Tooth extraction is a process that traumatizes the gums. After healing a diseased tooth, nerves, ligaments and small blood vessels are torn, which causes bleeding. This is a natural process - the blood does not allow pathogenic organisms to enter the circulatory system, washing them out. And then, curled up, it forms a barrier between unprotected tissues and bacteria. After tooth extraction, white plaque on the gum is not pus, but another stage of protection and restoration of the body.
When removing a tooth, the patient must be prepared:
➢
to moderate bleeding that may last for some time;
➢
the appearance of a dense blood clot in the gum;
➢
unpleasant odor 10-12 hours after surgery;
➢
the formation of a white coating on the blood clot;
➢
pain after surgery;
➢
temperature rise.
The listed symptoms are not a sign of an unsuccessful operation or infection in the body - this is the body’s natural response to tooth extraction.
What is white plaque on the wound after tooth extraction?
A few hours after the tooth is removed, a dark clot appears in the socket - bluish, black, red or brown. This clot is blood, and it is the primary protection of the socket from bacteria or pieces of food entering it. On the 2nd - 4th day, the patient may see that a coating appears on the clot - yellowish, gray or white. The deposit looks like pus and, together with the resulting bad breath, can alert the patient. However, there is no need to be alarmed - this plaque is not a sign of wound decay and indicates a normal healing process. This special protein compound is fibrin.
A milky plaque (fibrinous) can be very dense, hard or soft. This is no cause for concern. If you come to the dentist with this question for an unscheduled appointment, the specialist will tell you that everything is in order and there is no need to remove the film.
If the film is not removed and the wound is not disturbed, active processes will occur underneath it:
- the blood clot will begin to dissolve;
- the hole will begin to decrease in size;
- young cells, osteoblasts, will begin to move from the edge of the wound to the center;
- The gums will begin to close the wound.
Fibrinous plaque after tooth extraction is a natural stage of gradual recovery of the body, in which it is better not to interfere.
Is plaque on the gums always considered normal?
The appearance of plaque in the oral cavity is noted by most patients after implantation. Natural processes and developing diseases during surgical intervention can contribute to the formation of a white to dark gray film.
Fibrinous plaque on a wound - how to distinguish it from inflammation
Often, a white coating appears on the surface of the gum during healing, which is formed from protein during blood clotting and is a natural defense that prevents infection from penetrating deep into the wound. This plaque is called fibrin , it should not cause concern.
There are situations when plaque is a sign of an inflammatory process or rejection of the structure. It differs in color and appearance, but only a doctor can determine this.
To independently distinguish normality from pathology, you need to take into account the healing process:
- On the day of implantation, a dark red or burgundy blood clot appears, and the mucous membrane may be swollen.
- On the second day, a white fibrin coating forms. The swelling may increase.
- With normal healing, plaque on the gums dissolves within 7 days after the formation of the epithelial barrier (the process of bone regeneration will continue for up to 3-6 months).
- On days 3-7, the swelling completely disappears, and the mucous membrane acquires a natural color. Sometimes fibrous plaque can still persist while epithelial tissue grows underneath it.
- By days 10-14, there is practically no plaque observed, the gums are covered with new tissue.
Implantologist's opinion : “After installation of the implant, the patient must note all changes in the oral cavity. The main sign of successful implantation is normal health. The white plaque does not need to be removed, as patients try to do, it is a natural protective reaction of the body. If by the end of the week the swelling and pain have disappeared, then there is nothing to worry about.
You need to carefully monitor any changes in your health, and if you have suspicious symptoms, immediately consult a doctor. After all, he is responsible for the results of the work performed and your condition. This means that it is within his competence to detect the problem even before the appearance of the first clinical symptoms.”
Manifestation of stomatitis
Stomatitis is a lesion of the oral mucosa that occurs in approximately 20% of people. At the initial stage, it manifests itself in the form of redness, swelling, burning, and then develops, turning into blisters or painful sores of a round or oval shape. They are white or gray in color, with a film on top and a red halo.
The disease lasts about 4-14 days. If once it appears, there is a possibility of relapses (repetitions). The typical frequency of exacerbations is 3-4 times a year. The ulcers heal calmly, leaving no traces.
The main reason for the appearance of plaque during stomatitis is considered to be the reaction of the immune system to irritants - when it cannot recognize new molecules. This provokes an attack of lymphocytes and leads to the formation of ulcers.
The development of stomatitis is promoted:
- insufficient hygiene;
- smoking, drinking alcohol;
- side effects of chemotherapy;
- dehydration (with prolonged elevated temperature, vomiting, diarrhea, blood loss);
- antibiotic therapy after tooth extraction and implant installation;
- low-quality or poorly installed implants.
Risk factors for stomatitis include:
- Gastrointestinal diseases: colitis, gastritis, duodenitis, helminthic infestation.
- mouthwashes and toothpastes containing sodium lauryl sulfate;
- emotional/mental stress;
- genetic predisposition;
- hormonal changes;
- mechanical trauma to soft tissues in the oral cavity (appears from hard food, sharp tooth fragments, uneven edges of the crown, etc.);
- bacteria and harmful microorganisms (can penetrate the wound during implantation);
- systemic diseases or malignant tumors;
- insufficient amount of vitamins and minerals in the body;
- increased tissue sensitivity;
- allergic reactions.
Treatment of stomatitis is carried out using two methods: local impact on the affected area and general strengthening of the immune system.
Among the medications prescribed are antibacterial and antiviral agents, ointments that accelerate the restoration of damaged epithelium. It is recommended to rinse the mouth with medicinal compounds and liquid antiseptics.
When rinsing the mouth, avoid swallowing medications.
In order to restore immunity, a course of intensive immunization, general strengthening procedures are prescribed, and stress factors are limited. Vitamins and a balanced diet will have a positive effect.
Effective folk methods:
- rinsing with soda solution;
- aloe and kalanchoe juice;
- flax seeds;
- egg white;
- tea mushroom;
- viburnum with honey;
- carrot juice;
- blueberry;
- onion broth;
- green tea;
- tincture of propolis or echinacea;
- decoctions of medicinal herbs (chamomile, St. John's wort, millennial, calendula, sage, oak, burdock root and seeds).
Why you don’t need to remove white plaque after tooth extraction
In some cases, patients intentionally or accidentally remove a blood clot or fibrinous film from the socket. This is not necessary, since removing a clot or film can provoke negative processes.
First of all, an open wound provides access for bacteria to the circulatory system and tissues of the maxillofacial apparatus. Infection can cause serious consequences and require long-term treatment with antibiotics. Also, removing the clot and white plaque increases the pain, since an open wound is more sensitive to any irritants, including drinking drinks and food, during a conversation.
Finally, plaque on the gums after tooth extraction does not need to be cleaned off because this can cause re-bleeding and prolong the wound healing stage.
In any case, there is no need to intentionally remove plaque; this can cause:
- serious complications;
- severe pain;
- improper gum formation;
- long recovery process after tooth extraction.
To avoid accidentally damaging the socket, blood clot or fibrinous film, you must follow the recommendations given by the doctor after the operation.
Treatment methods
Before consulting a doctor, you should not self-medicate or use folk remedies, as this can only speed up rejection.
Comprehensive treatment of reimplantitis at an early stage may include:
- crown removal,
- opening the formation, removing pus, treating tissue with antiseptics or exposure to a laser beam,
- cleaning and reinstallation of the crown,
- taking antibiotics, anti-inflammatory and painkillers.
If the inflammatory process is advanced, the doctor will have to remove the implant. After this, the cavity is cleared of pus and medications are prescribed that will help stop the inflammation, relieve pain and swelling. After final restoration, reimplantation is performed. If the volume of bone tissue is not enough to reinstall the prosthesis, bone grafting is first prescribed.
To prevent relapse of reimplantitis, you need to:
- quit smoking
- use brushes, pastes and rinses recommended by your doctor for oral care,
- Regularly undergo preventive examinations at the dentist and have your teeth professionally cleaned.
How not to damage white plaque after wisdom tooth removal
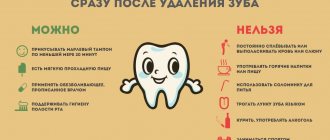
To eliminate the risk of complications and speed up the recovery process, you need to follow the rules of behavior after tooth extraction:
- do not eat or drink for 3 hours after surgery;
- stop smoking and drinking alcohol for a while;
- do not heat the cheek and gums, avoid overheating;
- for the first 24 hours, do not rinse your mouth or brush your teeth;
- Do not go to the bathhouse for a week, do not play sports.
Smoking is contraindicated, as it provokes vasospasm: the bleeding stops too quickly, the blood clot is not formed enough. Hot drinks, warming the cheek, sports training and visiting a bathhouse cause overheating of the body and dilation of blood vessels, which can cause re-bleeding, opening and infection of the wound.
Rinsing and brushing the mouth are acceptable 24 hours after tooth extraction, but they should not be overly vigorous. Hygienic procedures must be moderate so that the blood clot remains in the cavity and the subsequently formed fibrinous protective layer is not damaged. During the recovery period, food should be chewed only on the non-operated side of the jaw.
If you have a fever and severe pain in the first few days after tooth extraction, you can take Paracetamol - this will help reduce discomfort and improve your well-being.
Why don't implants take root?
Doctors identify several main factors that provoke the development of reimplantitis. These include:
- insufficient diagnostics before starting prosthetics,
- low quality of materials from which the pins and crowns are made,
- violation of installation rules,
- non-compliance with the rules of oral care after surgery,
- smoking and other bad habits,
- decreased immunity.
To avoid rejection, you need to carefully choose a clinic and a doctor, and strictly follow all his recommendations before and after the intervention. Rejection can begin either a few days or several years after installation, so it is important to carefully monitor the condition of your oral cavity and undergo regular preventive examinations with your dentist.
When white plaque on a wound after tooth extraction requires examination by a doctor
Despite the fact that white plaque after wisdom tooth removal is a natural reaction, the patient needs to conduct a daily self-examination of the oral cavity and consult a doctor for help if alarming symptoms appear.
You should consult a doctor if:
➢
on the 3rd - 4th day the pain does not decrease, it becomes throbbing and intense;
➢
a white, reddish or yellow mass or liquid is released from the wound;
➢
swelling of the gums has intensified or spread to the face;
➢
body temperature rose above 38 degrees.
These signs indicate possible infection or complications. After examining the oral cavity, the dentist, if necessary, may prescribe a course of antibiotics or surgical cleaning of the socket cavity.
What is leukoplakia?
If you look into your mouth, only your teeth will be white. And if your gums are white, you may have leukoplakia. According to the Mayo Clinic, leukoplakia is a condition in which thick white patches form on the gums, underside of the tongue, and inside of the cheeks. They can even form on the tongue, and the white spots cannot be erased or scraped off the surface. Medical science has yet to determine what exactly causes leukoplakia, but one of the most likely causes is thought to be tobacco use. The cause may also be chronic alcohol dependence. Most cases of leukoplakia are benign. However, in some cases it is an early symptom of cancer. Cases of oral cancer that develop under the tongue at the bottom of the mouth are sometimes accompanied by leukoplakia plaques. One of the precancerous conditions is known as dysplasia. Dysplasia can be mild, moderate, or severe according to the American Cancer Society classification. The severity of dysplasia determines its development into cancer or spontaneous resolution.
Gum healing
After tooth extraction, you need to be prepared for the fact that pain and swelling may intensify on the second day after surgery. But already on the 3rd - 4th day after the operation, the discomfort will begin to decrease. By this time, the wound healing processes are more active, and by touching the tip of the tongue to the hole, you can feel that a compaction has formed.
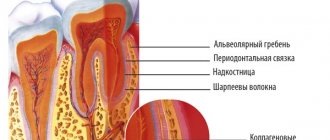
During this period, the following are actively developing:
- bone formation in the area of the removed tooth root;
- narrowing of the socket due to the “growth” of the gums;
- formation of the mucous membrane in the socket area.
Fibrinous plaque after tooth extraction persists for a week. It disappears on its own, without mechanical cleaning. Little by little, the mucous membrane begins to turn pink, gradually acquiring a healthy, natural color. Around the 10th day, wound healing is completed: healthy tissue is formed that covers the mouth of the hole. A small depression remains in the area of the removed tooth. The formation of bone tissue at the site of tooth extraction takes much longer - up to 6 months. Changes will be visible on an x-ray.
Natural symptoms after implant placement
- Minor pain syndrome (throbbing pain can appear with any physical activity);
- difficulty swallowing or sore throat;
- elevated body temperature on the first day after implantation;
- bleeding from the wound for 2 days;
- nosebleeds after sinus lift in the upper jaw;
- swelling in the area where the artificial root is implanted;
- numbness of the cheek, part of the tongue, lip or chin;
- whitish coating on the wound;
- increased drowsiness and fatigue;
- unpleasant smell.
You need to rest more so that the body can quickly restore injured tissue. But there are cases when you need to see a dentist.
Dentist's opinion : “Engraftment of the implant system is a complex process that directly depends on the patient’s health condition. When everything is fine, the symptoms that are considered normal after surgery will quickly pass. But if the situation worsens on day 3-4, there may be a risk of developing an inflammatory process or rejection of the structure. It is important not to miss this moment and consult a doctor in time.”
Causes of gingivitis
Most often, gingivitis develops as an independent disease, but sometimes the causes of its occurrence are acute and chronic diseases of the gastrointestinal tract, cardiovascular system, hematopoietic organs, infectious diseases, and changes in hormonal levels. In this case, gingivitis is one of the symptoms of the underlying pathology. The causes of gingivitis can be internal or external.
Internal reasons include:
- tooth growth that injures the gums - the eruption of wisdom teeth;
- vitamin deficiency, hypovitaminosis (most often lack of vitamin C and zinc);
- weakened immune system;
- metabolic disease;
- allergic diseases;
- diabetes;
- stress, mental illness;
- anomalies and various deformations of the gums;
- diseases of the gastrointestinal tract.
External reasons are a number of factors:
- physical (injuries, burns);
- chemical (the influence of aggressive substances);
- medical (incorrectly applied fillings, incorrectly installed veneers, traumatic wearing of braces);
- bad habits (smoking, mouth breathing);
- biological (infectious process);
- hygienic (insufficiently thorough hygienic procedures).
Toxins from microorganisms that enter the oral cavity with food and water, as well as those that live there permanently, form dental plaque (plaques) due to insufficient hygiene measures. They are the most common cause of the inflammatory process.
Inflammation can develop differently depending on the cause. Chronic catarrhal gingivitis occurs most often due to unsatisfactory hygiene measures or as a result of gum injury or burns. Hypertrophic gingivitis is caused by crowded teeth, incorrectly installed fillings or dental crowns, as well as changes in hormonal levels, for example, during pregnancy (pregnant gingivitis) or puberty (adolescent or juvenile gingivitis). Necrotizing ulcerative gingivitis (Vincent gingivitis) is usually caused by an infectious process. It occurs due to the activation of two microorganisms (Vincent spirochete and spindle bacillus) against a background of weakened immunity, hypothermia, stress or malnutrition.
Symptoms
The growth of the mucous membrane is a gradual process. There are 3 degrees:
- The gingival papillae increase in volume. The gingival contour is disrupted and hangs over the tooth.
- The growth progresses, the tissue covers up to half of the coronal part. Bleeding and discomfort when brushing teeth and eating food develop.
- The gum covers the tooth by two thirds, sometimes completely. Folds form in which microflora accumulate, causing inflammation.
The process is generalized
when the entire gum on the jaw suffers.
Focal
hyperplasia is located around one or more teeth.
The edematous form is characterized by the presence of plaque, there is a lot of it, it is quite soft, but covers the enamel with a thick layer. Gum pockets form. The papillae turn red and bleed when pressed.
Patients complain of itching, discomfort in the mouth while eating, and an unpleasant odor.
With fibrous gingival hyperplasia, patients are only concerned about the unusual appearance of the mucous membrane. There is usually no pain or bleeding, but there are complaints of an unpleasant odor.