per os
complex antihomotoxic therapy with Traumeel S, 1 granule 3 times a day and lymphomyosot, 15 drops 3 times a day for 24 days, spascuprel, 1 tablet 2 times a day for a course of 5 days. All manipulations were carried out only after the informed consent of the patient, signed by him and the attending physician in duplicate. The rationale for the use of these homeopathic drugs was that Traumeel S is a highly effective remedy for inflammatory processes, the drug spascuprel has an antispasmodic, analgesic, sedative and anticonvulsant effect, the drug lymphomyosot improves the microcirculation of peripheral vessels. All obtained digital values were processed by the method of variation statistics using the Statistica 8.0 program.
Treatment methods for sialadenosis
Treatment of sialadenosis is quite difficult, since various therapeutic measures aimed at reducing the size of the glands are not always successful. However, for the symptomatic treatment of sialadenosis, methods such as:
- acupuncture;
- courses of novocaine blockades to inhibit the increased tone of the sympathetic nervous system.
Physiotherapy methods are also used in the treatment of sialadenosis, namely:
- novocaine electrophoresis;
- galvanization in the area of the salivary glands and cervical sympathetic ganglia;
- pulsed magnetic therapy;
- laser therapy on the area of the salivary glands;
- galvanic collar;
- infiltration of the subcutaneous base of the parotid glands with weak solutions of novocaine;
- hyperbaric oxygenation.
The treatment method for sialadenosis also includes oral and parenteral medications and vitamin E, as well as intravenous administration of rheopolyglucin and hemodez solutions. In the absence of satisfactory results of conservative therapy, surgical treatment may be indicated. The prognosis and prevention of sialadenosis depend entirely on the underlying disease.
Sialadenitis
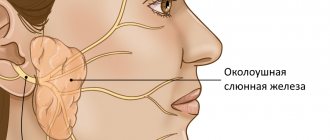
What is sialadenitis?
The salivary glands contain a network of tiny tubules called ducts.
Saliva enters the mouth through them. If the flow of saliva slows or stops for any reason, bacterial growth can occur in the “stagnant” saliva. This infectious disease is called sialadenitis. The most commonly inflamed glands are the parotid glands (in front of the ear) and the submandibular glands (under the chin). Inflammation is often caused by the bacteria Staphylococcus aureus. Sialadenitis occurs most often with a combination of the following factors:
• Old age (over 50 years).
• Weakened state after illness or dehydration.
• Dry mouth (xerostomia).
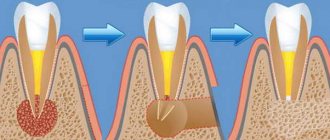
Saliva production sometimes decreases during illness or after surgery, as well as in old age. The formation of stones (sialolith) or twisting of the duct leads to stagnation in the salivary gland. In some diseases, such as Sjögren's syndrome, saliva production decreases, causing sialadenitis. People undergoing cancer treatment are also susceptible to this infection.
Symptoms
Sialadenitis appears as a swelling, painful lump in the cheek or under the chin. Pus may leak through the gland into the mouth. The spread of infection is indicated by fever, chills and general malaise.
Diagnostics
During an external examination, the dentist will detect swelling in the area of the salivary gland. If there is pus, you will be tested for bacteria. You may be referred for other tests and examination of your salivary glands and ducts.
Expected duration of illness
Sialadenitis is usually cured within one week. But a mild or untreated infection can become chronic (long-term). In this case, treatment lasts from several weeks to several months, with temporary deterioration of the condition.
Prevention
Always drink plenty of fluids. This is especially important after surgery, during illness and in old age.
Treatment
The first step is to ensure your body has enough fluids. You may be given fluids intravenously. The doctor will prescribe antibiotics to kill the bacterial infection.
Once fluid balance is restored, your doctor will recommend eating foods that stimulate saliva secretion, such as sugar-free sour candies and chewing gum.
If the infection cannot be cleared with medication, surgery may be required to open the ducts or remove the stones.
When to see a doctor
According to information on the website of the Russian Dental Association, sialadenitis is treated by a dentist. Additionally, to find out the causes of the disease, you may need to consult other specialists. If you notice redness and painful swelling in front of the ear or under the chin, contact your dentist, especially if you are at risk for developing sialadenitis.
Forecast
With prompt diagnosis and intensive treatment, the outcome of sialadenitis is favorable in most cases.