The proportions of the face largely depend on the condition of the parotid salivary glands, which for various reasons can increase in size, swell and create not only aesthetic problems, but also health problems.
The parotid salivary glands, or rather their unhealthy condition, affect the proportions of the face. this creates aesthetic problems, and can also significantly affect the health of the entire body. The main problem of the parotid glands is the occurrence of a tumor. Outwardly, this is a small swelling, which cannot be immediately noticed, but when palpated, a small formation with clear boundaries appears. As a rule, this type of tumor does not bother the patient in any way, and not everyone notices it right away.
Most of these manifestations do not become a threat to humans, since the tumor is benign. However, there are also situations when the tumor literally becomes larger and larger in a matter of days. in this case, the status of the tumor changes to malignant and requires immediate contact with a specialist for removal of the formation.
Removal of parotid tumor
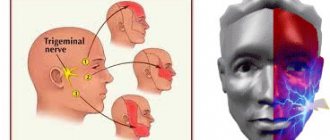
At the ART Clinic, under the guidance of Professor Nerobeev, operations of the parotid salivary gland are performed. This type of surgical intervention presents certain difficulties that should only be trusted to professionals. The gland contains branches of the facial nerve, which should not be touched under any circumstances. If this happens, then the person who came for help may be left with a distorted face for the rest of his life.
Unfortunately, not all doctors work honestly, and in some cases they ask you to sign a paper that describes the possible consequences in advance. This indicates the unprofessionalism of the surgeon who is not ready to take responsibility.
Treatment of a tumor of the parotid salivary gland at the ART Clinic means reliable staff, high-quality equipment and the best techniques. Before undergoing any surgery, you must schedule an initial consultation for examination. Remember that even if there is no discomfort or pain, a tumor of the parotid gland still requires examination.
Would you like more information about surgery in our clinic? We are ready to answer any questions by phone, as well as in the feedback form. You can find out the cost of the operation on our website or during your first visit.
Pleomorphic adenoma (mixed tumor). This benign tumor is the most common, occurring in 72% of all epithelial tumors of the salivary glands. In terms of frequency of lesions, the parotid salivary gland is in first place, the mucosalivary glands of the palate are in second place, then, respectively, the submandibular, sublingual and minor salivary glands, glands of the lip, cheek, and tongue.Pleomorphic adenoma grows painlessly, slowly, over several years and can reach large sizes. When the adenoma is localized in the parotid salivary gland, paresis of the facial muscles is not observed. Upon examination, a tumor is detected in the area of the salivary gland, mobile, often with a bumpy surface. Its consistency is densely elastic, sometimes with areas of softening due to the mucus-like component. The skin above it does not change, it folds freely. The salivary function of the affected gland is usually not affected. Pleomorphic adenoma has a capsule, but may not be completely encapsulated, in which case the tumor cells penetrate into the adjacent glandular tissue. This explains tumor recurrences after extracapsular removal. Sometimes tumor growth accelerates significantly (within 1 month), and pain may appear. Such symptoms are characteristic of tumor malignancy; in such cases it is interpreted as carcinoma in pleomorphic adenoma.
The diagnosis of a tumor is clarified by cytological examination of the punctate, which is obtained in the needle in the form of a crumbly whitish mass.
Macroscopically, pleomorphic adenoma is a tumor in a thin translucent capsule, on a section in the form of a pasty mass of white-gray color with areas of mucus and compaction.
Microscopically, the tumor, in addition to pronounced epithelial tissue, contains mesenchyme-like areas consisting of myxoid or cartilage-like structures, the presence of which is explained by the accumulation of mucoid or hyaline substance between the myoepithelial cells.
Treatment is surgical. If the tumor is localized in the submandibular and sublingual salivary glands, the tumor is removed along with the gland. Tumors located on the palate, cheek, lips, tongue are excised within unaffected tissues. The peculiarity of the operation on the parotid salivary gland is associated with the branching of the facial nerve in the thickness of the gland. The nature and extent of surgical intervention depend on the size and location of the tumor. In all cases, it is necessary to excise the tumor with adjacent glandular tissue. Some authors suggest extracapsular tumor removal. When the tumor is localized in the lower pole of the gland, resection of this section is used. If the tumor occupies the anterior section and lies in the gland above the branches of the facial nerve, subtotal resection of the gland is performed in the plane of the branches of the facial nerve. Parotidectomy with preservation of the branches of the facial nerve is performed when most of the gland is affected and the tumor recurs, as well as when there is a tumor of the pharyngeal part of the gland. Access to the gland is carried out by two well-known methods - Kovtunovich and Redon. In the first case, the operation begins with exposure of the peripheral part of the facial nerve (middle branch), in the second - the central trunk.
The operation is parotidectomy with preservation of the branches of the facial nerve. A skin incision is made in front of the auricle 2-3 mm, starting from the scalp of the temple, bordering the earlobe and continuing in the retromaxillary and submandibular areas. the skin-fat flap is prepared and retracted anteriorly. The parotid-masseteric fascia and the anterior edge of the gland are exposed. When approaching the peripheral branches of the facial nerve, the location of the middle branch is determined: it is located next to the duct of the parotid gland along the line connecting the tragus with the angle of the mouth. The middle branch is dissected to the point of division of the trunk, then the upper and lower branches are isolated from the gland, holding them with threads to reduce trauma. The surface layer of the gland is removed, bandaged and the salivary duct is crossed. By lifting the branches of the nerve, the deep and pharyngeal parts of the gland are dissected and removed along with the tumor, and the external carotid artery is ligated along the way.
In an operation using the Redon method, after removing the skin-fat flap, the posterior edge of the gland is released and the external carotid artery is ligated. Then the trunk of the facial nerve is found deep in the wound between the mastoid process and the posterior edge of the mandibular ramus. The location of the nerve branch is determined and all three main branches are prepared. The further course of the operation is identical to that described.
An operation that involves removing only the superficial layer of the gland along with the tumor located above the branches of the facial nerve is called subtotal resection of the glands in the plane of the nerve branches.
In case of resection of the lower pole of the parotid salivary gland, a skin incision is made bordering the angle and body of the jaw, moving downwards by 1.5-2 cm, so as not to damage the marginal branch of the facial nerve. This must also be remembered during excision of the gland due to its location in this area. Subcutaneous tissue is dissected, m. platysma and fascia. The lower part of the gland, where the tumor is located, is exposed and removed. The wound is sutured in layers.
A mucous retention cyst most often forms in the minor mucosalivary gland of the lower lip, less commonly in the cheek, the anterior floor of the mouth, the lower surface of the apex of the tongue and palate. The predominant localization on the lower lip is associated with biting it.
The cyst is located under the mucous membrane, has the appearance of a hemispherical elevation with clear boundaries, ranging in size from 0.5 to 2 cm, with a bluish tint. Sometimes the mucous membrane over it is whitish in color, which is due to the presence of scar changes due to injury. Palpation of the cyst is of elastic consistency with ripple, painless. Biting the mucous membrane over the cyst can lead to its emptying, releasing a clear, viscous fluid. When the contents become infected, inflammation occurs.
Pathohistologically, the cyst wall is a connective tissue with granulations, turning into fibrous tissue, sometimes the inner side of the wall is partially lined with stratified squamous epithelium.
A mucous retention cyst must be differentiated from tumors of the minor salivary glands, which are less common, have an elastic consistency, sometimes with a bumpy surface, without fluctuation. In some cases, it is necessary to differentiate it from cavernous hemangioma, which is characterized by a purplish-bluish coloration and a symptom of filling.
Treatment consists of removing the cyst. Two converging semi-oval incisions are made in the mucous membrane above the cyst. Using a hemostatic mosquito clamp, the membrane is separated semi-bluntly from the surrounding tissues, the connective tissue bridges are cut with scissors and the cyst is isolated. Injured small glands protruding from under the edges of the wound and interfering with suturing are removed with tweezers or a “mosquito”, each separately and entirely. Using a scalpel for these purposes can lead to their dissection, incomplete removal and recurrence of the cyst. The operation is completed by applying catgut sutures to the mucous membrane.
Cyst of the sublingual salivary gland (ranula). This cyst is located, as a rule, in the anterolateral part of the floor of the mouth near the frenulum of the tongue. Clinically defined as an oval bulge, covered with unchanged mucous membrane or translucent with a bluish tint. The cyst is always intimately associated with one of the areas or the entire sublingual salivary gland. Its former name ranula (“frog tumor”) is determined by the type of cyst and its resemblance to the laryngeal bladder of a frog. It grows slowly, over months, and does not cause pain. When it reaches a significant size, speech is impaired and eating becomes difficult. Sometimes the cyst can extend beyond the midline of the floor of the mouth, displacing the tongue posteriorly or into the submandibular region. In the latter case, it is difficult to differentiate from a cyst of the submandibular salivary gland. On palpation, the cyst often appears as a formation with fluctuation, sometimes it is more elastic. When the membrane breaks through, a viscous transparent fluid is released abundantly from the cyst, and it is not contoured. After time, the cyst fills with fluid again and becomes visible.
Microscopically, the cystic fluid contains protein substances (clumps) and sometimes so-called cystic cells, apparently of epithelial origin.
Macroscopically, the cyst shell is thin, bluish-white. In terms of its microstructure, it is fibrous and granulation tissue associated with the interlobar connective tissue layers of the gland. The inner lining of the membrane rarely has cubic or columnar epithelium.
Diagnosis of a sublingual salivary gland cyst is usually not difficult. It should be differentiated from a cyst of the submandibular salivary gland, a dermoid cyst and vascular tumors (lymphangiomas and hemangiomas) localized at the bottom of the oral cavity.
Treatment: given the close connection of the cyst with the parenchyma of the gland, they are completely removed. The previously recommended cystotomy has limited use due to the frequent development of relapses. A cyst of the sublingual salivary gland, which spreads in the lower part of the floor of the oral cavity in the form of an hourglass, is operated on in two approaches: through an incision in the submandibular triangle, the lower part is bandaged and removed; from the side of the oral cavity, the sublingual gland with the remaining part of the cyst is excised.
A cyst of the submandibular salivary gland is much less common than a ranula. It is located in the submandibular triangle and is a painless formation of soft consistency. It grows slowly and is detected by chance when a swelling is detected in the submandibular region. A large cyst pierces the mylohyoid muscle (m. mylohyoideus) or bends around it from behind and spreads to the upper part of the floor of the mouth. In these cases, its bulging into the sublingual area is also determined. The salivary function of the gland is not affected.
Diagnosis of a cyst of the submandibular salivary gland is sometimes difficult. To clarify the diagnosis, a puncture is used: obtaining a yellowish mucous fluid suggests the presence of a cyst.
A cyst of the submandibular salivary gland is differentiated from lymphangioma, lipoma, lateral neck cyst, dermoid cyst.
To determine the topography of the cyst, a double contrast method is used: cystography and sialography. Different X-ray projections allow you to determine the relationship between the cyst and the gland
Treatment. The cyst of the submandibular salivary gland is removed along with the gland.
Parotid salivary gland cyst. This is a rare disease, localized in the superficial and deep layers of the gland, mainly in the lower pole. The cyst grows slowly. It is often discovered by accident.
The cyst is a limited, painless swelling in the parotid region of soft elastic consistency. The skin over the cyst is of normal color and gathers loosely into a fold. Unchanged saliva is released from the gland duct. The contents of the cyst are yellowish liquid, sometimes cloudy, mixed with mucus. Histologically, the walls of parotid salivary gland cysts do not differ from the walls of cysts of other salivary glands.
A parotid salivary gland cyst is differentiated from organ-specific tumors, lipomas, vascular tumors of the gland, as well as from a branchial cyst caused by pathology of the first branchial cleft.
Treatment consists of removing the cyst. Due to the close connection of the cyst shell with the parenchyma of the parotid gland, the adjacent section of the latter is excised. The complexity of the operation is related to the location of the branches of the facial nerve. Surgical access to the gland is the same as when removing benign tumors of the parotid salivary gland.
"Surgical Dentistry" edited by Robustova T.G.
Fourth edition. Moscow "Medicine" 2010
Clinical cases:
Pleomorphic adenoma of the left parotid salivary gland.
Advantages of parotid salivary gland treatment at ART-Clinic
Online consultations for patients from the regions
A team of highly qualified specialists with extensive experience
Modern minimally invasive techniques of operations and reconstructions
Affordable prices, promotions, discounts, installments
Operations for the treatment of the parotid salivary gland at the ART Clinic are performed by a team of highly qualified plastic surgeons, headed by Doctor of Medical Sciences, Professor A.I. Nerobeev, who is one of the most famous maxillofacial surgeons in Russia. He specializes in reconstructive surgery.
At ART-Clinic they perform operations even in very complex cases. Success in this case is determined by both the expert class of surgeons and advanced equipment: during the operation in our clinic, a modern neurodetector is used, which sends weak current pulses and, by the reaction of the facial muscles, allows one to judge where the nerve passes, giving the doctor a hint.
Make an appointment with Professor Nerobeev by phone and 8 800 500 42 32 (calls within Russia are free) or using a special form.
Arteries and veins
Veins of the submandibular triangle
Arteries of the submandibular triangle
The main vessel in this area is the facial artery. It is the main supply line of the face. In the submandibular triangle, the vessel bends and passes along the upper and posterior surfaces of the gland, located next to the pharyngeal wall.
The facial vein is located in the thickness of the superficial layer of the second fascia. In the region of the posterior border of the triangle, it connects with the retromandibular vein and forms the common facial vein.
Pirogov triangle
This is a small portion of the triangle where the lingual artery can be found. The boundaries of the Pirogov triangle will be:
- hypoglossal nerve;
- digastric tendon;
- mylohyoid muscle.
The hyoglossus muscle acts as the bottom of the triangle. The Pirogov triangle can only be detected when the head is strongly thrown back and tilted in the opposite direction.
Important! The instructions that the doctor must follow when working with this area are extremely important, since the cost of an error is very high. Bleeding from the lingual artery can be fatal.
Causes of parotid gland tumor
The causes of tumor growths of the salivary glands are not fully understood; it is believed that they can be caused by:
- past infections (influenza, scarlet fever, measles and others);
- various chronic diseases, especially diseases of the gastrointestinal tract (the salivary glands are part of a single digestive process);
- eating disorders;
- insufficient oral care;
- genetic factors and unfavorable environmental influences.
Hypertrophy of the masticatory muscles
Along with a tumor of the salivary glands, there is hypertrophy of the masticatory muscles, which also leads to disproportions of facial features, but is sometimes caused by dental and neurological problems. To understand the true causes of the deficiency, it is necessary to conduct a detailed examination and determine whether the glands are directly enlarged or just the muscles.
When it comes to muscle hypertrophy, botulinum toxin injections come to the rescue, blocking excessive muscle activity and over time they decrease in size.
Features of surgery on the parotid salivary gland
“It must be borne in mind that tumors of the salivary glands are often multicentric (that is, there may be several of them, and unevenly located), and if not all are removed at once, relapses are possible. Therefore, parotidectomy (removal) of all or most of the gland is performed, which subsequently does not in any way affect the normal secretion of saliva,” explains A.I. Nerobeev.
During the operation, which lasts about four hours due to its complexity, the doctor makes an incision in front of the ear, isolates the nerve and removes the tumor along its branches along with the gland tissue.
If the tumor occurs in adulthood, a facelift can be performed simultaneously with surgical removal of the parotid gland, especially since the incisions are made in approximately the same places. Such operations are successfully carried out at the ART Clinic. The result of the combined approach is not only the patient’s health, but also his rejuvenated appearance.
After removal of the salivary gland, it is necessary to warn cosmetologists about this, since fillers cannot be injected into the parotid area.
Symptoms
A stone located in the duct of the salivary gland clogs the duct and prevents the flow of saliva into the mouth. In this case, saliva collects in the salivary gland, which becomes swollen and often painful. Depending on the location of the stone, pain and swelling occurs either under the jaw (submandibular gland) or in front of the auricle and in the area of the angle of the jaw bone (parotid gland). Some stones can be removed endoscopically through the mouth under local anesthesia as an outpatient procedure, but sometimes the entire salivary gland must be removed. Most often, stones are found in the submandibular gland.
The tumor is usually palpable as a nodule in the salivary gland and can cause swelling, pain, and facial nerve dysfunction. Even a benign tumor usually must be removed.