Symptoms Possible causes Elements that may fall out What to do if they fall out How to avoid loss
Implantation is a successful and effective method of tooth restoration. The most technologically advanced and safe. But what to do if the implants do fall out? And who is to blame? Let’s say right away that according to long-term statistics, implant rejection occurs in only 1-2% of cases.
of the total. And the reasons why dental implants fall out have been studied enough to avoid this even at the stage of planning prosthetics on dental implants. But there are a number of factors that do not depend on the doctor. In this case, only the patient is responsible for the implant falling out.
What to do if part of the rod comes out of the gums
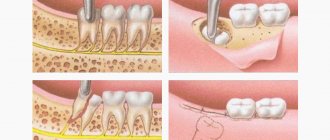
When the implant is exposed, a flap operation is performed to build up its soft tissue:
- A flap is peeled off from the palate and applied to the exposed area.
- If necessary, correction is carried out on the bone tissue.
- The edges of the wound are sutured with non-absorbable thread.
- After 10 days, the sutures are removed.
- After the artificial root has engrafted, a former is placed.
Another way to correct a defect with a lack of periodontal tissue can be the transition from a two-stage installation to a one-stage method. However, it is necessary to take into account that the one-stage technique has the main drawback - non-ideal conditions during the period of implant engraftment, high risks of developing inflammation.
What elements of implants can fall out?
The implant consists of several parts and during installation a plug, former and abutment are added to it:
- The healing abutment
fell out of the implant. The reason may be that the implant is planted too deep; it simply becomes overgrown with mucous membrane. Inflammation can also cause loss of the former; - plug
has fallen out - an error in the technology of its installation or non-compliance with the doctor’s recommendations; - pin
fell out . We discussed the reasons above.
In all cases, you should urgently contact your doctor.
Is implant failure a sign of rejection?
If the problem of exposing the rod is accompanied by additional symptoms, it is necessary to understand their causes. Pain at the site of installation of the structure, swelling, and redness of the gums during the first week after surgery is a normal reaction to surgery, since tissue injury occurs. Signs of rejection are the following situations:
- 1-2 weeks after implantation, acute pain does not go away;
- swelling and redness of the gums do not subside after 4 days after surgery;
- discharge of ichor, bleeding lasting more than 7 days;
- the mobility of the implant is felt;
- unpleasant smell from under the plug screw;
- painful sensations when pressing on the rod;
- the appearance of purulent discharge from the gums;
- increase in body temperature.
Plastic surgery of bone tissue and gums when the implant is exposed
The surgical intervention is aimed at building up bone tissue and gums to completely cover the surface of the implant, which is achieved by adding bone tissue and mucous membrane to the implant area. The operation is performed by an implantologist under local anesthesia.
increase in gum volume around the implant
Before the operation, a preparatory stage is required: sanitation of the oral cavity (treatment of caries and its complications, elimination of inflammatory processes in the oral cavity), removal of tartar (professional oral hygiene).
Restoration of gum recession around the implant is carried out in the following sequence:
- the exposed area of the implant is carefully treated with antiseptics;
- perform bone grafting (bone augmentation) in this area;
- in a selected area of the oral cavity (usually on the hard palate), a flap of the mucous membrane is peeled off;
- the flap is moved to a place with tissue deficiency;
- Sutures are placed at the site of tissue collection and at the extension site.
After the operation, the graft engraftment period begins, the sutures are removed on the tenth day.
Possible complications
Gum and bone grafting, like other types of surgical interventions, has the potential to develop complications:
- the occurrence of an allergic reaction to the anesthetic;
- repeated exposure of the implant (another operation is required in six months);
- swelling in the area of the operation;
- pain;
- bleeding;
- hematomas.
Such phenomena occur due to the abundant blood supply to the tissues of the maxillofacial area, therefore even minor surgical interventions, especially on the lower jaw, are accompanied by severe swelling and hematomas. However, after a couple of days they decrease and disappear completely within 1-2 weeks.
Soreness for several hours after surgery is considered normal and can be successfully relieved by taking analgesics. If pain increases and there are no positive changes after three days, you should see a doctor, as there is a risk of developing serious complications.
Minor bleeding of the operated area is acceptable in the first few hours after the intervention, but heavy bleeding may indicate injury to a large vessel or even a blood clotting pathology. Therefore, before surgery, a laboratory blood test is required to identify possible pathologies and take them into account when planning surgical intervention.
Why the design may not take root
This can happen for several reasons, related both to the course of the operation itself and to the actions of the patient in the postoperative period.
Medical error
Due to his incompetence or carelessness, an implantologist may make the following mistakes:
- choose the wrong model - the titanium root may be significantly longer or thicker than the jawbone;
- violate sterility conditions;
- incorrect installation of the implant;
- when drilling a hole for the rod, overheat the tissue;
- do not fully study information about the patient’s health status and possible contraindications.
Poor quality implant
Large dental clinics, through dealer networks, work with systems that are directly supplied from manufacturers. This eliminates the possibility of receiving a fake. In dentistry that work through intermediaries, it is risky to agree to an operation, as there is a risk of installing low-quality analogues. Therefore, you need to take the choice of a clinic and a doctor seriously, be interested in warranty conditions, survival statistics, and other important points.
Failure to comply with operating and maintenance rules
Even if the doctor performs the operation correctly, observing all the norms, problems with implant healing may arise due to the patient’s fault. Among its possible errors:
- providing the doctor with incomplete information about your well-being and health status. Even minor facts must be stated;
- excessive load on the implant during the healing period;
- failure to follow the rules of oral hygiene - even artificial teeth require careful care;
- hypothermia or overheating in the first days after surgery (visiting a sauna, diving into ice water);
- undisciplined use of medications prescribed by a doctor.
Deterioration of health
Rejection may occur several years after implantation. In addition to mechanical damage, the cause may be the development or exacerbation of:
- cardiovascular diseases;
- diabetes;
- AIDS;
- tuberculosis;
- oncological diseases.
The risk of rejection increases significantly if the patient smokes . Nicotine and tar disrupt the nutrition of mucosal cells, which has a negative effect on the condition of the tissues around the installed rod.
For what reasons can there be loss?
Dentists-implantologists, based on their clinical experience and colleagues, have identified situations and time periods that indicate the causes of tooth implant loss.
Who may be responsible for the fact that a dental implant pin or part of it falls out:
- the fault of the manufacturer of a low-quality implantation system. The product is made without proper cleaning and contains inappropriate impurities, which inhibits osseointegration;
- medical error during surgery;
- the orthopedic structure (crown, prosthesis) was selected and manufactured in violation of the omissions of the technician or orthopedist;
- the patient did not follow the doctor’s recommendations;
- allergic reaction to the material;
- independent circumstances: injury, sudden deterioration in health, emergence of a serious illness.
Let's take a closer look at some of the factors why implants fall out.
Let's start with the fact that if an implant falls out a year or several years after implantation, responsibility for this most likely lies with the patient or unplanned circumstances. It is extremely difficult, almost impossible, to prove that the manufacturer or doctor is to blame. Since, if something did not go according to the planned treatment protocol, all the signs indicating whether a dental implant might fall out or complications would be visible in the first month.
After a long period of time
The reasons for implant loss may be the following:
- mechanical trauma, a blow that damages the jaw bone in the place where the titanium root is installed;
- failure to comply with hygiene rules;
- refusal of annual dental examinations.
If the crown falls off the implant, then you should think about the load on the implant and the method of fixation. There may have been errors in the manufacture of the structure in the dental laboratory. The denture can also rub the gum, causing it to become inflamed right at the point of contact with the titanium pin.
Doctor's actions
resulting in implant loss:
- not fully planned treatment at the stage of collecting an anamnesis, the doctor did not familiarize himself with the patient’s diseases, which are a contraindication to implantation;
- the condition of bone tissue is underestimated;
- the selected location for installing the pin is incorrect;
- errors during surgery: poorly prepared bed, incorrectly selected implant, deviation from the protocol.
Common reasons
Why do dental implants fall out?
- low-quality implants;
- allergy to titanium alloy (extremely rare, sensitivity to impurities in the composition is possible);
- diseases preventing osseointegration: insulin dependence, immune diseases. The body does not accept a foreign body;
- non-compliance with recommendations after implantation;
- violation of the installation of the implantation system, preoperative studies, medical error;
- smoking affects the circulatory system as badly as it does the lungs, spasms occur in blood vessels, tissues are poorly saturated with oxygen, including tissues near the implant;
- independent and unforeseen circumstances: injuries, diseases after implantation.
How is inflammation treated?
If signs of inflammation appear, you should immediately consult a doctor . He will conduct an examination and order an x-ray. If necessary, temporarily unscrew the implant plug and clean its outer surface.
Signs of advanced peri-implantitis are eliminated by removing the structure, since an advanced inflammatory process will lead to the spread of infection. At the initial stage, surgical sanitation of the focus of gingival inflammation is carried out:
- They make an incision.
- Granulation tissue is removed.
- The surface of the titanium root is cleaned with a Prohy-Jet apparatus or special curettes.
- Rinse the pocket.
- After the operation is completed, the patient is prescribed antibiotics and antiseptic rinses.
The conservative phase of treatment includes procedures:
- Professional oral hygiene.
- Irrigation with ozonated solution.
- Laser therapy.
- Oral applications and baths are prescribed.
What we do to speed up the survival of dental implants and prevent unpleasant consequences
Our clinics have the latest diagnostic equipment, so the doctor will not miss an alarming symptom and will prescribe treatment before implantation. During preparation for surgery, if necessary, doctors of related specialties - periodontists, therapists - are invited for consultation.
When dental implants have already been installed, rehabilitation takes place under the supervision of the attending physician, who will pay attention to oddities even when you have not yet discovered them. But when using our equipment and dental implants from world-famous companies, such problems practically do not happen. Personal customer service will help you not to get confused: there is always someone to turn to and ask an exciting question. Our patients are never left alone with a problem.
How much does it cost on average in Moscow?
Treatment of complications
| Name of service | Cost, rub. |
| Periodontal applications in the area of 1 tooth | 370 |
| Application of a protective periodontal bandage | 400 |
| Laser therapy of the gum mucosa | 490 |
| Implant removal | 6900 |
| Implantation of osteoconductive material in the area of 1 tooth | 10900 |
| Implantation of a protective membrane (1 tooth) | 12900 |
Gum plastic surgery
| Name of service | Cost, rub. |
| Plastic surgery of marginal gums | 1200 |
| Gingivoplasty (1 tooth) | 1500 |
| Plastic surgery of marginal gums (segment) | 3500 |
| Plasty of gingival margin recession | 3500 |
| Flap surgery in the area of one tooth | 3500 |
| Smile line plastic surgery | 4000 |
| Gingivoplasty (1 tooth) using laser | 4000 |
| Gingivoplasty (segment) | 4500 |
| Flap surgery (three teeth) | 7000 |
| Gingivoplasty (segment) using laser | 10000 |
| Flap surgery (segment) | 10000 |
| Flap surgery (whole mouth) | 30000 |
Associated symptoms when the implant loses stability
Early implant rejection, that is, the absence of its fusion with bone tissue, can be painless and unnoticeable. Sometimes, when the rod is clearly mobile, the patient tries to get it out himself. But more often this is done by a dentist at an appointment during a follow-up examination. After this, the situation is analyzed and a re-installation is scheduled, which can be done free of charge.
If not in the first months, but much later, a tooth implant falls out, or rather its fixation in the bone weakens, this does not go unnoticed. In most cases, even before the rod loses stability, the patient notices that the gums have turned red or bluish, swollen, and pain or discomfort has appeared. If you do not consult a dentist at this time, the mobility of the implant will soon become noticeable and more pronounced symptoms of trouble will appear:
- increased pain, especially when chewing and pressing on the gums;
- the appearance of ichor, blood, pus from under the gingival margin in the area of the installed implant;
- change in the appearance of the gingival cuff that surrounds the crown;
- the appearance of bad breath;
- increase in body temperature.
It is important to quickly see a specialist at the first changes in the tissues surrounding the implant.
What to do if a tooth implant falls out
When calling the dentist with the question “a tooth implant has fallen out - what to do,” patients often mean a crown that has fallen off, a gum former or abutment that has become twisted. Some problems can be solved quickly and easily. Others may require long-term and extensive treatment:
- Screw-retained crowns often unscrew and become detached. The use of a cement composition makes the fastening stronger and allows you to preserve the same prosthesis.
- If a crown falls out due to an incorrectly selected prosthesis, it involves the production of a new artificial tooth and its installation on an existing implant.
- A common situation is that the gum former falls out. The doctor reinstalls the old one or exchanges it for a new one. The task is ordinary and does not affect the process of osseointegration and the implant itself.
What to do if a tooth implant pin falls out? Loss of an implant most often occurs due to inflammation - this is the last stage of peri-implantitis, when it is no longer possible to save the artificial root. The initial stage of tissue inflammation (mucositis) and even the first symptoms of peri-implantitis give a favorable prognosis with a high probability of saving the rejected implant.
How to protect yourself from implant loss
You can reduce the risk of implant failure by:
- Choosing the right dental clinic and doctor. Every little detail matters - modern equipment and tools, the availability of different brands of implants, the experience of a dentist-implantologist, knowledge and adherence to the intricacies of surgical implantation protocols, as well as taking out insurance against unsuccessful implantation. A rating of doctors in the required specialty or an independent assessment of metropolitan clinics will help with this.
- Consent to install implants from trusted manufacturers. Low-quality raw materials and pins from unknown companies greatly increase the risk of subsequent implant failure.
- Carrying out mandatory examination and sanitation of the oral cavity. It is important to exclude all contraindications for installation.
- Compliance with doctor's requirements. It is necessary to maintain oral hygiene, take medications prescribed by a doctor, and balance the menu to avoid overload—destruction, chipping, or rejection of implants.
- Give up bad habits - smoking and alcohol have a negative effect on osseointegration and have a bad effect on healing.
Implantation is a serious dental intervention, so it is extremely important to contact experienced dentists with good reviews and listen to their advice and recommendations - including when choosing an implant manufacturer. Then the result of the operation will be excellent, the risk of rejection and loss of the implant is minimal.
Solution
If the neck or root of a tooth located next to the implant is exposed, gum plastic surgery may be required. Flap operations are common in dental surgery. To cover exposed areas, soft tissue flaps taken from the hard palate are used. This is a fairly simple operation, the contraindications for which may include:
- allergy to anesthetics,
- malignant tumors of the jaw,
- poor blood clotting,
- uncompensated diabetes mellitus.