Trigeminal neuropathy (trigeminal neuralgia) is a chronic pain syndrome that involves the trigeminal (5th cranial nerve). Trigeminal neuropathy is a type of neuropathic pain (pain associated with injury or damage to a nerve). The usual or “classic” form of the disease (the so-called “Type 1”) is characterized by attacks of intense pain in the form of a burning sensation or shock that last from a few seconds to two minutes. These attacks can occur in group episodes lasting up to two hours. The “atypical” form of the disease (the so-called “Type 2”) is characterized by constant aching, burning, stabbing pain of somewhat less intensity than with type 1. Both forms of pain can occur in the same person, sometimes at the same time. The intensity of pain can lead to disability, both physical and mental.
The trigeminal nerve is one of 12 paired nerves that exit the brain. The nerve has three branches that carry sensory sensations from the upper, middle and lower parts of the face, as well as the mouth, to the brain. The ophthalmic or superior ramus provides sensory sensation to most of the face, forehead, and front of the head. The maxillary or middle branch provides sensation to the cheek, upper jaw, upper lip, teeth and gums, and side of the nose. The mandibular or inferior branch innervates the lower jaw, teeth and gums, and lower lip. With trigeminal neuropathy, more than one branch may be affected. In rare cases, there may be manifestations of neuropathy on both sides at different times. Even less common is bilateral involvement.
Trigeminal neuropathy occurs most often in people over 50 years of age, although the condition can occur at any age, including in infants. The possibility of developing trigeminal neuropathy increases slightly with multiple sclerosis when it occurs in young people. The rate of new cases is approximately 12 per 100,000 people per year; the disease is more common in women than in men.
How does neuritis of the facial nerve appear?
Neuritis of the facial nerve can begin with mild pain in the ear area. Simultaneously with the onset of pain or after a couple of days, the facial muscles partially or completely lose mobility. The patient's face becomes distorted, the affected part freezes in the mask.
With timely treatment, the patient has a great chance of recovery - in 75% of cases the disease goes away completely. If facial paralysis does not resolve within three months, the patient's chances of making a full recovery are greatly reduced.
In order for facial neuritis to pass without consequences, you need to consult a doctor in the first hours after the onset of symptoms.
Causes
Trigeminal neuropathy can be associated with a variety of conditions. Neuropathy can be caused by blood vessel compression on the trigeminal nerve as it exits the brainstem. This compression causes the protective covering around the nerve (myelin sheath) to wear or become damaged. Symptoms of trigeminal neuropathy can also occur in patients with multiple sclerosis, a disease that damages the myelin sheath of the trigeminal nerve. Rarely, symptoms of neuropathy may be due to nerve compression by a tumor or arteriovenous malformation. Damage to the trigeminal nerve (possibly as a result of oral surgery, stroke, or facial trauma) can also lead to neuropathic pain.
Symptoms
The following symptoms of inflammation of the facial nerve are distinguished:
- partial or complete impairment of facial muscle movements;
- the corner of the mouth lowers, the nasolabial fold on one side is smoothed out;
- the face becomes asymmetrical;
- the eyelid does not close completely;
- the eyeball protrudes and turns upward;
- pain in the ear, taste disorder;
- watery or dry eyes;
- hearing loss or sensitivity to loud sounds;
- the patient cannot whistle or stretch out his lips with a straw.
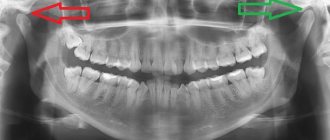
How is the disease diagnosed?
The diagnosis of a neurological disorder is carried out by a specialist - a neurologist. To exclude dental pathologies, an initial consultation and examination by a dentist will be required. The primary examination is carried out by palpation. The doctor determines the pain of the main points located on the tongue and in the sublingual area. Unpleasant sensations occur when pressure is applied to the skin located in the lower part of the jaw on the side in which the disorder develops. In this case, there is no change in taste sensations. Degenerative changes in the mucosa, ulcerative lesions, and deformation of the lingual papillae can be visually determined.
To clarify the diagnostic assumption, the described nerve processes are blocked. Common anesthetics are used for this: lidocaine, novocaine. Confirmation of the suspected disease occurs if the pain disappears as a result of the administration of local anesthesia. At the same time, the neurologist tries to exclude anomalies with similar symptoms: tumors, cystic processes, damage to the trigeminal nerve, etc.
Causes of inflammation
Primary neuritis of the facial nerve occurs due to:
- hypothermia of the face, cold, wind, drafts;
- insufficient blood supply (ischemia) to the nerve.
Secondary neuritis of the facial nerve is caused by the following reasons:
- inflammatory diseases of the ear: otitis media, eustachitis, mastoiditis;
- infections: mumps virus, measles, herpes;
- traumatic brain injuries;
- vascular disorders - for example, atherosclerosis of the vertebral arteries;
- brain tumors;
- anesthesia of the inferior alveolar nerve by the dentist.
Other factors that provoke inflammation include:
- traveling on a bus or minibus next to an open window;
- long work under air conditioning;
- metabolic disorders in the body;
- endocrine diseases - for example, diabetes;
- hypertension, intoxication of the body;
- nervous stress, emotional instability.
Description of the pathological condition
The disease of the nerve branches located in the tongue and lower jaw is accompanied by pain and salivation disorders. Nerve clusters (nodes) located in this area belong to the peripheral parts of the NS. Despite the fact that neurologists anatomically separate the sublingual and submandibular nodes, degenerative processes occur in them simultaneously. This is due to the fact that numerous neural connections are distributed between the channels. This allows the pathology to be classified as one disease.
Complications of the disease
Neuritis of the facial nerve can lead to contracture of the facial muscles. It appears 4-6 weeks after the onset of the disease due to incomplete restoration of the motor functions of the facial muscles. Contracture is a contraction of the muscles of the affected half of the face. At the same time, it seems that it is not the diseased part of the face that is paralyzed, but the healthy one.
To avoid complications of inflammation of the facial nerve, you need to consult a doctor in time. For prevention, we recommend doing facial exercises. You will find examples of exercises at the end of the article.
Treatment
Treatment options include medication, surgery, and multimodal treatment.
Medications
Anticonvulsants, used to block nerve stimulation, are generally effective in treating type 1 NTN but are often less effective in treating type 2 neuropathy. These drugs include carbamazepine, oxcarbazepine, topiramate, gabapentin, pregabalin, clonazepam, phenytoin, lamotrigine, and valproic acid.
Tricyclic antidepressants such as amitriptyline or nortriptyline may also be used to treat pain. Analgesics and opioids are usually not effective for treating acute, recurrent pain caused by T1, although some patients with T2 respond to opioids. Ultimately, if treatment does not relieve pain or results in significant side effects such as cognitive impairment, memory loss, excessive fatigue, bone marrow suppression, or allergies, then surgery may be recommended. Because trigeminal neuropathy is most often a progressive disease that becomes drug-resistant over time, patients often seek surgical treatment.
Surgery
Several neurosurgical techniques are generally used to treat NTN, depending on the nature of the pain, the wishes of the individual, physical health, blood pressure and the presence of previous operations. Some procedures are performed on an outpatient basis, while others, which are performed under general anesthesia, are performed in a hospital setting. After these surgical procedures, there may be some reduction in the face and it is not uncommon for NTN to recur, even if the procedure was initially successful. Several procedures will be used. These are like:
- Rhizotomy is a procedure in which nerve fibers are damaged to block pain. Rhizotomy to treat NTN always causes some degree of sensory loss and facial numbness.
- Glycerin injections are an outpatient procedure that is performed after light anesthesia. This form of rhizotomy usually results in pain relief within 1-2 years. However, this procedure can be repeated several times.
- Radiofrequency thermal ablation is most often performed in an outpatient setting.
- Stereotactic radiosurgery (using Gamma Knife or CyberKnife) uses CT scanning to deliver highly focused radiotherapy to the area where the trigeminal nerve exits the brain stem. This causes slow nerve damage, which disrupts the transmission of sensory signals to the brain. Patients who have had this procedure can go into remission for up to three years.
- Microvascular decompression is the most invasive of all surgeries for treating NTN, but it also has the best long-term results and the lowest likelihood of pain recurrence. About half of people who have this procedure will experience periodic pain for 12 to 15 years.
- A neurectomy, which involves a partial incision of the nerve, can be performed at the nerve's entry point into the brainstem while attempting microvascular decompression. A neurectomy can also be performed by cutting the superficial branches of the trigeminal nerve on the face.
Surgical management of T2 is usually more problematic than for T1, especially where vascular compression is not detected on neuroimaging.
Additional treatments
Some patients benefit from combining medications with other treatment methods. These methods have varying degrees of effectiveness. Some patients find that gentle exercise, yoga, creative visualization, aromatherapy, or meditation can help. Other treatment options include acupuncture, chiropractic care, biofeedback, vitamin therapy, and nutritional therapy. Some patients note a certain effect from the use of botulinum toxin.
Treatment methods
It is important to consult a doctor immediately after the first characteristic symptoms appear. Timely treatment increases the chances of a full recovery. Neuralgia requires long-term therapy, the tactics of which are determined depending on the clinical condition of the patient and the course of the disease.
Conservative therapy
The patient is prescribed:
- taking non-steroidal anti-inflammatory analgesics;
- antiepileptic drugs;
- neuroleptics;
- muscle relaxants;
- a complex of vitamins and microelements to strengthen the immune system.
If oral administration is ineffective, the patient is prescribed injections of blockades under the tongue. Anesthetics are used for local treatment of the oral cavity. To increase efficiency, physiotherapeutic procedures (for example, exposure to diadynamic and sinusoidal currents, galvanization) are prescribed in combination with drug treatment.
Surgery
The operation is performed to release the compressed nerve. For this purpose, the method of microvascular decompression is used in the area where the nerve process exits the brain. If indicated, it may be necessary to dissect the hypoglossal ligament and shorten the styloid process.
The manipulation is carried out using endoscopic microsurgical equipment, which minimizes the impact on healthy tissue and prevents negative consequences.
Negative consequences may occur after an incorrectly performed intervention (for example, re-infection or injury to the affected area). Timely treatment and compliance with the recommendations of the attending physician increases the chances of a favorable outcome.
Causes and symptoms
As a rule, we are talking about inflammation of the temporomandibular joint (TMJ).
This can happen either as a result of mechanical trauma or an infection that has entered the body. In addition, inflammation can be acute and chronic, serous, aseptic, purulent and deforming. This disease often occurs in patients with rheumatism. Older people are especially susceptible to a type of this disease called osteoarthritis.
The main causes of TMJ inflammation:
- injuries to the bones of the facial skeleton;
- problems in the development of jaw bone tissue;
- lack of chewing teeth;
- incorrect orthopedic treatment;
- constant chewing on one side.
In patients, diseases of the jaw joint manifest themselves as follows:
- a crunching or clicking sound is heard when opening the mouth;
- it hurts to chew and yawn;
- the bite is deformed;
- headache, ringing in the ears.
Moreover, in the early stages, a person may not even experience pain, but only notice various oddities such as a jaw crunch or feeling unwell. And in some situations, on the contrary, everything is so neglected that it is impossible to even open your mouth. Here we need to take action immediately.