When installing a metal crown or metal ceramics on a tooth, the patient often does not know which procedures are necessary for him and which are harmful. If we are talking about a tooth with a removed nerve that needs to be saved from destruction by applying a crown, everything is clear. But if the tooth is healthy, is it worth opening it up and depulping it, that is, removing the nerve?
Until relatively recently, tooth depulpation was mandatory before prosthetics. In this way, orthopedic dentists tried to avoid possible complications - after all, if the tooth pulp under the crown becomes inflamed, the crown will have to be removed, and if it serves as a support for the bridge, then the entire bridge. It will not be possible to install the same crown a second time after treatment - which means that all the work will have to start all over again - which will not please the patient at all. Therefore, just in case, the nerves of all prosthetic teeth were removed - this is relatively quick and makes the work much easier. Why has depulpation before prosthetics become quite a rare occurrence today?
What is depulpation and what is its essence?
What does tooth depulpation mean? Let's break the word down into parts - “de” means “removal”, and “pulp” refers to the soft neurovascular bundle that is located inside the tooth cavity and in the root canals. That is, depulpation or depulpation is the removal of the so-called “dental nerve”. After which the “empty” areas are filled with filling mass or pins, and then closed with crowns, inlays or special fasteners for dentures. Depulpation[1] is irreversible, i.e. a new pulp does not form in place of the removed one. Dental tissues cease to receive nutrition from the inside, and the tooth itself is considered “dead.” But this does not mean at all that it will fall out soon.
Any dentist should be able to carry out this procedure, but in the field of work this is most often done by dental therapists or more specialized specialists - endodontists. That is, if a patient comes to an orthopedist for a prosthesis, then if pulp removal is necessary, he will refer the person to a dentist-therapist.
Depulpation during prosthetics
If you were going to do dental prosthetics, you must first prepare the tooth so that the crown is not larger than the usual size.
Before covering the tooth with a crown, it was filed down, removing 3 mm of tissue. In the case of a large pulp chamber, the doctor definitely depulps the tooth. Otherwise, the tooth will hurt under the crown.
If the patient has undergone depulpation and the person begins to experience pain, then it is not necessary to undergo prosthetics immediately. You need to wait for the pain to go away. If there is no pain for a long time, then it is already possible to create and install crowns.
What is the purpose of depulpation?
The goal of the procedure is to achieve several important results that will allow the patient to wear the prosthesis for a long time. Moreover, during the entire period of wearing the person will not be bothered by pain and the need to remove, for example, a crown. Let's take a closer look at what effect should be achieved:
- the pulp will not overheat during grinding of the stump and, accordingly, will not become inflamed (i.e., pulpitis will not appear under the crown),
- cariogenic bacteria will not penetrate into the pulp (i.e., pulpitis is again excluded),
- It will be possible to place pins or a core inlay into the canals: this will strengthen the restoration, i.e. it will last longer.
Don't know what type of prosthetics to choose?
We will help in the selection, advise where to read more information and compare types of prosthetics.
Consultation with an orthopedic doctor in Moscow clinics is free! Call now or request a call
Working hours: from 9:00 to 21:00 - seven days a week
When a nerve must be removed - indications
Whether tooth depulpation is necessary before prosthetics or not, only a doctor can say after a thorough examination - instrumental and x-ray. Mandatory removal of the dental nerve is necessary for the following indications:
- there are signs of pulpitis, i.e. inflammatory process of the pulp: pain, darkening of the deep layers of dentin,
- the top of the tooth is severely damaged,
- the natural crown has massive fillings,
- the patient often experiences relapses of caries,
- it is planned to install a crown with thick walls (for example, metal-ceramic): in this case, it is necessary to sharpen the stump quite strongly, which will lead to thinning of the dentinal layer (i.e., the pulp underneath will be less protected) and to its potential overheating during treatment with a drill. As a result, if depulpation is not performed, the risk of pulpitis increases and the time for re-prosthetics approaches.
Indications for removal
The more tissue that is removed during tooth preparation, the higher the risk of opening the pulp chamber. To avoid this, the nerve is removed before prosthetics. This is also done if:
- in the presence of a large cavity, due to which the dentin layer after preparation will become too thin to perform protective functions;
- when teeth move out or lengthen;
- when tilting, turning and abnormal positioning;
- in some cases in patients with periodontitis;
- with increased tooth wear of 2-3 degrees;
- when using large volume stump inlays;
- with increased tooth sensitivity that persists after treatment;
- when the neck of the tooth is exposed as a result of gum recession (loss).
In these cases, the pulp is removed even with healthy teeth. Also, manipulation is carried out in cases of root fracture, multiple caries and pulpitis (inflammation of the pulp).
When can you do without deletion?
Let's consider situations when depulpation can be abandoned, i.e. do not perform it before prosthetics:
- the stump (ground tooth tip) has thick walls,
- the pulp is not inflamed,
- in the future there is no risk of caries/pulpitis under the denture,
- overheating of dentin and pulp is excluded.
For veneers and restorative inlays, you can, in principle, do without depulpation altogether, as well as for thin ceramic crowns - but only if all the requirements just outlined are met.
What happens to a pulpless tooth?
Depulpation significantly reduces the risk of complications, but it has its drawbacks.
- Change in enamel color. Teeth become more dull and unnatural.
- Changes in the properties of enamel: when exposed to negative factors, it begins to collapse.
In other words, the tooth loses its natural properties, so to protect it, a crown is installed.
Contraindications to the procedure
Contraindication is children's age. Or rather, a milk bite - here it is forbidden to go through root canals with instruments, because... the developing rudiments of permanent teeth can be damaged. Intolerance or prohibition of the administration of anesthesia is also a contraindication. As well as serious mental disorders, when a person can unknowingly harm himself during dental procedures.
Read on the topic: indications and contraindications for installing dentures.
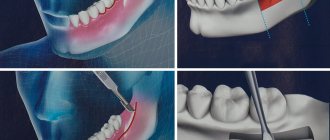
How is the procedure performed?
How is tooth depulpation done? It is carried out in at least 2 visits to the clinic. In one visit, removing the pulp and immediately placing a filling or pin can be dangerous because if pathological areas remain in the cavities, then over time inflammation will develop under the prosthesis. Next, we will consider how depulpation occurs and what stages are included in it.
First visit to the doctor
First of all, the patient is given an x-ray to find out the condition of the pulp and the presence of inflammation under the roots. Then they give a “freezing” injection with an anesthetic. To remove the pulp, the dentist needs to drill out part of the hard tissues - enamel and dentin. First, the pulp is removed from the pulp chamber. And then, using special endodontic instruments, you will need to remove all the loose pulp from the canals. After this, medicine is put inside and a temporary filling is placed, which lasts for an average of 7-14 days. During the process, you need to take an x-ray to assess the quality of the work. And in the most modern clinics, canals are treated under a microscope.
If the pulp is removed using arsenic paste, the treatment technology is different. Anesthesia is not required here, because... it does not hurt. Paste is placed into the cavity and closed with a filling. After 2-3 days, the patient must return to the clinic, because... It is during this time that arsenic will “kill” the pulp bundle and may begin to negatively affect healthy tissue. If the filling falls out or is damaged, you should immediately contact the clinic.
Second visit to the dentist
At the second appointment with the doctor, the medicine or arsenic paste is removed, the canals are processed, dried and sealed. Next, you again need to take an x-ray to assess the quality of the filling and the absence of “empty” areas. The patient is sent to an orthopedist, where the doctor will unseal the canal a little and place a pin, stump tab or attachment (lock) for a removable denture into it, and then take impressions for a crown or other orthopedic structure.
Stages of the depulpation process
- X-ray – necessary to assess the condition of the pulp, the number, length and branching of the canals to be filled.
- Anesthesia - local or complete anesthesia completely covers the issue of pain when removing a nerve (it doesn’t hurt!). At the same time, general anesthesia is used relatively rarely - when treating children, with true dental phobia, etc.
- Installation of a rubber dam - a latex film for insulating a tooth. A modern solution to improve the dentist’s working conditions and protect against the possible spread of microorganisms through saliva.
- The actual removal of the nerve is the excision of tissues affected by caries, opening the pulp chamber and extracting the nerve with a special instrument (pulpoextractor). In modern practice, this is a careful cutting of the pulp without affecting sensitive areas.
- Installation of a temporary filling (for a period of 1-2 weeks).
- Control x-ray.
If the x-ray and the condition of the tooth are satisfactory, after the control period a permanent filling is installed.
The appearance of pain and its causes
Why does a tooth hurt after pulp removal? Soreness often occurs after the anesthetic injection wears off. Pain after the procedure occurs for several reasons - normal and pathological. Here you need to understand the nature of the pain and what it is talking about.
For example, if the pain is tolerable or can be easily eliminated with painkillers, if it weakens every day, then this is a variant of the norm. After all, during the passage and expansion of the channels, healthy tissues were slightly injured, and pain is a natural reaction of the body. How long can a tooth without a nerve hurt after the procedure? On average, the discomfort goes away completely in 7-14 days. But in some patients it persists for 4-6 weeks and then disappears.
Read on the topic: what to do if a tooth hurts under a crown - causes of pain and methods for eliminating it.
The pathology is considered to be severe pain for several days, which is practically not relieved by pills. And also the reappearance of pain a few days or weeks after a period of painlessness. Symptoms such as severe redness and swelling of the gums, fever, headache, and bad breath should alert you. These signs most likely indicate that the depulpation was carried out incorrectly and inflammation began under the prosthesis. Or aggressive caries develops under the crown. Dental care is needed here, otherwise complications may arise - periodontitis, for example.
Possible complications
A medical error associated with poor-quality disinfection of the canal when removing a nerve can trigger the process of suppuration with subsequent transition to a periodontal abscess (in the absence of adequate treatment). This complication leads to the need for tooth extraction.
Other possible complications:
- Pain for several days after nerve removal. The duration of discomfort is individual for each patient; if pain persists for a long time, it is necessary to consult a doctor to re-open the canals and carry out disinfection.
- Increased bleeding of the canal occurs when the pulp extractor is removed after the pulp has been torn off. To avoid this phenomenon, many specialists carry out the procedure in stages with copious rinsing of the tissues with an antiseptic. Bleeding control is carried out directly at the appointment.
- The appearance of granuloma, fistula, cyst, gumboil.
Specific problems can arise if the material is applied incorrectly: if the filling extends beyond the boundaries of the root apex, the jaw nerve may be pinched.
If you experience pain in the lips and chin, you should urgently consult a dentist: a possible complication is facial paralysis.
How long will a tooth last with and without a nerve?
It all depends on the skill of the doctor, on how competently he assessed the future functionality of the tooth with or without the preserved nerve. If metabolic processes are maintained in the supporting unit (i.e., while the pulp is preserved), then its service life is expected to be longer than that of the pulpless one. When all the conditions on the part of the dentist are met, and the patient treats the restorations with care, then, if the nerve is preserved, the support under the prosthesis can last on average 8-10 years (under a single crown) and about 7 years under an extended structure. If a tooth is “dead,” then its service life is shorter by an average of 30%, i.e. about 5 years.
But if the prosthetics are performed poorly, if the patient does not take good care of the prostheses, then the nerve may become inflamed - and very soon treatment and a new orthopedic design will be required.
Tooth removal
Depulpation (depulpation of a tooth) is the removal of pulp, connective tissue consisting of blood vessels and nerve endings. Removing the tooth nerve and cleaning the canals is designed to relieve the patient from pain, inflammation and further complications. However, the tooth, having lost its blood supply, becomes dead and, therefore, more fragile.
Dental treatment and nerve removal is one of the most common dental procedures. This is partly because patients turn to the dentist only in case of unbearable pain, when it is no longer possible to do without depulpation. Removing the nerve of the tooth and filling the canals allows you to preserve the natural tooth, which is a priority for endodontic treatment.
Indications for depulpation:
- extensive caries
- classic pulpitis and infectious pulpitis (bacteria penetrate through the root apex)
- trauma and damage to the tooth affecting the pulp
- if it is necessary to install crowns or classic bridges
Many patients who come to the dentist's office with toothache are interested in the question: is it possible to save the pulp? Today, there are methods of biological treatment (preservation of the entire pulp) and vital amputation (preservation of the root pulp), but many favorable factors must converge for them to be carried out. For example, biological treatment is not carried out after 25 years.
Does the shade of dental tissue change after the procedure?
Does the tooth darken after depulpation? Yes, over time the color will change - it will become gray and lifeless, because the tissues do not receive nutrition from the inside. But the pulpless unit is covered with a prosthesis - so the change in shade will be completely invisible from the outside. If the color of the prosthesis itself has changed, then the reason for this may be the following:
- the use of low-quality materials for manufacturing or non-compliance with its technology,
- staining from coffee, wine, food coloring, tobacco,
- formation of plaque and stone due to poor oral hygiene.
When is depulpation prescribed?
An intervention of this kind is necessary when it is necessary to stop pathological processes in the soft tissues of the tooth. Indications for the procedure are:
- sharp pain followed by prolonged aching pain;
- caries, which destroyed the protective tissues of the tooth and caused inflammatory processes in the pulp;
- pulpitis, requiring complete or partial removal of the pulp;
- periodontitis;
- mechanical damage to the tooth, which resulted in exposure of the neurovascular bundle;
- prosthetics;
- dental defects;
- there is excessive tooth wear;
Before carrying out the depulpation procedure, the specialist must conduct a visual and instrumental examination of the patient. After collecting an anamnesis, taking into account the analysis of x-rays, the doctor determines the feasibility of the manipulation.
Important: Sometimes before depulping, professional teeth cleaning is carried out: removing plaque and tartar. Manipulations are recommended if without them it is not possible to obtain a long-term result.
Prosthetics after tooth depulpation
After removing the tissues that fill the tooth cavity, containing blood vessels and nerves, the tooth is considered “dead.” He becomes vulnerable and brittle. To prevent the destruction of the dental element in the future, the doctor recommends installing a crown on it after depulping the tooth. When filling, the pulp is replaced with a composite material. The sealed element of the dentition, along with other teeth, participates in the processes of chewing food and is subjected to significant loads. To prevent staining of the filling, it is covered with a crown.
Depulpation of teeth during prosthetics
But there is also the exact opposite process. If the patient wishes to install a permanent denture, the specialist must examine the teeth that will be involved in the procedure. In some cases, the dentist prescribes pulpotomy of all or some elements of the dentition:
- with increased tooth sensitivity;
- in case of deformation and incorrect positioning of the tooth in the row;
- with initial signs of pulpitis;
- for chronic caries.
Depulpation before prosthetics is carried out, since after installing a permanent prosthesis, it will be more difficult to treat the tooth; you will need to remove the bridge or crown, which is a traumatic factor. In addition, under the bridge, pathological processes can develop much faster and be more widespread.
Whitening of pulpless teeth
After pulp removal, teeth become susceptible to external factors. They can quickly lose their aesthetic appeal as they darken. In this case, a color restoration procedure is recommended. It is called “endobleaching”. The essence of the manipulation is the introduction of a lightening substance into the tooth. Endobleaching is performed without pain.
Indications for tooth whitening after pulp removal are:
- filling with a coloring composition;
- darkening of dentin under the influence of dyes: tea, coffee, nicotine.
Endo-stripping involves removing the filling and cleaning the composite material from colored particles. Bleach is injected into the existing cavity, and the tooth cavity is covered with a temporary filling that will last two weeks.
When you visit the dentist again, the temporary filling and coloring material are removed. The tooth is restored with special materials. The recommended frequency is once a year.
Consequences of tooth depulpation
Sometimes after removal of the nerve, the patient feels pain in the tooth, and swelling of the gums is observed. Reaction to cold and hot food or mechanical stress can be caused by:
- the body's reflex to remove the pulp;
- poorly performed depulpation procedure;
- the presence of nerves that were not removed;
- using unsuitable filling material;
- inflammation of the gums caused by tissue trauma during treatment;
- the presence of pathological processes in the adjacent element of the dentition, when the pain radiates to the “dead” tooth.
Only a specialist can determine the cause of the pain. If the pain is caused by inflammatory processes, a specialist may prescribe antibiotics. If the sensations are caused by a poor-quality depulpation procedure, it is necessary to re-open the canals, clean them, and restore the tooth with a composite. If you ignore prolonged painful sensations, a gumboil, fistula or cyst may develop.
Tooth removal: contraindications
Dental pulpotomy is not performed for the following diagnoses and conditions:
- acute leukemia;
- chronic heart disease;
- pregnancy;
- infectious hepatitis;
- stomatitis in acute or chronic stages;
- hemorrhagic diathesis;
- inflammatory diseases of the oral cavity and upper respiratory tract.
If there are contraindications to pulp removal, the dentist should offer an alternative treatment method.
How long will a tooth last after pulpotomy?
It is important to understand that the resource of a pulpless tooth may vary from patient to patient. Even in one person, two different teeth after depulpation can “behave” differently.
If the procedure is carried out in compliance with the protocol, the canals are thoroughly cleaned, their sealing is achieved, and pathological tissue is completely removed, the tooth can last several decades. The service life of a tooth after pulpotomy increases significantly if a high-quality and reliable crown is installed on it.
How to avoid tooth depulpation?
If pathological processes are already running, it will not be possible to avoid the procedure. If left untreated, the tooth will be lost. It is possible to exclude depulpation only if the occurrence of pathological processes is prevented. In this case, prevention is the best ally.
Careful care of the oral cavity with well-chosen products, a nutritious and balanced diet, and regular visits to the dentist will help keep the elements of the dentition healthy and prevent the development of caries and other pathologies.
What complications may arise
During the process of removing the dental nerve, the following complications may occur:
- perforation of the root wall,
- exit of the instrument or filling mass beyond the root: as a result, periodontitis begins - root inflammation,
- fracture of the instrument in the root canal: such fragments are very difficult to remove, sometimes the entire tooth has to be removed.
Many dentists perform pulp removal only to insure against possible complications after prosthetics - caries or periodontitis. After all, then you will have to remove the prosthesis, treat the tooth, and then make a new prosthesis, because the old one either cannot be removed without damage, or it will not fit on a fresh filling or stump inlay. But let us repeat once again, they will not remove the nerve without clear indications.
Why is it necessary to depulp a tooth during prosthetics, indications for the procedure
The need for pulp removal is a controversial issue with considerable debate among many dentists. On the one hand, every doctor tries to preserve living teeth, if there is even the slightest opportunity for this, because a tooth without a nerve becomes fragile: the nutrition of the enamel is lost. In addition, the “empty” tooth becomes insensitive and will not be able to give a signal about caries or other diseases.
On the other hand, the pulp is exposed during prosthetics, and, sooner or later, makes itself felt. Also, after the installation of a dental implant, pain symptoms may occur, the cause of which can only be understood after removing the artificial tooth, which will then be unusable.
Depulping a tooth before prosthetics is 100% necessary for:
- advanced caries that affects the pulp;
- inflammation in the pulp chamber or periodontitis;
- teeth tilted more than 10 degrees;
- presence of enamel hypersensitivity;
- having low, small teeth or their abnormal alignment.
Features of care after removal
Oral care after dental nerve removal and prosthetics must be regular and thorough. Twice a day you need to use a brush and paste, follow the correct cleaning technique (only sweeping movements). It is recommended to rinse your mouth after each meal, and also to exclude toffees, chewing gum, hard pieces of food, and not to chew nut shells or seeds. In order to promptly identify and eliminate dental problems, you should visit an orthopedic dentist at least 1-2 times a year.
“I had a crown placed on a post about 7 years ago. They did it very well and treated it under a microscope. But after the prosthetics, the dentist told me not to forget to come to them every year or every six months for an examination. At the same time, professional hygiene was carried out. I’ve never had any problems in all this time, I eat whatever I want.”
Anna, review from irecommend.ru
Advantages and disadvantages of depulpation
The advantages of tooth depulpation are that it will eliminate or almost completely minimize the risks of pathologies appearing under the prosthesis - it all depends on the skill of the dentist and the patient’s attitude towards the new smile. The disadvantage is that the tooth will become “dead”, i.e. more fragile and with a shorter service life than non-pulpless. But these shortcomings are eliminated, again, by high-quality treatment and materials, and competent care of restorations, as well as the absence of extremely high chewing loads.
How much does depulpation cost?
How much does tooth removal cost? The cost of the procedure ranges from 3000-4000 rubles per 1 tooth in small cities, and in large cities, when treated under a microscope, from 3000-4000 rubles per 1 root canal (there can be 3-4 of them in one tooth). It is more profitable if the clinic offers turnkey installation of the prosthesis - absolutely all manipulations, examinations and materials are included in the total price.
[1] Shashmurina V.R. Biomechanical features of dental depulpation, 2022.
Author: Dulgarov Zh. G. (Thank you for your help in writing the article and the information provided)
Change in enamel color after nerve removal
If the dental clinic follows international depulpation protocols, such phenomena are excluded. However, in budgetary institutions there are frequent cases of using outdated practices.
The color of the enamel after nerve removal can be affected by:
- Improper preparation of the tooth for installation of a filling;
- Poor quality instrumental processing of channels;
- Low quality filling materials.
Thus, when using resorcinol-formalin paste (the use of the material is practiced in the treatment of baby teeth), the enamel acquires a pinkish tint; When using endomethasone, the tooth may turn yellow after a few years.