Pericoronitis, or a total inflammatory process of the gums caused by infection in the oral cavity. Most often it occurs at the time of tooth eruption, especially with the growth of wisdom teeth. The process is accompanied by severe swelling of the gums, severe pain, especially when opening the mouth, as well as an unpleasant odor and unusual taste from the mouth. In addition, pericoronitis is accompanied by a state of general weakness, less often by a rise in temperature to a low-grade level. Some people also note discomfort in the digestive tract (diarrhea, among others).
Causes of Pericoronitis
Incorrect growth of wisdom teeth
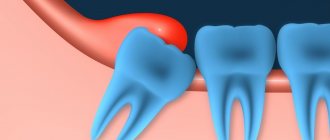
The specificity of the formation of such a phenomenon as Pericoronitis lies in the field of human development, starting from the embryonic period. As a rule, the phenomenon is caused by inhibited development of the jaw arch while maintaining the size of the dental crown. In this case, difficult teething occurs, especially wisdom teeth.
Painful sensations are caused by inflammation of the thickened gum tissues, on which the growing tooth presses from below.
As a result, hyperemia, swelling of external tissues and traumatism of bone tissue occurs and, as a result, periosteal abscess if the patient does not consult a dentist in time. In addition, a tooth that is experiencing discomfort as it grows can injure the tooth next to it, damage its enamel, which ultimately leads to the loss of a healthy tooth. As a rule, teeth that provoke the development of Pericoronitis must be removed.
Varieties
The process may differ in its severity, degree of complexity, and location. Taking these points into account, several types of pericoronitis are distinguished - acute, retromolar, isolated purulent, ulcerative, catarrhal.
Catarrhal
This case can be observed in most cases as it is the initial stage of the disease. If you consult a doctor in a timely manner, a person can avoid advanced, complex forms of pericoronitis. The symptoms are a little easier here. If a person seeks professional help in time, he will be able to stop the inflammation quickly.
Ulcerative
The reason for the appearance of this type of disease is the gum, which was inflamed and infected with fusosprirochaetes. The main symptom is a necrotic ulcerative rim along the edges of the gums. If a person removes the plaque on the teeth that covers the gums, the bleeding will become stronger. At this stage, surgical intervention is not allowed. Ulcerative pericoronitis should be treated using conservative methods.
Purulent isolated subacute
This type of disease suggests that it is a chronic form. At this stage, in the place where the tooth erupts, there is severe pain of a constant nature. And as a person chews and swallows food, it becomes stronger. Usually the temperature rises, regional lymph nodes become enlarged, and there is an inability to open the mouth. If you press down on the gum hood, pus will flow out of it. With the help of an X-ray examination, you can see that the bone tissue near the wisdom tooth is resorbing.
Retromolar periostitis
An abscess is already forming here. The symptoms resemble the previous version, but they are more pronounced at this stage. The patient's condition becomes much worse. The dentist must examine the mouth visually by forcefully opening the mouth. This type of disease involves inflammation and changes in soft tissues; it is observed in those places where the tooth erupts. If there is an infiltrate there, then the doctor makes such a diagnosis.
Acute periostitis
This type of pericoronitis has all the symptoms listed above. If it is not treated on time, the disease can become chronic. If pericoronitis persists for a long time, purulent periostatitis may occur. This condition usually appears when the lower third molars erupt.
Pathogenesis of Pericoronitis
The pathogenesis of the inflammatory process in the oral cavity is associated with the formation and growth of an erupting tooth. Partial lifting of the gum forms a tissue formation - a periosteal flap, or, as it is also called, a “hood”, covering the part of the tooth that comes out of the gum. A pocket is formed under it, where plaque and food particles accumulate, as well as microorganisms that cause decomposition and decay processes, leading to a type of inflammation such as pericoronitis.
Any absorption of food by the patient is a supporting process of growth and development of pathogenic microflora in the patient’s oral cavity, during which the inflammatory process progresses. Mechanical damage to the gum mucosa also occurs here. The result is tissue changes that form scars on the body of the hood, as a result of which the periodontal gap quickly increases in size, bringing new suffering to the patient.
Classification
Pericoronitis is divided into acute, which occurs most often, and a rarer form - chronic pericoronitis. According to the flow, the following types of pericoronitis are distinguished:
Catarrhal – characterized by slight swelling and pain when touched; Purulent - constant pain and the presence of purulent discharge; Ulcerative – leads to the formation of ulcerative defects on the gums;
Retromolar is distinguished as a separate form - it is distinguished by its location, which does not allow it to be easily seen and treated, which makes it difficult to combat this disease and increases the likelihood of complications.
Development of acute pericoronitis
Acute Pericoronitis is considered as a type of acute periodontitis with primary symptoms of damage to the gum tissue. Damaged tissues located above the crown of a growing tooth involve in the inflammatory process all areas of the gums located near the resulting lesion. This course of the process is most often observed during the growth and eruption of the third, less often, fourth large molars of the lower jaw.
As a reason, experts consider both the lack of space for the formation of new teeth due to the development of a short jaw, and the abnormal development of the dental crown itself, which has assumed an incorrect location in the dentition.
Clinical picture
During a dental examination, hyperemia and swelling of the tissues formed around the growing tooth are observed. The area of the wings of the jaw fold is also affected. The lower fornix of the vestibule of the oral cavity is particularly susceptible to damage, with the transition of hyperemia to the palatine arch. The infiltrated tissue flap is raised.
Often in this area one can observe traces of tissue erosion with exudate of a serous-purulent composition released from under them when pressed.
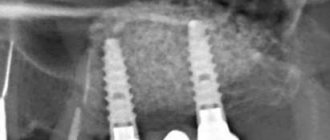
As a rule, an X-ray examination confirms the diagnosis, and the photographs clearly show the rear, highly sparse bone part of the growing tooth, shaped like a semicircle. Often the temperature may rise in the area of the affected tissue. When the general body temperature rises to subfebrile levels, regional lymph nodes enlarge.
Bad breath and changes in taste when eating are virtually inevitable symptoms accompanying the inflammatory process. If the process is neglected, a periosteal abscess may occur, accompanied by a constant outflow of pus and the patient’s inability to open his mouth. A severely neglected process causes the formation of osteomyelitis or phlegmon.
Symptoms
Pericoronitis is accompanied by a number of symptoms.
- Objective symptoms that can be seen by the patient himself or the dentist during an examination of the oral cavity.
The presence of a mucosal hood on the surface of the erupting tooth and a pathological gingival pocket are determined [6,9,10]. Externally, at the site of the erupting tooth, the gum tissue is hyperemic (red), voluminous due to swelling. The causative tooth may be mobile.
During the examination, the dentist evaluates the regional lymph nodes (cervical, submandibular, preauricular), their size and the presence of pain. An increase in the latter indicates a prolonged course of pericoronitis. With mild severity, the body temperature rises to 37°C, and in the presence of purulent complications - to 38-39°C [2,5,13]. The face with pericoronitis is asymmetrical, due to swelling and enlargement of soft tissues on the affected side.
- Subjective symptoms caused by the patient’s sensations.
Pain in the gums occurs at rest and intensifies when brushing teeth, chewing food, talking and opening the mouth. Pain sensations can spread along the branches of the trigeminal nerve to the ear and eye[7]. There is an unpleasant, putrid odor from the mouth. General health worsens, weakness occurs, sleep is disturbed, appetite and performance decrease. In response to pain, the masticatory muscle spasms, making it difficult to open the mouth, chew and swallow food[11].
Diagnostics
Diagnosis is carried out exclusively by dental specialists based on the examination data provided, including, if necessary, the results of fluoroscopic examinations. Based on the examination data, a clinical picture is drawn up. It serves as the basis for prescriptions for treatment aimed at preventing the possibility of complications. The method of treatment depends primarily on the general condition of the patient, as well as on the nuances and characteristics of the course of the inflammatory process.
Treatment
You can't do it without the help of a doctor!
In the case of pronounced hyperemic edema and severe contraction of the jaws, the patient is prescribed a trigeminsympathetic blockade. If pericoronitis occurs without any particular complications, rinsing of the pocket under a tissue flap - a hood - is prescribed. This can be either a weak solution of potassium permanganate or a solution of furatsilin.
Local treatment is also prescribed, consisting of constant warm rinsing with a disinfectant solution and placing a tampon soaked in iodoform. Sulfonamide drugs and painkillers are prescribed for oral administration. Surgery may be performed if local therapy does not produce a positive result.
Curative surgery can act in 2 directions:
- Excision of the hood under local anesthesia to facilitate the eruption of a growing tooth and remove the infection that has accumulated under it.
- Extraction (removal) of a tooth in a position where tooth growth is impossible, or when it destroys another tooth nearby. As a rule, such manipulation is often performed with wisdom teeth, which have virtually no functional load in the oral cavity.
Pericoronitis, which causes relapses, can be cured only after removal of the corresponding tooth. Recently, laser therapy has become widely used to treat inflammatory processes associated with teething. Using a low-intensity infrared laser under local anesthesia, the resulting hood is excised, while simultaneously stimulating the flow of fresh blood to the surgical site.
Recommendations for patients
If an incision or excision of the hood was performed in the treatment of pericoronitis, it will be necessary to follow several preparatory and postoperative measures that will speed up healing and reduce the risk of complications.
- For two to three hours after the intervention, do not take food, hot drinks, or alcoholic drinks.
- On the day of the operation, do not go to the bathhouse, sauna, take a hot bath, or be in the sun or in a hot room.
- Limit physical activity the day before and on the day of treatment.
- During these days and the next three days, it is recommended to follow a diet, exclude alcohol, spicy, very hot foods.
- Before the intervention, you should not eat foods with a strong smell.
- Smokers should quit cigarettes the day before the hood excision, on the day of surgery, and two days after.
- For sanitation (cleaning and disinfection), you can use a mouth rinse with antiseptic solutions.
- After the intervention, the doctor will prescribe medications that accelerate healing.
- Do not apply warm compresses or ointments containing bee, snake, etc. venom.
- If after excision of the hood or placement of therapeutic turundas there is pain, severe swelling, increased discomfort, pain in the area of the submandibular lymph nodes, you need to consult a doctor to identify the cause and take action.