Seal
One of the most popular procedures in modern dentistry is the installation of crowns. The method allows you to save a damaged tooth, restore its function, and restore the attractiveness of your smile. But sometimes after orthopedic treatment, discomfort, sharp or dull pain, and sensitivity to temperature occur under the crown. In this case, discomfort may appear both in the coming days after prosthetics and several years later. What should be done in this case?
First of all, you need to understand what is causing the pain. If very little time has passed after treatment and the discomfort is not too great, do not worry. Such pain is residual in nature. As a rule, specialist intervention is not required - 3-5 days after treatment, the discomfort goes away on its own. It’s worse when the tooth starts to hurt months or even years after prosthetics. In this case, you cannot do without a visit to the clinic.
Khashchenko Stanislav Sergeevich is a dental surgeon with extensive experience.
The importance of prosthetics
The main reason for refusals to install dentures is associated with the erroneous opinion of old-school dentists about the mandatory depulpation (removal of the nerve) of teeth before prosthetics. Before dispelling this myth, it is necessary to recall the importance of timely prosthetics.
Without an adequate prosthesis, neighboring healthy teeth begin to carry an unusual load, which leads to their increased wear, mobility and early loss. In addition, in the absence of even one tooth, speech defects appear, chewing functions are disrupted, bite pathologies occur, and even facial proportions are distorted.
How is the tooth nerve removal procedure performed?
For most people, the fear of removing the nerve of a tooth comes from the times when dentistry was not yet as developed as it is today. Many people remember that previously this operation was performed with the help of arsenic, which made it possible to “kill” the nerve. But depulpation in this way had two significant drawbacks:
- Danger of tooth decay due to prolonged exposure to arsenic;
- Extremely painful sensations during the procedure.
Fortunately, all this is a thing of the past and today dentists have managed to achieve the optimal combination of treatment effectiveness and patient comfort when removing the nerve.
How is tooth nerve removal done in modern dentistry? The key difference is that safe arsenic-free agents are used to remove the pulp, as well as high-quality local anesthesia. Depulpation can be done in one visit to the dentist, with minimal discomfort during the procedure and a quick recovery period.
Causes of frequent depulpations
Why do orthopedists so often remove pulp from teeth? The main reason lies in the desire of doctors to play it safe and avoid complications after prosthetics. The fact is that teeth have a porous structure. Pores are dentinal canals that run from the enamel to the pulp of the tooth. During grinding of teeth for a crown, mechanical irritation of the pulp may occur through these dentinal canals.
And at the last stage of fixing the prosthesis, there is a toxic effect of cement. And as a result - infection and death of the pulp. However, this does not allow us to consider depulpation as a prevention of complications, since this procedure is inevitably associated with the risk of developing periodontal pathologies. After all, no one suggests removing the appendicitis for preventive purposes. Living teeth retain their stability much longer.
Whereas teeth subjected to depulpation become extremely fragile and are more susceptible to destruction, losing their shock-absorbing function.
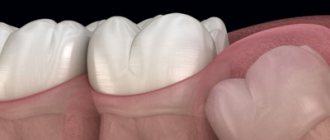
Technique for installing a crown on a living tooth
The procedure is performed in several stages (Fig. 1). First of all, an initial examination and diagnosis will be carried out. At this appointment, a treatment plan will be developed. The dentist will advise you to perform hygienic cleaning of the mouth in order to most accurately select the color of the crown. Treatment of caries and pulpitis is mandatory. The doctor will not deal with prosthetics for a diseased tooth.
At the next appointment, the specialist will prepare the tooth to give it the desired shape. He will remove enamel equal to the thickness of the crown. The procedure is quite painful, so it is performed under anesthesia.
Rice. 1. The process of installing a crown on a living tooth
To make a crown, the doctor will take an impression, from which a plaster model is first made, and then a full-fledged prosthesis is poured. During the manufacturing period, a temporary crown is placed on the tooth. Trying it on will show how accurately it is made. Next, the crown is fixed with dental cement and treated with antiseptic agents.
Knowledge and experience of orthopedists
Of great importance in the issue of prosthetics without depulpation is the knowledge of orthopedic doctors about the safety zones of the crown parts of teeth. Safety zones are those areas of the tooth within which you can safely grind the tooth tissue without damaging the pulp.
The canines have slightly more such tissue than the lateral incisors. The age of the patient is also important: the older the person, the less likely the pulp is to be damaged.
Contact our clinic for a consultation on prosthetics without depulpation, and we will definitely find the right solution for you!
Dental prosthetics in our clinic. Types of dental crowns and methods of their manufacture
Methods for removing the nerve of a tooth
Today, the depulpation procedure is not limited to one method and can be performed in two ways, depending on individual indications.
Vital method of tooth nerve removal
With this method, the “living” nerve is removed, and thanks to local anesthesia, the patient does not feel pain during this treatment. The advantage of this method is that the nerve is removed in one visit to the dentist. After administering anesthesia, the doctor “removes” the area of the tooth affected by caries, then the nerve is removed, after which a permanent filling is installed on the tooth. Vital depulpation is possible for both adults and children.
Devital method of tooth nerve removal
This method involves the complete removal of the “dead” nerve from the crown and root part of the tooth. It takes longer than the vital. First, under anesthesia, the doctor “removes” the area of the tooth affected by caries, then a special paste is applied to the pulp to kill the nerve. After this, a temporary filling is placed. On the second visit, the nerve is completely removed, and a permanent filling is installed in place of the temporary filling.
Today, the vital method of nerve removal is more common in dentistry due to its speed and efficiency. However, in some cases, if there are indications, the devital method of depulpation is more applicable for the patient. The removal method is determined by the doctor based on the results of an x-ray examination.
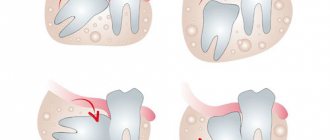
Indications for depulpation
Despite all the disadvantages of tooth depulpation, in some cases it is impossible to do without this procedure. Indications for nerve removal may include:
- advanced caries affecting the deep tissues of the tooth;
- the appearance of caries on one or more roots;
- incorrect anatomical position of the tooth;
- low landing of crowns;
- inability to prepare a tooth without opening the pulp chamber;
- inflammation of the pulp or periodontium;
- uncharacteristic anatomical features of the organ (for example, significant tilt of the tooth axis or large size of the pulp chamber).
If the dentist identifies at least one of the listed reasons in the patient, depulpation will be justified.
If caries or pulpitis is present, depulpation is necessary
How long does a tooth hurt after nerve removal?
As already mentioned, the depulpation procedure is performed using local anesthesia, so pain directly during nerve removal is excluded. However, after the anesthetic wears off, the patient may feel discomfort at the treatment site.
After removal of the nerve, it is possible to use painkillers, but before using them you must consult with your dentist. This will help reduce pain if it causes severe discomfort. It is also recommended that during the healing period, stick to soft foods in the diet that will not create additional stress when chewing food. Another way to reduce pain can be preventive rinses and oral baths.
To accurately answer the question of how long a tooth hurts after nerve removal, you need to understand that these are all individual characteristics of each patient. However, on average the healing process takes 2-3 days. Do not self-medicate or ignore pain. If the pain does not go away at the end of this period, this is a reason to consult a dentist.
Why does a tooth hurt under a crown and what to do about it?
In addition, the harmful effects on the tooth are enhanced when using low-quality instruments: dull burs, poorly centered tips, insufficient water cooling which leads to nerve burns, overheating of the tooth during polymerization of the adhesive, etc.
Another equally common cause of tooth sensitivity is medical errors and violations of the technology of tooth preparation and fixation of restorations. For example, excessively deep tooth preparation, when the doctor grinds off more dental tissue than necessary, coming too close to the dental nerve. In this case, traumatization of the nerve occurs, to which the tooth responds not with short-term, quickly passing sensitivity, but with long-term aching, severe pain - pulpitis.
If you experience pain under a crown or veneer of this nature, this means inflammation of the dental nerve. The only salvation in such a situation will be depulpation of the tooth, and it would be good if this does not require removing and redoing the restoration, but it will be possible to get through it.
Another trouble that can lead to pain in a living tooth under a crown or veneer is caries that was not completely cleaned out during tooth preparation and continued its victorious march after fixing the structure.
Another example of medical error is damage to the gums either with a bur during tooth preparation, or with a retraction thread placed in the gingival sulcus to obtain a clear preparation boundary.
Since such injuries heal quite quickly in the oral cavity, they cause inconvenience for a fairly short time, although sometimes they require treatment.
Another thing is chronic gum injury caused by improperly made crowns or veneers.
This refers to either the edge of the restoration going too deep under the gum, or the edge being too thick, overhanging the margin of the preparation.
In both cases, compression of the gums by ceramics occurs, which means impaired blood circulation in this area, chronic inflammation of the gums - gingivitis and periodontitis - with all the ensuing consequences: cyanosis, bleeding, etc.
Another problem that causes pain in a tooth under a crown or veneer is tooth mobility that appears after the structure is fixed.
As a rule, this is also a consequence of an error, which consists in overestimating the bite, which leads to overload of the tissues that hold the tooth in the bone - the periodontium and periodontal tissue. As a result, the tooth becomes mobile and becomes painful when biting and chewing food, and sometimes even when simply closing the mouth.
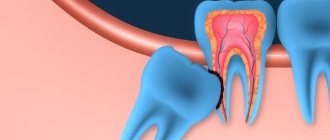
Another danger of overbite is the so-called “aseptic periodontitis”. The essence of this phenomenon is that overloading a tooth does not cause its mobility, but the death of the nerve and the transition of the pathological process to the bone, in which a focus of inflammation is formed - cystogranuloma, and then a cyst.
And since the cause is not infection, but overload, this process is called aseptic.
It must be said that this kind of mobility and development of cysts can occur both in living teeth and in pulpless ones, even very carefully treated and with perfectly sealed canals.
Well, now let's talk about pulpless teeth.
In addition to the problems common to living teeth, they have their own characteristics.
First of all, we must talk about errors associated with poor diagnostics.
Very often, it is impossible to see a cystogranuloma or dental cyst on simple dental or panoramic photographs. This leads to the fact that the doctor makes decisions about making a crown or veneer without having all the necessary information about the condition of the tooth and surrounding tissues.
This means that a restoration can be made for a tooth that is already involved in a pathological process, which simply has not yet manifested itself properly.
Under the influence of medical manipulations and the changed load on the tooth, periodontitis begins to progress, pain appears and, as a rule, such a tooth is removed.
That is why we pay such serious attention to the diagnosis of dental diseases and always use the most modern type of dental diagnostics - computed tomography - during the initial examination of the patient.
Another common cause of pain in a pulpless tooth under the crown is a crack in the root of the tooth or a chipping of any of the walls of the crown part, that is, mechanical damage to the tooth.
If a root crack most often occurs in pulpless teeth restored with root pins or stump pin inlays, then wall spalling occurs in teeth without pins, with thin walls and large fillings. When the wall breaks off, the broken part seems to “hang” on the gum, causing pain with each vibration.
With a root crack, the pain sensations are similar to those with periodontitis.