Neuritis
is an inflammation of the peripheral nerve trunk.
The peripheral nervous system refers to the nerve structures outside the brain and spinal cord (which are in turn called the central nervous system). Excitation (signal) is transmitted along the nerves, allowing the central nervous system to receive information about the state of all organs and systems of our body and control muscle contractions. The tissues of various organs are penetrated by nerve endings, which are connected to the brain, and in most cases to the spinal cord using bundles of nerve fibers enclosed in a sheath of connective tissue. Such bundles are called nerves, and large nerves are called nerve trunks.
With neuritis, nervous tissue is involved in the inflammatory process. This leads to the fact that the signal in some part of the nerve passes worse or does not pass at all. Accordingly, the sensitivity of any area may be lost and the mobility of the muscles innervated by the affected nerve may decrease.
Types of neuritis
A distinction is made between local neuritis and polyneuritis.
Local neuritis
is an inflammation of any one nerve (facial, auditory, oculomotor, glossopharyngeal, radial, sciatic, peroneal, femoral, etc.).
Polyneuritis
is multiple inflammation of the nerves. If the effect of the factor that caused the inflammation is local, only one nerve is affected. Polyneuritis develops under the influence of a systemic factor, which, as a rule, leads to degeneration of the nerve sheath and nerve fibers.
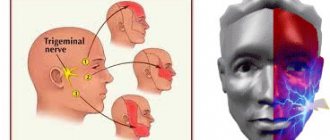
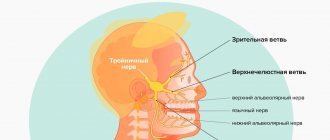
Trigeminal neuralgia - symptoms and treatment
There are two types of pain due to trigeminal neuralgia:
- constant, dull, periodically intensifying pain without wide irradiation, arising in the area of distribution of one or another branch of the nerve and not accompanied by pronounced autonomic reactions;
- pain of a paroxysmal nature, lasting from several minutes to several hours.[4][5]
The intensity of the attacks varies: from mild but frequent, lasting a few seconds, to strong and unbearable, lasting for minutes and causing severe suffering.
Attacks often occur spontaneously, without any irritants, or as a result of hard and cold food getting into the mouth, touching, drafts, hypothermia under air conditioning, jaw movements, etc.
The attack usually begins with pain in one branch of the nerve - the site of the primary lesion, then the pain spreads to other branches, often radiating to the back of the head, to the ear nerves, to the neck and even to the area of the thoracic nerves.
Severe attacks are usually accompanied by autonomic reflex reactions: redness of the face, lacrimation, runny nose, drooling, sometimes swelling of the cheeks, eyelids, and slight swelling of half the nose.
The patient's suffering is manifested by general anxiety, rubbing the painful area with his hand, putting pressure on this area, and smacking his lips. This layering of new stimuli obviously accelerates the moment of the onset of an inhibitory state in the center of pain perception, which usually gives way to an attack.
As motor manifestations in connection with a painful attack, tic-like muscle twitching or spasmodic contractions occur. The maximum twitching or contraction of the muscles corresponds mainly to the zones from which the pain begins, i.e., to the sites of primary damage.
With long-term disease, graying of the scalp hair on the affected side is sometimes observed.
Sometimes paroxysmal neuralgia is accompanied by a rash of herpes zoster (herpes zoster), located according to the primary lesions of certain branches, sometimes affecting the corneal mucosa.
Periods of exacerbations may alternate with periods of remission, which last for months, sometimes years.
Outside of an attack, usually no disorders are observed: no pain points, no objective sensitivity disorders. Sometimes you can notice a decrease in pain sensitivity, mainly in the area of the branch that was the site of the primary lesion. Less commonly, decreased sensitivity is found in the area of all branches of the trigeminal nerve. In some cases, outside of attacks, patients experience mild dull pain. Pain occurs at any time, but more often during sleep.[6][7]
Causes of neuritis
Local neuritis is caused by:
- local infection;
- local hypothermia;
- injury. Often neuritis develops after a nerve injury;
- compression of the nerve. Thus, neuritis of the axillary nerve can develop due to prolonged use of a crutch, neuritis of the peroneal nerve - due to working in an uncomfortable position, etc.;
- arthritis (in this case the nerve of the joint may become inflamed);
- tumor (if the tumor compresses the nerve).
Multiple neuritis (polyneuritis) can be caused by such reasons as:
- infectious diseases, including measles, herpes, influenza, malaria, diphtheria and some others;
- intoxication. Poisoning with arsenic, lead, mercury, carbon monoxide, phosphorus, bismuth and other highly toxic substances can lead to the development of various types of neuritis. The most common cause of multiple neuritis is alcohol poisoning;
- systemic diseases (diabetes mellitus, rheumatism, gout);
- avitaminosis;
- vascular disorders;
- as well as some other reasons.
Causes of the inflammatory process
Pathology appears after bacterial and viral infections or under the influence of external factors and internal processes in the body. The most common reasons are:
- consequences of ARVI, sore throat, bronchitis, influenza;
- previous injuries;
- pathological changes in blood vessels;
- poisoning: alcohol, toxic substances;
- diseases of the endocrine glands: thyrotoxic goiter, diabetes mellitus.
The disease also occurs due to compression of the nerve trunk. The reason may be the constant adoption of an uncomfortable posture. Thus, pianists and cellists often suffer from neuritis of the median nerve of the hand. Treatment will help avoid complete loss of sensitivity in the fingers or hand, and atrophy of muscle tissue.
Symptoms of neuritis
The main symptoms of neuritis are:
Pain along the nerve
The most common symptom of neuritis is pain along the affected nerve. The pain, as a rule, is dull in nature and intensifies in the cold, with physical activity or uncomfortable body position.
Sensory impairment
Sensory loss in the area of the affected nerve is common. It can manifest itself in the form of numbness, tingling, or “pins and needles.”
Decreased muscle activity
There is a partial decrease in muscle strength (paresis), a decrease or loss of tendon reflexes, and in some cases, muscle paralysis (complete cessation of muscle activity).
Vegetative and trophic disorders
With neuritis, there may be such vegetative and trophic disorders as depigmentation of the skin, the acquisition of a bluish tint, local hair loss, increased sweating and dry skin, swelling.
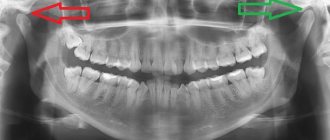
Diagnosis of neuritis
The success of treating this disease depends on many factors, and important here are the age of the patient and the stage at which the disease was detected. That is why early detection of pathology plays such a significant role.
Since the symptoms of neuritis are in many ways similar to the clinical manifestations of cerebrovascular accidents, multiple sclerosis and brain tumors, a careful differential diagnosis is required. It must be carried out by a qualified neurologist.
The doctor receives valuable data from a survey and physical examination of the patient, checking reflexes, muscle strength and other parameters. If necessary, the patient may be recommended to consult with specialists.
To clarify the diagnosis, the following studies may be prescribed:
- blood tests (clinical and biochemical),
- general urine analysis;
- radiography;
- MRI (magnetic resonance imaging);
- electroneuromyography (ENMG);
- CT (computed tomography).
Treatment methods for neuritis
Neuritis must be treated. At the first signs of the disease, you should consult a neurologist. If treatment for neuritis is not started on time, the risk of developing paresis and muscle paralysis increases.
Treatment of neuritis is aimed, first of all, at eliminating the cause that caused it. If neuritis is of infectious origin, antibacterial therapy or antiviral drugs are used. If neuritis is of toxic origin, it is important to remove toxins from the body.
Drug treatment
In addition to antibacterial or antiviral drugs, the course of treatment for neuritis usually includes:
- B vitamins
- drugs that improve blood microcirculation
- drugs that increase the conductivity of nerve fibers
Massage
Massage of the muscles innervated by the affected nerve is recommended. Massage can be combined with heat therapy (infrared sauna).
More information about the treatment method
Physiotherapy
For neuritis, physical therapy methods such as electrophoresis, diadynamic therapy, SMT therapy, ultrasound therapy, magnetic therapy, and laser therapy can be used.
More information about the treatment method
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Treatment of neuralgia
Almost all types of neuralgia can be successfully treated in the neurology department of the Bone Clinic. The nature of the therapeutic effect is determined individually, depending on the type of neuralgia and its cause.
Among the main methods of treating neuralgia at the Bone Clinic are various methods of physiotherapy: interference currents, ultrasound therapy, echothermotherapy and others, as well as methods of sanatorium treatment (mud therapy). Therapy is carried out using intelligent equipment, which greatly improves the quality and convenience of treatment for our patients.
Doctors at the Bone Clinic relieve inflammation and swelling of the nerve, eliminate pinched nerves and relieve muscle spasms. As a result of the treatment course, immunity increases and blood supply to nerve fibers improves.
Treatment
The choice of therapeutic tactics is determined by the nature of the disease, the intensity of symptoms, the presence of concomitant disorders, as well as the characteristics of the patient’s body.
The First Medical Clinic implements an integrated approach to the treatment of neuropathies, neuritis and neuralgia using unique, highly effective modern methods, such as:
- therapeutic blockades;
- autoplasmotherapy;
- reconstruction of the spine (intervertebral discs);
- photodynamic therapy;
- transcutaneous electrical stimulation;
- ozone therapy and others.
For emergency relief from acute pain (this is of particular importance for neuralgia), they resort to blockades of nerves or their roots. The method is based on the administration of painkillers directly to the affected area. The high concentration of the active substance at the site of pathology allows you to almost instantly block the transmission of the pain impulse and ensure pain relief.
Treatment of neurology
High therapeutic effectiveness in treating neurological diseases is demonstrated by the method of plasma therapy - the use of platelet autoplasma. A small volume of the patient's venous blood is centrifuged. The result is plasma with a high content of platelets, sources of bioactive substances such as growth factors. Plasma injection leads to the release of these growth factors at the site of pathology, where they activate tissue regeneration processes. As a result, swelling and inflammation are relieved, pain is reduced, and pathological changes are eliminated.
If nerve damage is caused by spinal pathologies, reconstruction of the intervertebral disc and photodynamic therapy can help reduce the symptoms of the disease, as well as eliminate the cause of the disease. During reconstruction, the medicine is injected directly into the intervertebral disc, which stimulates its self-healing processes. In photodynamic therapy, a photosensitizing drug is applied to the skin in the area of the affected nerve and the area is exposed to laser radiation. As a result, the source of pathology is destroyed by high-energy oxygen.
With transcutaneous electrical stimulation, short pulses of electric current are applied to the area where the diseased nerve passes.
The required amount of therapeutic assistance can only be determined by a specialist after diagnostic procedures. If you have signs of nerve damage, we recommend that you contact the First Medical Clinic in a timely manner.
You can make an appointment for a consultation and appointment by phone
Causes of neuralgia
Unlike neuritis, which is an inflammatory disease, neuralgia is not. Neuritis develops against the background of a virus and infection. Neuralgia occurs due to mechanical effects on the trigeminal nerve, provoked by various factors.
- Head injuries with displacement of the skull bones.
- Tumors of various etiologies, which, as they grow, compress the trigeminal nerve.
- Bite defects and other anomalies of the dentofacial area.
- Diseases of blood vessels located in close proximity to the trigeminal nerve.
- Chronic sinusitis and otitis.
- Medical error during tooth extraction.
- Neuralgia can be triggered by infections, including periodontitis, stomatitis, herpes, and syphilis.
Hypothermia does not cause neuralgia, but makes treatment difficult. Neurosis, metabolic disorders, diabetes mellitus and other chronic pathologies have a negative effect on therapy.
Read also
Consequences of traumatic injuries to the skull, spine, brain and spinal cord
Traumatic brain injuries, or traumatic brain injuries, are damage to the brain that impair brain function.
Brain injuries are divided into two large groups - closed… Read more
Chiari malformation
What is Chiari Malformation? Chiari malformation (formerly Arnold-Chiari malformation) is a congenital defect of brain development that involves the dislocation of the cerebellar tonsils into the spinal canal through the large…
More details
Rehabilitation
Restoration of the body after diseases of the central and peripheral nervous system, operations on the brain and spinal cord, conditions after removal of the mammary gland due to a tumor, consequences...
More details
Atherosclerosis
Atherosclerosis is a vascular disease that is caused by a decrease in the elasticity of the vascular wall, the deposition of cholesterol on the inner surface and, as a result, the appearance of atherosclerotic plaques. Atherosclerosis…
More details
Intracranial hypertension
Intracranial hypertension is a condition (syndrome) associated with increased cerebrospinal fluid (CSF) pressure inside the skull. The main symptoms of increased intracranial pressure are...
More details