Doctors Cost
Price list Doctors clinic
Children under one year of age are also susceptible to various diseases. A runny nose and cough are some of the most common. A cough in a child under one year old can be a symptom of ARVI, but the virus is far from the only reason for the appearance of this protective mechanism. A runny nose is also a response to the invasion of pathogens and other factors. And if every child has a cough reflex, then the baby cannot blow his nose to free the nasal cavity from mucus. It is important to promptly receive medical help and recommendations for treating a runny nose and cough in a newborn.
Causes of viral and bacterial runny nose
Rhinitis is most often caused by viral and bacterial infections that cause respiratory diseases.
The vast majority of rhinitis, about 90% of the total, are viral in nature. The causative agents of colds are different types of influenza and parainfluenza viruses, adeno- and rhinoviruses.
Viruses are quite active during the cold season - autumn and winter. However, you can “catch” the infection in a situation where there is a carrier nearby, since it is transmitted by airborne droplets. The development of a viral runny nose is facilitated by reduced immunity.
The cause of a bacterial runny nose is the activation of opportunistic microflora, which, when multiplied, causes inflammation of the nasal mucosa. The causative agents of the pathology can be staphylococci and streptococci, pneumococci and other microbes.
In this case, the impetus for the development of bacterial rhinitis is also in most cases a viral infection. The virus penetrates cells and causes a pathological process, against the background of which immunity decreases and the body becomes more vulnerable to pathogenic microbes. In some cases, a bacterial infection is primary, and rhinitis occurs without the participation of viruses.
The development of bacterial rhinitis is promoted by:
- chronic respiratory diseases;
- congenital or acquired anomalies of the structure of the nose;
- severe systemic diseases;
- smoking, working in unfavorable working conditions (dust, chemical fumes).
The nature of the appearance of a runny nose during teething
Parents and pediatricians always play it safe as soon as they discover any abnormalities in the baby’s condition. Therefore, even a slight runny nose is often treated like ARVI. This is correct, because babies do not yet know how to blow their nose normally, and sputum flows down the trachea into the bronchi. This can subsequently lead to complications such as bronchitis or even pneumonia.
However, it is not always necessary to rely on vasoconstrictor drugs. A runny nose during teething occurs:
- non-infectious nature. The problem of snot during the period of teeth growth in a baby is explained by physiological reasons. The anatomical structure of the nasopharynx is as follows: the blood supply to the gums and mucous membranes of the nasal passages is carried out through a network of vessels that are closely interconnected due to their close location. During teething, the blood supply to the gums increases, so the mucous membranes begin to work more actively - saliva is produced abundantly in the oral cavity, and nasal mucus ;
- against the background of a respiratory infection. When a baby is teething, his local immunity suffers a slight disruption. Resistance to colds decreases, so the child easily picks up any virus.
If a runny nose is caused by physiology, snot on the teeth may not go away for weeks, which is not typical for ARVI.
As for nasal congestion due to a respiratory infection, excessive mucus production is not the only symptom. Other catarrhal phenomena and changes in the baby’s well-being will not be long in coming.
How are the symptoms different?
Symptoms will help determine whether it is a viral or bacterial runny nose. Signs of the bacterial nature of the disease are:
- thick discharge from the nose of a yellow or yellow-green color, often with an unpleasant odor and impurities of pus;
- impaired nasal breathing due to the accumulation of thick secretions;
- increase in body temperature to 38-40 C;
- headache, muscle pain, chills.
With the right treatment, bacterial rhinitis goes away in 7-10 days.
Viral rhinitis also has its own characteristic symptoms:
- nasal discharge is abundant, colorless and odorless;
- the temperature is normal or slightly elevated;
- sneezing, sore throat, redness of the mucous membranes of the eyes and watery eyes.
As a rule, the disease resolves within 5 days.
The differences between viral and bacterial rhinitis in children and adults are the same. At the same time, a child suffers a runny nose, regardless of its nature, more severely than adults. This is especially true for infants who are breastfed. Due to impaired nasal breathing, it is more difficult for them to latch onto the breast, which can cause digestive disorders.
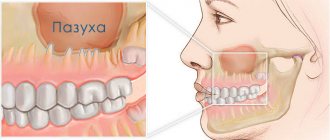
Sinusitis or “viral”: how not to make a mistake with the treatment of a runny nose
A runny nose, even in the absence of other signs of acute respiratory infections, is a problem that you want to get rid of as quickly as possible. In this case, the recovery time depends on the “nature” of inflammation and rational treatment tactics. And, in the case of sinusitis, the wrong strategy even threatens the development of complications. So how not to confuse the onset of ARVI and bacterial inflammation? And what tests can help with this?
Symptomatic analysis
Viral infections, unlike bacterial pathologies, in the vast majority develop rapidly. “Increasing” the severity of symptoms over just 1-2 days.
That is, “yesterday” only frequent “sneezing” was noted, for no apparent reason. And “today” is literally pouring out of the nose.
In addition, a “viral” runny nose is most often quickly accompanied by other signs of inflammation, in the form of “brokenness,” a sore throat, and then a cough. However, in mild cases, such “hints” may not exist.
Symptoms of bacterial acute respiratory infections, and especially inflammation of the sinuses (such as sinusitis and other sinusitis), increase much more slowly. Which, by the way, is reflected in the average duration of the disease (on average 10 days or more). And the nature of the discharge from the very beginning is “thick”, “sticky” and has a white-yellow (purulent) or greenish tint.
“Sinusitis” runny nose is usually accompanied by an intense headache or pain in the upper jaw, which increases as discharge accumulates in the nasal passages and somewhat weakens after “blowing the nose.” As well as a temperature above 38.0 C and severe symptoms of intoxication.
Who needs to be “on alert”
In the vast majority of cases, a runny nose during the “season” of acute respiratory infections is caused by the influence of viruses and is rarely complicated by any sinusitis.
However, a small percentage of cases still occur due to bacterial infections. Moreover, mainly as a complication of a viral infection.
The fact is that opportunistic flora in the nasopharynx and oropharynx is present in “safe” concentrations in every healthy person. The presence of foci of chronic infection, such as caries, tonsillitis and others, is also important.
With a decrease in general or local immunity, such flora “will not miss the chance” to be active. But the severity of the “consequences” of this “event” already depends on the quality and quantity of the latter.
The most aggressive pathogens of sinusitis include Staphylococcus aureus, some types of streptococci and Pseudomonas aeruginosa. And only culture of a smear from the nose and throat can help verify their participation in the process.
How to figure out what kind of runny nose you have
The first distinguishing feature is the color of the snot. If a green or green-yellow tint appears, it means that the nature of the runny nose is most likely bacterial. However, to determine whether a runny nose is viral or bacterial, you need to pay attention not only to the color of nasal discharge, but also to other symptoms.
If a person’s health worsens, the temperature rises to high levels, the disease continues to progress and does not go away after 10 days or more, it is necessary to consult a doctor. The specialist will prescribe a general blood test, rhinoscopy, and laboratory testing of a smear from the nasal canals.
Is it necessary to treat “tooth” snot?
One of the most common mistakes that many parents make if their child develops snot is to independently use various medications to combat this problem. The first place in this list is traditionally occupied by various anticongestive drugs that cause constriction of blood vessels and are intended to relieve swelling in the nasal cavity. Such drugs include drops “Nazivin”, “Naphthyzin”, “Xylometazoline” and other drugs with a similar mechanism of action.
The main component of the drug is oxymetazoline hydrochloride
Anticongestants have a large number of side effects, the main of which are the rapid addictive effect and gradual atrophy of the nasal mucosa, which can ultimately lead to the development of chronic atrophic rhinitis. The use of these medications is justified only in severe cases, when the child cannot breathe normally due to severe swelling of the mucous membrane, which happens mainly with infectious rhinitis. Antihistamines that block the production of the main mediator of inflammatory reactions (histamine) are also unacceptable for the treatment of physiological rhinorrhea associated with teething.
Important! Despite the fact that the use of traditional remedies for snot associated with teething is not recommended, it is impossible to completely refuse treatment, since stagnation of mucus in the nose creates an excellent breeding ground for various bacteria and can cause serious complications: otitis media, bronchitis, etc. .d.
The tooth came out, but the runny nose does not go away
If the tooth has already erupted, but the runny nose still does not go away, and the child feels satisfactory, his body temperature is normal, and the snot retains a watery consistency, perhaps the reason is improper hygienic care and non-compliance with sanitary standards. For the normal functioning of the nasal mucosa, constant hydration is necessary: moistened epithelium effectively binds particles of dust and dirt and removes them from the nasal cavity, preventing them from penetrating further into the airways.
To create physiologically correct conditions for normal functioning of the mucous membranes, it is necessary:
- maintain the required temperature in the children's room (about 20°-22°C for games and 16°-18°C for sleeping);
- ventilate the room at least 6-8 times a day, each ventilation should last about 10-15 minutes;
Don't forget to ventilate the nursery
- regularly carry out wet cleaning, remove dust from furniture, clean toys and carpets (ideally, it is better to remove carpets, thick curtains, books and soft toys from the baby’s room);
- Do not use disinfectants during cleaning (plain water is fine).
Do wet cleaning at least three times a week
Strengthening the immune system is also of great importance, which consists of compliance with the vaccination calendar and the introduction of complementary foods, frequent walks, adequate temperature and movement conditions, and hardening procedures.
Video – Komarovsky about runny nose and teething
Rhinorrhea (snot) during teething is a very common occurrence that should not be confused with an infectious runny nose. Under no circumstances should you give your child antiviral drugs, immunomodulators, antihistamines and anticongestive drugs without consulting your doctor. In most cases, such a runny nose goes away on its own after teething, and to relieve it, it is enough to adhere to a certain hygiene regimen. Read the article for strong painkillers for toothache.
- How long does it take for drugs to leave the body?