Maxillofacial phlegmon: causes and dangers
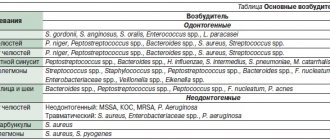
The vast majority of phlegmons (more than 90%) are odontogenic in nature, that is, they arise due to a tooth that is not treated in time, destroyed by caries or periodontitis. The causative agents of inflammation - staphylococci, streptococci, anaerobic and putrefactive microorganisms - penetrate from the affected tooth root into the tissues of the perimaxillary region due to the peculiarities of the outflow of lymph and venous blood. Another difference between phlegmon and an abscess is that it develops against the background of a significant decrease in immunity, while an abscess can form in a patient with normal protective reactions of the body.
Cellulitis of the maxillofacial area is a dangerous condition that requires serious surgical intervention. The severity of the patient’s condition is determined by the degree of neglect of the process and general intoxication of the body. In addition, nerve endings are concentrated in the jaw area, so a diffuse purulent inflammatory process brings unbearable pain and physical suffering to a person. Vital functions are impaired - swallowing, chewing, speaking, breathing. And a large number of venous plexuses favors the rapid spread of the process and its transition to vital organs and systems. The most severe complications of this disease:
- phlebitis;
- thrombophlebitis;
- mediastinitis,
- abscesses of internal organs;
- meningitis;
- meningoencephalitis;
- sepsis.
Cellulitis is especially severe in children or if it is caused by anaerobic microorganisms.
Tonsillogenic phlegmon of the neck, complicated by mediastinitis, in a patient with diabetes mellitus
Tonsillogenic phlegmon of the neck against the background of diabetes mellitus (DM) is extremely difficult, often complicated by the spread of a purulent process into the mediastinum and the development of multiple organ failure, which in 10–15% of cases leads to death. In such patients, the purulent process is prone to lightning spread. Decompensation of diabetes worsens the patient's condition. 1 ml of pus inactivates 10–15 ml of endogenous or exogenous insulin, thereby aggravating metabolic disorders [1–3].
We present an observation of tonsillogenic phlegmon of the neck, complicated against the background of diabetes by purulent mediastinitis, pleural empyema and multiple organ failure, which was the cause of death.
Patient M., born in 1948, was admitted to the ENT department of the State Budgetary Healthcare Institution MONIKI named after. M.F. Vladimirsky" with complaints of difficulty breathing, pain in the neck, worsening when turning the head, swelling in the submandibular region on the right, sore throat when swallowing, thirst, weakness, increased body temperature, headache.
From the anamnesis it is known that 5 days before admission to the hospital there were complaints of a sore throat and difficulty passing liquid and solid food after hypothermia (the patient worked outside, drank cold water). She did not seek medical help, she treated herself: she drank hot milk. After 2 days, difficulty breathing appeared during physical activity, and an infiltrate in the submandibular region also began to gradually increase. During the illness, she did not notice any increase in body temperature. She did not sleep the entire night before hospitalization due to difficulty breathing. For the last 3 days I drank only water. I contacted an ENT doctor at a local clinic, who diagnosed: peritonsillar abscess, neck phlegmon, 2nd degree laryngeal stenosis. The patient was urgently sent to the ENT department of the State Budgetary Healthcare Institution MONIKI named after. M.F. Vladimirsky". It is known that the patient has been suffering from hypertension in recent years with an increase in blood pressure to 180/110 mm Hg. Art. and type 2 diabetes, for which she took glibenclamide 5 mg, 0.5 tablets 2 times a day. Blood sugar levels were not measured.
Condition on admission: extremely severe, body temperature – 37.5oC. The patient is conscious, forced position - sitting. Hypersthenic physique, increased nutrition. The skin is pale, there are no rashes. Breathing at rest is noisy, with the participation of auxiliary muscles, respiratory rate is 26–30/min. The chest is symmetrically involved in the act of breathing; in the lungs, breathing is harsh and is carried out in all parts of the lungs. Heart sounds are rhythmic, muffled, heart rate - 110/min. Blood pressure – 157/95 mm Hg. Art. The abdomen is soft, the liver is at the edge of the costal arch, physiological functions are normal. No meningeal symptoms were detected at the time of examination.
During mesopharyngoscopy: grade II–III trismus, asymmetry of the soft palate due to edema and infiltration of the right palatine arch are determined; at the upper pole of the right palatine tonsil there is a point fistula with copious purulent discharge. There is a dense infiltrate in the right submandibular region, which extends to the anterolateral surface of the neck, the skin over it is hyperemic. The laryngeal mass is not changed. Moore's sign is positive.
Fibropharyngolaryngoscopy: the mucous membrane of the pharynx and larynx is sharply hyperemic and swollen. A bulging of the lateral wall of the oropharynx is detected, the laryngeal mass is shifted to the left due to infiltration. The mucous membrane of the epiglottis is sharply hyperemic and infiltrated.
The patient was consulted by an endocrinologist, cardiologist, maxillofacial surgeon, and ophthalmologist.
After administration of 10 units of soluble insulin subcutaneously, glycemia was 33.4 mmol/l. The insulin dose was calculated. Blood test dated 04/11/2007: hemoglobin – 175 g/l, glucose – 31.2 mmol/l, total protein – 82.7 g/l, creatinine – 240 µmol/l, leukocytes – 21,109/l, ESR – 51 mm/h
Electrocardiogram (ECG): sinus tachycardia. Rare ventricular extrasystole. Horizontal direction of the electrical axis of the heart. Low-voltage ECG in standard leads. Rotation of the heart clockwise, i.e. with the right ventricle forward. Pronounced changes in the myocardium of the left ventricle.
On a chest x-ray, the lung fields are transparent. Roots are structural. The diaphragm is positioned normally. Heart with an enlarged left ventricle. The aorta is compacted. The mediastinal shadow is not expanded. Free gas and liquid are not detected.
An X-ray of the neck according to Zemtsov shows thickening of the prevertebral soft tissues due to infiltration with a maximum at the level of C5.
Taking into account complaints, anamnesis, clinical picture, and examination, a diagnosis was made: right-sided paratonsillar abscess; phlegmon of the neck; II degree laryngeal stenosis; Type 2 diabetes of moderate severity, decompensated; suspected ketoacidosis; stage II hypertension; III degree obesity.
After 3-hour preoperative preparation (antibacterial, detoxification therapy, correction of blood sugar levels - surgical level 12.9 mmol/l), surgical intervention was performed - tracheostomy under local infiltration anesthesia, then under anesthesia through a tracheostomy, abscessonsillectomy on the right, opening and drainage of the cellular spaces of the neck on right. Surgical findings: soft tissues have the appearance of “boiled meat” with a pungent putrefactive odor, their differentiation is difficult. A passage into the posterior mediastinum was detected about 4 cm below the jugular notch. There is no pus, but gas with a putrid odor is obtained. An inspection of the submandibular area and peripharyngeal space was carried out; purulent discharge was also obtained. A smear was taken for microflora and sensitivity to antibiotics. 3 double-lumen drains were installed in the posterior mediastinum, peripharyngeal space, and submandibular region (Fig. 1).
After the operation, the patient was transferred to the intensive care unit, where massive systemic antibacterial therapy was carried out according to the principle of de-escalation - meropenem 1 g 2 times a day IV + metronidazole 100.0 3 times a day IV, infusion therapy in a volume of 2900 ml , decongestant therapy, vascular therapy, correction of blood sugar levels (insulin 40 units). Daily dressings were performed and active flow aspiration was established.
Blood sugar levels ranged from 13.4 to 18.1 mmol/L. In a biochemical blood test dated April 13, 2007: total protein - 48 g/l (normal - 64-83), urea - 61.1 mmol/l (normal - 1.7-8.3), creatinine - 700 µmol/l (normal – 44–80), creatinine kinase – 782 units/l (normal – 24–170), lactate dehydrogenase – 1050 units/l (normal – 230–460), C-reactive protein – 215 mg/l (normal – <5), uric acid – 1232 µmol/l (normal – 142–339).
X-ray of the chest organs in dynamics 1 day after the operation: negative dynamics are noted, manifested in the form of total inhomogeneous darkening of the left pulmonary field; infiltration of the pulmonary field cannot be excluded. The mediastinal shadow is expanded. Free gas is determined. There is also a moderate widening of the mediastinum.
Together with thoracic surgeons, an inspection of the cellular spaces of the neck on the right and thoracoscopy were performed, during which a turbid liquid with a foul odor was obtained. A right thoracotomy was performed. In the right pleural cavity there is about 200 ml of liquid the color of meat slop with an ichorous odor and fibrin flakes. Inspection and drainage of the right pleural cavity, anterior and posterosuperior mediastinum were performed. In the postoperative period, previously administered therapy was continued. The patient was consulted by a detoxicologist, and plasmapheresis was recommended. 1 day after the operation, a dynamic X-ray of the chest organs was taken: there was no gas in the pleural cavities, the mediastinum was moderately dilated, and there was a small amount of fluid in the pleural cavities. The median shadow is expanded at the level of the aortic arch.
Despite the measures taken - detoxification, antibacterial therapy, correction of blood sugar levels, 2 sessions of plasmapheresis - the patient's condition continued to progressively deteriorate. The patient was on artificial ventilation through a tracheostomy, unconscious, hemodynamics were supported by adrenergic agonists, and complete compensation of diabetes could not be achieved.
Against the background of progressive cardiovascular failure, cardiac arrest was recorded on the 4th day after admission to the hospital. Resuscitation measures for 40 minutes - without effect. The patient died. An autopsy confirmed the diagnosis and revealed pronounced dystrophic changes in parenchymal organs. The cause of death was multiple organ failure.
Thus, clinical observation shows that the occurrence and progressive course of neck phlegmon with the development of such severe complications as mediastinitis, sepsis are directly dependent on concomitant diseases of the body; their course worsens sharply against the background of diabetes.
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Complications of cellulitis
Purulent-necrotic phlegmon of the leg in the process of cleansing the wound surface and forming granulations.
The main ones are:
- gangrene,
- sepsis,
- thrombosis of arteries and veins of the lower extremities, mesenteric vessels,
- abscesses of the liver, kidneys, spleen, respiratory organs, lungs, brain,
- thromboembolism of small and large branches of the pulmonary artery,
- multiple organ failure.
Purulent-necrotic phlegmon of the back
With a progressive disease, pus accumulates in the deeper layers of the skin, causing the development of inflammation of the surrounding tissues, affecting the blood and lymphatic vessels and nerves.
Cellulitis of the posterior thigh
Symptoms
Phlegmon of the perimaxillary region, unlike an abscess, develops rapidly and is characterized by severe intoxication. Its main clinical manifestations:
- infiltration on the affected area of the face or neck;
- hyperemia, swelling, soreness of the skin at the site of inflammation;
- high body temperature;
- rapid pulse;
- severe pain when chewing, swallowing, talking;
- spasm of the muscles responsible for opening and closing the mouth (trismus);
- increased salivation;
- weakness;
- chills;
- pale skin;
- loss of appetite;
- sleep disorders;
- enlargement of regional lymph nodes;
- facial asymmetry.
Periandibular phlegmon, photos of which can frighten impressionable people, is always accompanied by an increased number of leukocytes and neutrophils in the blood, a shift in the leukocyte formula to the left and an increased ESR value. The diagnostic sign of phlegmon in the blood serum is C-reactive protein. Protein and white blood cells also appear in the urine.
Prevention of cellulitis and oral infections
The best way to avoid oral phlegmon is prevention.
- Regular visits to the dentist for professional teeth cleaning, plaque and tartar removal reduces the likelihood of caries and gum problems. Tartar causes bleeding gums, and microtraumas on the gums provide an entry point for bacteria and oral infections.
- General strengthening of the immune system, taking vitamins, and a varied diet with plenty of protein and fiber leave little chance for infections to enter the body through the oral cavity.
Treatment
Despite the severity of the disease, in general, with timely treatment, perimandibular phlegmon has a favorable prognosis. Treatment is carried out only in a hospital setting, but at the initial stage everything is often limited to the use of conservative methods - antibiotic therapy, the prescription of restoratives, vitamins, and a special diet. But if the process has already started and the spread of infection is observed, complex surgical treatment is indicated, which includes the following points:
- opening the inflammation site under general anesthesia;
- cleansing the wound from pus;
- installation of drains for drainage of wound contents;
- daily treatment with bactericidal solutions;
- powerful antibiotic therapy - often a complex of several drugs is prescribed;
- detoxification of the body;
- use of antipyretic and painkillers;
- prescription of immunomodulating, restorative agents, vitamins;
- physiotherapy – ultraviolet irradiation, UHF, magnetic therapy, etc.
If treatment is successful and there are no complications, the patient’s recovery occurs on average in 14-21 days.
Classification of disease stages
The development of the purulent process in the orbital tissue occurs in stages, passing through the preseptal stage, the stage of orbital cellulitis, the stage of subperiosteal abscess, the stage of abscess and phlegmon. At the same time, timely adequate therapy can interrupt the further development of purulent inflammation at any stage.
The preseptal stage of the disease is characterized by inflammatory swelling of the tissue of the orbit and eyelids, mild exophthalmos, with preservation of eye mobility, without changes in visual acuity. Further progression of the inflammatory process and its spread to the posterior parts of the orbit provokes the development of orbital cellulite. This form of the disease is manifested by swelling of the eyelids, chemosis, exophthalmos, limited eye mobility, and decreased vision. In the case when the accumulation of pus occurs between the periorbital wall and the bony wall of the orbit, destruction of the latter occurs, with the formation of a subperiosteal abscess. This stage is characterized by swelling and hyperemia of the upper eyelid, displacement of the eyeball in the opposite direction from the location of the abscess and limitation of its mobility. In addition, exophthalmos develops and a significant impairment of visual acuity occurs. With an abscess of the orbit, there is an accumulation of pus in the tissues of the orbit, due to which a cavity is formed, limited by the pyogenic membrane. In addition to the symptoms described above, with an abscess of the orbit, ophthalmoplegia often develops, compression of the optic nerve, and blindness occurs.
Diffuse inflammation of the orbital tissue indicates phlegmon of the orbit.
Treatment methods for phlegmon of the floor of the mouth
The first place a person comes with this disease is dentistry. Although this is a dental problem, the doctor should send him to the hospital. Since such patients are treated only by maxillofacial surgery.
Treatment of phlegmon of the floor of the mouth combines conservative and surgical methods. If there is pus, it is always necessary to open the source of infection, otherwise it will not resolve on its own. Access for drainage of infiltrate can be made through the mouth or through the skin, here the surgeon starts from where the infection is closest.
The most rational access to the purulent contents is an external incision along the midline going down from the lower jaw. It is safe and cosmetic. The scar remains practically invisible. Then a drain is inserted into the wound for several days. And the causative tooth is removed.
Afterwards, during the recovery period, the doctor must prescribe antiseptic care and antibiotics to eliminate the development and proliferation of microorganisms. In order for the wound to heal faster, vitamins and physical therapy can also be prescribed.
In Moscow, any maxillofacial hospitals, as well as specialized clinics, provide such treatment, each of which has its own price list for such an operation.
Rehabilitation therapy and rehabilitation
After surgical opening of the phlegmon, ointments, antibiotics and therapeutic techniques are prescribed that help remove residual pus from the wound and quickly cleanse the skin. Among products with herbal ingredients, preference is given to sea buckthorn oil, rosehip extract and Troxevasin ointment. If the wound does not heal for a long time and the skin does not tighten, the patient is prescribed dermoplasty.
Dermoplasty is a skin graft that is performed in case of severe damage to the dermis during trauma and extensive surgery. When removing phlegmon, this operation is prescribed in the case of removal of extensive inflammatory foci in which soft tissue necrosis has begun. In addition to the use of local remedies that promote rapid recovery and healing of the wound, the patient is prescribed conservative treatment methods aimed at restoring the immune system, relieving intoxication and preventing re-inflammation.
Bed rest is mandatory throughout the entire rehabilitation period. The area of the body where surgery was performed should be in a slightly elevated position. If there is pain, painkillers are prescribed and injected into the muscle.
All patients who have undergone surgery to remove cellulitis must take a course of antibiotics. The medications are prescribed by the attending physician depending on the individual characteristics of the patient and the type of virus that provoked the inflammation. If anaerobic cellulitis has been removed, intramuscular injections of anti-gangrenous serum are prescribed. To restore and normalize the acid-base balance, a solution of methenamine is prescribed. To restore tone to the walls of blood vessels, calcium chloride in solution is used.
To relieve the effects of intoxication and restore the functioning of the heart muscle and circulatory system, adonylene and caffeine are prescribed. Patients need to adhere to proper nutrition, it is imperative to exclude fatty and fried foods, and it is not recommended to consume large amounts of flour. Be sure to drink plenty of plain water; fruit compotes and fruit drinks are allowed to restore the immune system. Antibiotics are used until the inflammatory process is completely removed.
Diagnostics
In a clinical blood test with phlegmon, changes characteristic of purulent inflammation are present: leukocytosis, neutrophilia and a sharply increased ESR. When examining blood serum, C-reactive protein is detected.
The diagnosis is made by a dentist-therapist. It is based on the clinical manifestations of the disease, the patient’s subjective complaints, as well as the results of the necessary laboratory tests, which allow us to draw conclusions about the extent of the disease, the severity of the inflammatory process, and evaluate the effectiveness of therapy.
It is important not to confuse phlegmons and abscesses with facial boils and carbuncles, erysipelas, as well as inflammation of the submandibular and parotid salivary glands, since their external manifestations at the initial stage of the disease may be similar.
Forms of inflammation
With the development of phlegmon, the inflammatory process goes through several stages of formation. The initial stage is serous. With serous phlegmon, fluid—exudate—forms and accumulates under the skin, and leukocytes penetrate into the cells of the adipose tissue. Fatty tissue takes the form of jelly, completely saturated with exudate. There is a gradual spread of inflammation to healthy areas of soft tissue. If treatment is not carried out at this stage, the phlegmon passes into the next stage, putrefactive or purulent. It depends on what type of pathogenic microflora led to inflammation.
The purulent form provokes histolysis (in which the tissues melt and fill with pus). Due to histolysis, fluid begins to accumulate and may be greenish, cloudy white or yellow. The purulent type of neoplasm can lead to ulcers and fistulas. Without timely treatment, inflammation of purulent masses spreads to healthy tissue, cartilage and bones. At this stage of development of the inflammatory process, the muscles become loose, completely surrounded by pus, and appear gray and dirty. There is no internal bleeding.
The putrefactive form of phlegmon is characterized by rapid infection of soft tissues, which begin to deteriorate, and an unpleasant odor emanates from them. The tissues become brownish or greenish, their consistency is slippery and loose. With further development of phlegmon, soft tissues turn into a solid liquid mass. The main symptom of the putrefactive form of inflammation is severe intoxication of the body with a rapid deterioration in the patient’s condition.
Necrotic phlegmon is the death of destroyed soft tissues that are completely affected by purulent masses. If the tissues do not melt on their own, the body begins to reject them. At this stage of development of phlegmon, the inflammatory process begins to localize, multiple foci of abscess are formed, which can be opened independently. If there is too much accumulation of purulent masses that are deep under the skin, it is necessary to surgically open them and install drainage.
Anaerobic is the most severe stage of phlegmon, in which purulent masses infect adjacent healthy tissues, leading to their death, and gas is released. The fabrics have a fetid odor and are dark gray in color. If you press on the phlegmon, you can hear a crunch with which gas bubbles burst. The skin surrounding the source of inflammation becomes soft and loose, there is no redness.
Possible complications
Cellulitis is an extremely dangerous condition of the body, which without proper treatment can lead to severe intoxication and death of large areas of soft tissue. Chronic phlegmon is characterized by the absence of pronounced symptoms. The slow growth of pathogenic microflora allows the body to fight inflammation. During an exacerbation, a thickening occurs under the skin caused by the accumulation of infiltrate, which becomes woody. The skin around the inflammation becomes bluish.
The development of phlegmon on the lymph nodes is especially dangerous. This condition is fraught with the development of blood clots and sepsis. If the inflammatory process has not been completely treated and a small amount of pus remains on the soft tissues, a repeated purulent abscess may occur. Cellulitis that occurs on the face can lead to purulent meningitis.
cellulitis of the century
With further development of phlegmon, during which healthy tissues are affected, purulent arthritis, pleurisy, and osteomyelitis may occur. The most severe complication is the development of purulent arteritis, in which inflammation of the walls of large blood vessels - arteries - occurs, as a result of which the vessel begins to stratify and disintegrate. This pathological process can lead to severe internal bleeding.