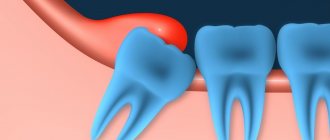
Pericoronitis is an inflammation of the soft tissues surrounding the crown of a partially erupted tooth. It affects the gums, tissues around the tooth and can spread to the immediate environment. The most typical place for pericoronitis to occur is wisdom teeth, third molars. Not only do they erupt later than everyone else (and sometimes do not appear above the surface at all), but they also have a special structure. A long stay in a “sleeping” form, the influence of neighboring teeth change the position of the third molar, and it begins to erupt sideways, at an angle, further damaging the gum from the inside, which provokes pericoronitis of the wisdom tooth.
Causes and factors contributing to the occurrence of pericoronitis
Inflammation of the mucous membrane and gums above the wisdom tooth, as well as associated with the formation of the so-called hood - folds of the mucous membrane - is the main cause of the disease. Pieces of food accumulate inside this hood, which are a good substrate for the growth of pathogenic bacteria. The combination of inflammation due to tooth eruption (often long, difficult, with injuries to the mucous membranes) and the hood with altered microflora leads to the formation of a focus of infection in this place.
Other common causes of pericoronitis
- Gingivitis and periodontitis as background processes for the formation of inflammation, the formation of a periodontal pocket, in which bacteria also accumulate. After this, the process moves on to the surrounding tissue.
- Local injuries. A typical phenomenon: an incorrectly filled or partially broken tooth digs into the gum opposite or next to it, constantly injuring it. This leads to inflammation. Sometimes pericoronitis occurs in people wearing orthodontic appliances, which can injure the mucous membrane.
- Polyodontia, or teeth in excess of a set.
Pericoronitis: treatment
If you have inflammation of the gums near the wisdom tooth, the treatment most often consists of a dental surgeon removing the hood over the wisdom tooth. However, if severe purulent inflammation is observed, then complete excision of the hood is undesirable immediately, because this can lead to various inflammatory complications.
In case of severe purulent inflammation, the hood is first only dissected to facilitate the outflow of purulent discharge, and anti-inflammatory therapy is prescribed. And the doctor will prescribe you for its complete removal after the active inflammation has subsided. Also, in some cases, the doctor may recommend immediately removing the wisdom tooth (24stoma.ru).
Excision of the hood over the wisdom tooth –
Removing the hood of a wisdom tooth involves excision of the overhanging mucous membrane over the erupting eighth tooth. Excision of the hood over the wisdom tooth leads to the elimination of conditions for the proliferation of pathogenic bacteria. This minor surgical procedure is usually less traumatic, but in some cases a large amount of gum tissue must be excised.
Excision of the hood over the wisdom tooth is performed by a dental surgeon under local anesthesia. The procedure is completely painless if you see a good specialist, if the anesthesia is administered correctly and a good anesthetic is used, and not something like novocaine. Pain will appear only after anesthesia has passed (after 30 minutes), so it is worth taking an analgesic even before the pain appears.
- Hood removal: price for 2021 in an economy class clinic in Moscow, a similar service costs about 2,500 rubles. In the regions, the cost of the procedure may be 2 times lower. By the way, in the clinic at your place of residence (if you have an insurance policy and a passport), you should undergo this intervention completely free of charge.
Stages of excision of the hood –
- Conducting local anesthesia,
- Using a scalpel and surgical scissors (less commonly, a surgical laser), the dental surgeon excises the gum overhanging the tooth.
- Treating the wound with antiseptics.
- An iodoform turunda is usually placed in place of the excised hood.
- The doctor gives recommendations and schedules a re-examination.
Removing a wisdom tooth hood: video
Please note that both hood excision operations are performed with a surgical laser and not with a scalpel. Using a laser avoids bleeding, swelling and severe pain. In Russian dental clinics, lasers are practically not used (due to their absence), and only a few clinics can boast of their presence.
After the intervention, the following are prescribed:
- Antiseptic baths with chlorhexidine solution 0.05% (3-4 times a day);
- Antibiotics are not prescribed in every case;
- for pain - good tablet analgesics.
Usually this is enough for you to completely forget what wisdom tooth pericoronitis is after 4-5 days.
However, if the doctor performed the operation traumatically, the pain may last for 7-10 days. If you want to remove inflammation as quickly as possible, then after antiseptic rinses, you can additionally apply CholisalGel to the hood 2 times a day in the morning and evening (it has a pronounced analgesic and anti-inflammatory effect). Remember that if you put gauze soaked in iodoform on the wound surface, you need to remove it yourself no later than the next day. Then it itself will become a breeding ground for infection. After you take out this turunda, it may cover a little. Then it is advisable to treat the wound with a gauze swab soaked in 3% hydrogen peroxide.
Important: in some cases, the hood may form again, in which case either a repeat operation may be required, or the issue of tooth extraction will be decided. Often these teeth are in an incorrect position. An experienced doctor can quickly determine the chances of the eighth tooth taking the correct position using an x-ray and external examination of the tooth.
In what cases is it better to immediately remove a tooth with a hood -
If your gums near your wisdom tooth are inflamed, the most radical treatment method will be the removal of the 8th tooth, above which the ill-fated hood appears.
This will solve the problem permanently, but you must be prepared for the fact that the eighth teeth may have curved roots (this can be checked by taking a photo) and then removal may be difficult. Situations where deletion is the best solution to the problem -
- Firstly , when the lower jaw is insufficiently long, which means there is not enough space for the eruption of a wisdom tooth. Removal in this case will prevent the remaining teeth from being displaced by the erupting tooth, and will prevent the development of crowding of teeth in the anterior part of the lower jaw.
- Secondly , if the 8th tooth has a strong inclination towards the cheek or the seventh tooth, then it will still have to be removed sooner or later, because it will injure either the buccal mucosa or the root of the 7th tooth, respectively.
For more information about the difficult eruption of wisdom teeth, read the article: → “Features of the growth and eruption of eighth teeth”
Symptoms of the disease
Symptoms of pericoronitis depend on the intensity and severity of the inflammatory process and the patient’s physical health. Signs of the disease can also be constant or periodically subside and be replaced by other complaints.
Possible general symptoms:
- Pain. It can intensify when you press on the source of inflammation, or it can be constant, pronounced or low-intensity. Sometimes it radiates to the ear, throat, nose, jaw.
- Redness or redness with an area of whitish skin.
- Swelling around the pericoronitis area.
- Unpleasant odor that gets worse after a night's sleep.
- Change in the taste of food, the appearance of a taste of blood or pus.
- Formation of a purulent sac on the gum.
- Difficulty opening the mouth, talking, chewing.
- Increased body temperature.
- General malaise.
- Difficulty sleeping.
- Enlargement of the cheek due to swelling of the jaw.
The course of the disease in different types of pericoronitis
Pericoronitis is divided into acute and chronic. Acute begins, as a rule, suddenly, is accompanied by inflammation of varying degrees of intensity, which affects the dental hood, spreads to surrounding tissues and, with severe inflammation, can cause complications from the body. This type of pericoronitis can occur as catarrhal and purulent.
In the case of catarrhal type, the disease occurs at normal body temperature and general satisfactory condition. Patients complain of pain when chewing or biting in the area of an erupting molar (or other cause of pericoronitis). With a long-term process, the lymph nodes under the lower jaw may become enlarged and painful.
If you look at the affected tooth, you can see that the hood or edge of the gum is red, there is swelling, in which the erupting tooth sometimes appears. Touching the source of inflammation is very painful, and when you press on it, serous fluid may be released. This form responds well to treatment. If the catarrhal form is not treated, then the inflammation can turn into a purulent form of acute pericoronitis.
In the purulent form of acute pericoronitis, the condition and well-being quickly deteriorate, the temperature rises to 38 ° C, the general condition, sleep, and appetite suffer. The pain becomes constant and severe. It radiates into the ear, into the back of the head, into the temple. Due to significant swelling, it becomes painful to swallow, open your mouth, and talk. The submandibular lymph nodes enlarge, sometimes so much that it becomes difficult to turn or tilt the head.
When you try to examine the source of inflammation, you can see that not only the hood of the wisdom tooth is swollen, but also the gums around the tooth. The swelling can also cover the inner surface of the cheek, the palate, and can spread all the way to the entrance to the oropharynx. If you touch this hood, the patient will experience sharp pain, and pus will be released from the lesion, sometimes smelling bad. Purulent pericoronitis responds well to treatment, however, it is possible that in an advanced case or with improperly selected treatment, the purulent process spreads to the jaw with the formation of phlegmon [1].
Chronic pericoronitis occurs if the acute one was not noticed, the inflammation on its own or with the help of medications went away or subsided. But since the actual cause is not eliminated, it periodically worsens and produces symptoms.
Most often, the process occurs at normal body temperature and satisfactory general condition. In this case, there is an aching, constant, rather pronounced pain, which can interfere with chewing and talking. Enlarged, mobile, painful submandibular lymph nodes can interfere with head movements. Soreness can radiate to the ear, temple, jaw, and throat. An unpleasant odor appears from the mouth; touching the area of inflammation with the tongue or accidentally pressing it is painful. If you look at the area of inflammation, you can see that the gums above the hood begin to lag behind the tooth. Chronic pericoronitis requires treatment. Otherwise, complications may develop, including the formation of ulcers and phlegmon.
Three ways to check if you have bad breath
- Lick your wrist and smell it. This is what the front part of the tongue smells like, and at the root of the tongue the “aroma” is usually much more intense.
- Take a spoon, lick it a few times and smell it. There will be saliva on it and it will smell just like your breath.
- Exhale into the mirror and immediately inhale deeply through your nose. The smell that you smelled is felt by others when communicating with you.
If your breath is bad, contact your dentist for help. Your doctor will help you find out the cause of bad breath and get rid of it.
Treatment of pericoronitis
Treatment of pericoronitis has several tasks:
- Eliminate pain.
- Combating the pathological process, preventing its further spread and preventing complications.
Typically, both acute and chronic pericoronitis are treated on an outpatient basis [1]. Elimination of pain is carried out simultaneously with the fight against acute inflammation. In case of catarrhal form, the doctor cleans and treats the gums and hood with an antiseptic and applies a special bandage, which simultaneously treats with medicinal impregnation and lifts the hood [1]. In this way, conditions are created for the process to subside and, if necessary, for the eruption of the third molar.
For purulent pericoronitis, surgical treatment may be required, which is also carried out in a dental clinic. The hood is excised, the wound is treated with special therapeutic bandages and the resulting pocket is lifted so that it does not again begin to interfere with the tooth and does not provoke inflammation.
Anti-inflammatory drugs, antihistamines and antibiotics may be prescribed. After the pain has subsided and the inflammation has subsided, the dentist evaluates the possibility of saving the tooth or the need to remove it. For this purpose, a complex of studies is carried out, including examination, laboratory tests, and x-rays. Based on the results of this examination, the tooth is either removed or given the opportunity and “space” to erupt.
After your wisdom tooth is removed, you will need to come back the next day for an examination.
This will allow you to assess the condition of the hole and mucosa. If the tooth is saved, it will need to be shown to a doctor once every 6 months. Clinical guidelines (treatment protocols) for the diagnosis of pericoronitis [1]
How to get rid of bad breath
Halitosis is not masked by the scent of bubble gum or mint candy. To get rid of an unpleasant odor, you need to reduce the number of bacteria. This can be done only by removing tartar and plaque.
How to eliminate bad breath
- Use floss and irrigator to clean the interdental spaces.
- Use a special brush to clean your tongue, paying special attention to its root.
- Drink at least 2 liters of clean water per day.
- Visit your dentist regularly.
- Once every six months, undergo a professional hygiene procedure.
If you urgently need to freshen your breath, you can use special rinses or infusions of peppermint, string and cumin. There are also aerosol fresheners and special lollipops. True, the effect will be temporary and the smell will return very quickly.
Recommendations for patients
If an incision or excision of the hood was performed in the treatment of pericoronitis, it will be necessary to follow several preparatory and postoperative measures that will speed up healing and reduce the risk of complications.
- For two to three hours after the intervention, do not take food, hot drinks, or alcoholic drinks.
- On the day of the operation, do not go to the bathhouse, sauna, take a hot bath, or be in the sun or in a hot room.
- Limit physical activity the day before and on the day of treatment.
- During these days and the next three days, it is recommended to follow a diet, exclude alcohol, spicy, very hot foods.
- Before the intervention, you should not eat foods with a strong smell.
- Smokers should quit cigarettes the day before the hood excision, on the day of surgery, and two days after.
- For sanitation (cleaning and disinfection), you can use a mouth rinse with antiseptic solutions.
- After the intervention, the doctor will prescribe medications that accelerate healing.
- Do not apply warm compresses or ointments containing bee, snake, etc. venom.
- If after excision of the hood or placement of therapeutic turundas there is pain, severe swelling, increased discomfort, pain in the area of the submandibular lymph nodes, you need to consult a doctor to identify the cause and take action.
Is it possible to fight the unpleasant odor from under the crown?
Since the unpleasant smell is caused by rotting processes, while they continue, it is impossible to get rid of the smell. You can only reduce it a little during treatment. They can help:
- Mouth rinses. To do this, you can use special antiseptic solutions that your doctor will recommend. Decoctions of medicinal herbs, such as chamomile or oak, are also suitable.
- Professional hygiene. The denture must be removed and cleaned. If the crown was installed to treat partial edentia, we recommend professional cleaning.
- Careful daily oral hygiene. In addition to a toothbrush and toothpaste, you can use special devices. You can completely clean the oral cavity, including in hard-to-reach places, using an irrigator. The device delivers a stream of air under pressure, which completely cleans out any remaining food. To care for crowns and implants, special brushes are used - interproximal, beam. You can clean the spaces between teeth using floss and floss.