- Location and functions of the facial nerve
- Causes
- Symptoms
- Diagnostics
- Treatment
- Otogenic neuritis of the facial nerve
- Folk remedies
- Possible complications
- Prevention
Pathology of the facial nerve is registered annually in 2–3 people out of 10 thousand people. It occurs due to various reasons, the nature of which largely determines the treatment of facial neuritis. Taking into account the anatomical connection of this formation and the ENT organs, with neuritis of the facial nerve the patient needs to consult not only a neurologist, but also an ENT doctor.
Facial nerve, anatomy
The facial nerve, nervus facialis , the 7th pair of cranial (cranial) nerves is a motor nerve.
The facial nerve innervates the facial muscles of the face (except for the musculus levator palpebre superioris), as well as the muscles of the auricle and skull, the posterior belly of the digastric muscle (musculus digastricus), the stylohyoid muscle (musculus stylohyoideus), the stapedius muscle (musculus stapedius), the subcutaneous muscle of the neck (musculus platysma).
The nucleus of the facial nerve is located on the border of the lower part of the pons with the medulla oblongata, outward and anterior to the nucleus of the abducens nerve. The axons of the cells of this nucleus rise in the dorsomedial direction to the bottom of the rhomboid fossa, then loop around the nucleus of the abducens nerve located here, forming the internal knee of the facial nerve in the area of the facial tubercle . The root of the facial nerve exits the base of the brain in the cerebellopontine angle between the pons and the medulla oblongata, lateral to the olive, then, together with its companions and the cochlear part of the 8th pair of cranial nerves, enters the internal auditory foramen (miatus acusticus internus), then the nerve and its companions enter facial canal (canalis facialis) of the pyramid of the temporal bone (fallopian canal). The canal initially has a horizontal direction (parallel to the apex of the temporal bone pyramid), then bends vertically. It then opens at the base of the skull with a stylomastoid opening (foramen stylomastoideum). The bend of the facial nerve in its canal is called the “external genu of the facial nerve.” In this place there is the knee ganglion (ganglium geniculi), where the cells of the first taste sensitivity neuron for the intermediate nerve are located. After emerging from the stylomastoid foramen, the facial nerve penetrates the parotid gland and divides into many terminal branches to innervate the corresponding muscles, forming the pes anserinus. The companions of the facial nerve in the canal are the parasympathetic lacrimal fibers - the greater petrosal nerve (nervus petrosus major) and the intermediate nerve (nervus intermedius), the 13th pair of cranial nerves, the Wriesberg nerve.
Parasympathetic lacrimal fibers originate from the secretory nucleus, which is located near the nucleus of the facial nerve. Together with the facial nerve, they enter the facial canal, then are the first to leave it as part of the nervus retrosus major, which innervates the lacrimal gland. Loss of function of the greater petrosal nerve is accompanied by the following symptoms - dry eye, eye irritation, lacrimation.
The intermediate nerve is mixed, consists of efferent parasympathetic salivary fibers for the sublingual and submandibular salivary glands, afferent taste fibers for the anterior 2/3 of the tongue. Salivatory fibers originate from the superior salivatory nucleus (nucleus salivatorius superior), leave the brain in the cerebellopontine angle and enter the facial canal next to the facial nerve, then leave the canal in its descending part as part of the chorda tympani (chorda tympani). Sensitive taste fibers begin from the cells of the knee ganglion, the dendrites of which go in the facial canal along with the facial nerve, then depart from it in the descending part of the canal, participate together with salivary fibers in the formation of the tympanic chord, then enter the system of the 3rd branches of the trigeminal nerve (nervus lingualis ) and reach the taste buds of the anterior 2/3 of the tongue. The axons of the cells of the knee bridle leave the pyramid of the temporal bone through the internal auditory foramen, pass through the cerebellopontine angle and end in the taste nucleus of the solitary tract (nucleus tractussoliterii), common with the glossopharyngeal nerve, located in the medulla oblongata. Damage to the intermediate nerve and the chorda tympani, which is its continuation, leads to hypofunction of the sublingual and submandibular salivary glands and impaired taste in the anterior 2/3 of the tongue. Between the two companions in the facial canal, motor fibers are separated from the trunk of the facial nerve, which form the stapedius nerve (nervus stapedius). The stapedius nerve penetrates the tympanic cavity and innervates the stapedius muscle, which provides a certain degree of fixation of the stapes and tension of the tympanic membrane, which creates conditions for the best audibility. Damage to the stapedius nerve is accompanied by a symptom such as hyperacusis. Hyperacusis is an increased unpleasant perception of sounds, especially low tones.
The first to leave the facial canal is the facial nerve's companion, the greater petrosal nerve. The second branch of the facial nerve to leave the facial canal is the stapedius nerve. The third to leave the facial canal is the companion of the facial nerve - the intermediate nerve in the form of the chorda tympani.
There are features of connections between the facial nerve and the cerebral cortex - the lower third of the precentral gyrus. The upper half of the nucleus, which provides innervation to the facial muscles of the upper part of the face, has a bilateral cortical representation due to the partial supranuclear decussation of the corticonuclear fibers. Fibers to the lower half of the nucleus, from which the facial muscles below the palpebral fissure are innervated, originate from the opposite hemisphere. This point is an important criterion in making a topical diagnosis.
Medical Internet conferences
The trunk of the facial nerve from the beginning of the cervical branch from it to its exit from the stylomastoid foramen in all the adult head-neck complexes we studied lay behind the external carotid artery and the external jugular vein. Of the 9 variants of the facial nerves, we encountered the main type of branching of the nerve in 7 cases, and the scattered type only in 1 person, where both sides of the head and neck area were prepared. With the main type of branching, all facial nerves were quite long and split into 2 trunks: upper and lower, which were subsequently divided into 3 and 2 groups of branches, respectively. During the dissection process in 2 people, where the branches of the facial nerve were isolated on the right and left sides, we found differences in the number of branches, especially from the upper trunk. It branched off in one version: 2 temporal on the left and 3 on the right, 3 zygomatic on the left and 2 on the right, and 2 buccal branches. In another case: also - 2 temporal - on the left and 3 on the right, and there were 2 zygomatic and buccal branches on both sides. In cases of unpaired preparations from 3 different people, among which there were 2 right halves and 1 left half of the head-neck complex, we found: right temporal branches 1 and 2, respectively, zygomatic - 2 and 3, buccal - 2. In the case of the left half: there were 3 temporal branches, 2 zygomatic branches on the left and 1 buccal branch. From the lower trunk, in all cases of main branching, single branches departed - the marginal mandible and the cervical branch. In one case, from the unpaired complex of the left side, the division of the marginal branch into 2, 1 cm before entering the muscle, was noticeable. In the case of loose branching, all 5 branches of the “large crow's foot” were clearly visible. They were short and almost identical in diameter, quickly breaking up into secondary branches. The temporal branch was divided into 3 branches, the zygomatic branch was also divided into 3 branches, the buccal branch was divided into 5 branches, and the marginal mandible and cervical branches were also single, as in the case of the main branching. It should be noted that all angles between the branches did not exceed 14°. With the exception of one option, where the buccal-marginal angle was 20°. The magnitude of the zygomaticotemporal angle ranged from 6 to 9°. The buccal-zygomatic angle ranged from 4 to 7°. The buccal-marginal angle turned out to be the largest – 12–14°. The neck-edge angle was 5–6°. Moreover, of the named values, the smaller value corresponded to the scattered branching of the facial nerve. Among the preparations where measurements were carried out on both sides, the measurement values coincided, which suggests the symmetry of the branching of the facial nerves. Between secondary branches, the angle sizes for all types of branching were 4–5°.
During the preparation process, we discovered 2 anastomoses of the facial nerves with the branches of the trigeminal nerve and the cervical plexus. In one case, we observed an anastomosis between the buccal branch of the facial nerve and the infraorbital nerve, which is a branch of the maxillary nerve (the second branch of the trigeminal nerve). The nerve arising from the pes anserine was an isolated connecting branch, among 5 found in this individual. In another case, the cervical branch of the facial nerve and the transverse nerve of the neck, the cutaneous branch of the cervical plexus, were anastomosed. In this case, the main distribution of nerve fibers to the skin of the neck from the transverse nerve and from it a thin anastomotic branch to the cervical branch of the facial nerve were clearly defined.
Facial nerve: symptoms, lesion syndromes
When the trunk of the facial nerve, the root of the facial nerve or the nucleus of the facial nerve is damaged, paresis of the facial muscles (muscle paresis) of the same half of the face develops - prosoplegia. Facial asymmetry occurs, which is pronounced even at rest. The entire affected side is motionless and mask-like. The forehead folds and nasolabial folds are smoothed. The palpebral fissure is widened. The corner of the mouth is downturned. Due to loss of function of the circular muscle of the eye (musculus orbicularis oculi), the eye does not close. This is lagophthalmos , or hare's eye. When you try to close your eyes, the eyeball on the affected side turns upward, the iris goes under the upper eyelid - Bell's symptom. With mild paresis of the orbicularis oculi muscle, the palpebral fissure closes, but less tightly than on the healthy side, the eyelashes remain visible (eyelash symptom). When the normal function of the lacrimal gland is preserved, lagophthalmos is usually accompanied by lacrimation, which is caused by difficulty in moving tears to the lacrimal canal due to insufficient adherence of the lower eyelid to the eyeball and impaired absorption due to displacement of the opening of the canal. Also, lacrimation is facilitated by the strengthening of the tear reflex due to the constantly open eye. Inflammatory phenomena, conjunctivitis, and keratitis often develop due to irritation of the eye membranes by air flow and dust.
The asymmetry of the face increases sharply when teeth are shown. The corner of the mouth is pulled back and it is skewed towards the healthy side - this is the phenomenon of the exclamation point, it is associated with paralysis of the musculus risorius. Due to the weakness of the orbicularis oris muscle, whistling and stretching of the lips into a tube are impossible. The patient often has difficulty speaking and eating. Liquid food on the affected side spills out of the mouth, thick food gets stuck between the cheek and teeth. When frowning and wrinkling the forehead, folds do not form on the side of paralysis, it is impossible to puff out the cheeks, and there is no tension on the musculus platysma of the neck. The brow reflex, nasopalpebral reflex, corneal reflex, and conjunctival reflex are lost or weakened. If damage to the facial nerve occurs in a child of the first year of life, then the sucking reflex, proboscis reflex, and search reflex are reduced. As with any peripheral paralysis, atrophy of the facial muscles is possible. When studying electrical excitability and myography, a degeneration reaction is noted.
Peripheral paralysis of the facial muscles is sometimes accompanied by pain in the face, ear, and mastoid process. The pain is associated with the phenomenon of repercussion. Repercussion is the irradiation of excitation from the motor branches of the facial nerve to the sensory branches of the trigeminal nerve.
Prolonged peripheral paralysis can lead to the development of contracture of the affected muscles, which is manifested by a narrowing of the palpebral fissure on the affected side and a pulling of the mouth when baring teeth towards the affected affected side. Symptoms of incipient contracture are often pathological synkenesis of the facial muscles - ocular synkenesis. They are characterized by the following symptoms. The closing of the eyes is accompanied by movement of the corner of the mouth or baring of the teeth. Baring your teeth causes the eye on the affected side to close.
In pathological processes that cause irritation of the nucleus or fibers of the facial nerve, facial hemispasm is observed - this is squinting the eye and pulling the mouth and tip of the nose to the affected side with simultaneous contraction of the chin muscles and tension of the subcutaneous muscle of the neck. Signs of irritation of the facial nerve are also tics of facial muscles and Chvostek's sign.
The main nerves of the face and types of damage when injecting fillers
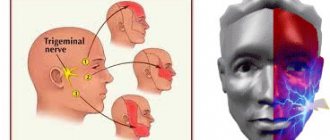
The main nerves that can be damaged during facial injection surgery are the facial and trigeminal nerves. The trigeminal nerve branches into:
- ophthalmic branch;
- maxillary branch;
- mandibular branch.
The trigeminal nerve passes through the openings of the skull and divides into independent sensory components.
Subscribe to our channel on Telegram !
The facial nerve , in contrast, has a single trunk, which passes through the stylomastoid foramen and, at the parotid gland, divides into two branches:
- cervicofacial;
- temporofacial.
The cervical and temporofacial branches are in turn divided into:
- temporal;
- zygomatic;
- buccal;
- marginal branch of the mandible;
- cervical
Nerve damage caused by dermal filler injections can be temporary, reversible, or permanent.
Damage can occur when drugs are administered using either a needle or a cannula. In addition to puncture or partial rupture of the nerve with a needle, it can be damaged as a result of :
- injection of filler directly into the nerve;
- tissue compression after filler injection;
- Too much massage after filler injections.
Nerve damage almost always results in neuropraxia , a loss of sensory and/or motor function.
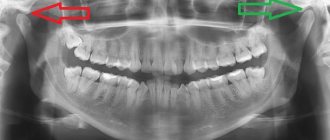
Diagnosis of the level of damage to the facial nerve
Isolated lesions of the nucleus of the facial nerve are observed quite rarely. It is manifested by total paresis of the facial muscles and occurs in the pontine form of polio.
More often, pathological foci localized in the pons are more common and lead to the involvement of the nucleus of the facial nerve, radicular fibers, and pyramidal tract in the process, which is manifested by alternating Millard-Hübler syndrome. Simultaneous damage to the nucleus of the abducens nerve is manifested by alternating Foville syndrome.
When the pathological process is localized in the cerebellopontine angle, the symptoms of damage to the facial nerve are combined with damage to its companions (the intermediate nerve and the greater petrosal nerve) and the vestibulocochlear nerve. Paralysis of facial muscles in these cases is accompanied by dry eyes - xerophthalmia, impaired taste in the anterior 2/3 of the tongue on the affected side. Xerostomia may be felt - dry mouth, but more often it does not occur due to the functioning of other salivary glands (parotid, sublingual, submandibular on the healthy side). Hyperacusis does not occur due to concomitant damage to the cochlear nerve. Hearing loss or deafness is more common. There may be signs of dysfunction of the trigeminal nerve and abducens nerve located in the immediate vicinity, as well as cerebellar disorders.
When the facial nerve is damaged in the facial canal above the origin of the greater petrosal nerve, dry eyes, taste disorders and hyperacusis develop simultaneously with paralysis of the facial muscles.
The lesion after the departure of the greater petrosal nerve is accompanied by increased lacrimation, taste disturbance, and hyperacusis.
When the facial nerve is damaged below the origin of the stapedius nerve, but above the origin of the chorda tympani, paralysis, lacrimation, and taste disturbance are observed.
Damage to the nerve in the bony canal below the origin of the chorda tympani or after exiting the stylomastoid foramen causes only paralysis with lacrimation.
When the process is localized in the area of the outer knee of the facial nerve with involvement of the knee node, Hunt's syndrome can be detected - this is paresis of the facial muscles (facial muscles), severe pain and herpetic rashes in the area of the auricle (ear).
Sometimes there are cases of bilateral damage to the facial nerve. Bilateral damage to the facial nerves is called diplegia facialis. The patient's face is mask-like, his eyes are half-open, it is impossible to form his lips into a tube or close his mouth.
Facial nerve (anatomy, physiology, symptomatology)
[Home] [To volume contents]
The facial nerve (VII), which innervates all the facial muscles of the face, plays an exceptional role in otiatry: already upon leaving the brain stem, at the bottom of the skull, it is inextricably linked with the auditory nerve (basilar meningitis, tumors , cracks of the base of the skull): along with it, it enters the internal auditory canal. In the further course of the nerve, inside the rocky bone, an even closer connection arises with the pathology of the middle ear, one of the most important and common causes of its damage. In this sense, the facial nerve constitutes a separate chapter of ear neurology.
Along the way, we will touch on the role of other cranial nerves (trigeminal, glossopharyngeal, vagus) related to the organ of hearing.
The facial nerve originates from the nucleus of the same name, which lies in the reticular formation of the Varoliev bridge; it is located posterior and outward from the superior olive (see cochlear nerve) and consists of very large polygonal cells. Nerve root - upon exiting the nucleus, it first goes inward in the direction of the rhomboid fossa, then, turning sharply, goes upward, forming the ascending part; finally, again turning outward and penetrating through the entire thickness of the medulla, it emerges on the anterolateral surface of the Varoliev bridge next to the auditory nerve. In this so-called The “brain knee” of the facial nerve lies the nucleus of the abducens nerve, which explains their often joint damage in intra-stem lesions. The nucleus of the facial nerve communicates with the cortex of the cerebral hemispheres, precisely with the lower part of the anterior central gyrus, through the corticonuclear pathway, which forms a cross just before the end of the fibers in the nucleus. Sensitive collaterals also end there, in particular from the trapezoid body (see about the auditory nerve), the trigeminal nerve, etc.
Upon exiting the brain stem, the facial nerve, together with the auditory nerve and the thin trunk n. lying between them. Wrisberg's interraedius enters the internal auditory canal. At the bottom of the latter, it separates, together with the Wriesberg nerve, from the auditory nerve, penetrates into the substance of the rocky bone and forms here - in the hiatus spurius - the so-called. geniculate ganglion (ganglion geniculum). The nerve then passes through the Fallopian canal, or facial nerve canal, and exits the temporal bone, hence the cranial cavity, through the stylomastoid foramen. On its way from the Varoliev bridge to the final branching, the facial nerve gives off a number of branches with different functional significance, which, by the way, makes it possible to more accurately localize the height of its lesion (see diagram, Fig. 24).
From the point where it exits the brainstem to the geniculate ganglion, the facial nerve does not form any branches. From the geniculate ganglion arise:
1. N. petrosus superficial major, connecting the indicated ganglion with the ganglion sphenopalatinum, the second branch of the trigeminal nerve (see Fig. 25). It contains secretory fibers coming from the trunk of the facial nerve for the lacrimal gland (via the lacrimal nerve of the first branch of the fifth pair). Therefore, damage to the facial nerve along its path from the exit from the pons to the geniculate ganglion, that is, at the base of the skull, in addition to all other symptoms, is also accompanied by a decrease in tear production on the side corresponding to the lesion.
2. An anastomosing branch to the tympanic plexus (plexus tympanicus) of the glossopharyngeal nerve, which, as we will see later, is of great importance for the sensitive innervation of the organ of hearing.
From the descending part of the nerve inside the Fallopian canal there are:
1. Nervus stapedius, motor nerve going to the muscle of the same name in the tympanic cavity; its participation causes a peculiar hearing disorder, expressed in increased sensitivity to sound stimulation (hyperacusis) and the sensation of noise.
Rice. 24. Topography of the main branches of the facial nerve. 2 - n. auricularis post.; 3 - foramen stylomastoideum; 1, 4.5, 6 and 7 - damage levels n. facialis; 8 - n. acustirus; 9 - n. facialis; 10 - ganglion geniculi. 11 - n. petrosus superf. major; 12 - stapedius; 13 - chorda tympani. ... tear-securing fibers; — — — flavor fibers. |
2. Drum string (chorda tympani), going to the tympanic cavity and through the fiss. petrotympanica - to the lingual nerve of the fifth pair. It contains centripetal and centrifugal fibers. The former carry taste fibers from the anterior two thirds of the tongue (the posterior one receives taste fibers from the glossopharyngeal nerve); through the facial nerve and geniculate ganglion they are part of n. intermedius. As mentioned, this latter passes as an isolated nerve between the roots of the facial and auditory nerves to the geniculate ganglion and can be considered as a special sensory root of the facial nerve (it also includes sensitive taste fibers from the n. petrosus superficialis major). The fibers of the chorda tympani and the Wriesberg nerve, as its central continuation, originate from the sensory cells of the geniculate ganglion; therefore, all three mentioned formations can be considered as a single whole - conductors of taste sensitivity. They also end separately from the facial nerve - in the so-called terminal nucleus. single fascicle, which is the primary center of taste.1
Naturally, if the facial nerve is damaged inside the Fallopian canal before the string leaves, its paralysis will also be accompanied by a taste disorder in the two anterior thirds of the tongue.
The centrifugal fibers of the facial nerve consist of secretory conductors for the sublingual and submandibular glands. They originate from the cells of the reticular formation near the nucleus of the facial nerve.
3. Anastomosing branch to the auricular branch of the vagus nerve. In the interval from the stylomastoid foramen to the entrance to the parotid gland, the facial nerve gives off:
1. Posterior auricular nerve (n. auricularis post), which departs from the trunk just under the opening and rises to the anterior surface of the mastoid process and is then divided into two branches: a) auricular, innervating the muscles of the auricle, and b) occipital, going to the same muscle.
2. Ramus digastricus, next to the first, innervating the posterior belly of the muscle of the same name, m. stylohyoideus, and sends an anastomosing branch to the glossopharyngeal nerve.
Paralysis of these branches has no clinical significance. Damage to the facial nerve as it exits the stylomastoid foramen—the usual location for the most common “rheumatic” paralysis—will not, therefore, be accompanied by disturbances in lacrimation, hearing, and taste.
Rice. 25. Facial, trigeminal and glossopharyngeal nerves in their relation to the middle ear (according to Schwart'zy). a - anastomosis between n. petrosus superf, major etminor; Npsma - N. petrosus superf; major; Npsmi-N; petrosus superf. minor; Nppma - N. petrosus profundus major; Nppmi - N. petrosus profundus minor, Ch - chorda tympani; C - cochlea; Fv - fenestra vestibull; Fc - fenestra cochleae (Other designations are in the figure). ——— autonomous fibers; …. sympathetic fibers; _ . _ . _ . flavor fibers; - motor and sensory fibers. |
Within the parotid gland, the facial nerve divides into superior and inferior branches, which immediately anastomose with each other to form the parotid plexus. Having penetrated the gland, the terminal branches, branching in the form of pes anserinus, go to the muscles of the face.
The superior branch of the facial nerve innervates the muscles of the auricle, the frontal and orbicularis oculi muscles (closing the eye) and the corrugator supercilii; lower branch - lanitis, orbicularis oris, all small facial muscles and platysma myoides. Thus, the facial nerve moves almost all the muscles of the face, with the exception of the levator of the eyelid (m. levatoris palpebrae sup., which opens the eye, innervated by the oculomotor nerve) and mastication (trigeminal nerve).
Peripheral paralysis of the facial nerve, in particular, of auricular origin, is characterized by the participation of both branches to the same extent; with a central lesion of the nerve (cortical-nuclear neuron), which is primarily important for differential diagnosis, only the lower branch is paralyzed, while the upper branch - therefore, the corresponding muscles - is almost or not at all involved in the paralysis. This is explained by the bilateral cortical innervation of these muscles, which is also the case for all muscles in general, acting synergistically on both halves of the body. In addition, with central paralysis, the phenomena are generally less pronounced.
But the facial nerve is not, as is commonly believed, exclusively a motor nerve: it also contains sensory fibers (general sensitivity), in addition to taste fibers from the chorda tympani, which also originate from the sensory cells of the geniculate ganglion. This explains, by the way, the fact that recent cases of peripheral paralysis of the facial nerve can sometimes be accompanied by painful sensations in the corresponding area of the face. If, in particular, the geniculate ganglion is affected, a peculiar Gunt's symptom complex may be observed, consisting of herpes oticus in the area of the outer ear and tympanic membrane, with a sensation of pain in the ear, paralysis of the facial nerve, and sometimes weakened hearing and vestibular symptoms (if the auditory nerve is also involved) .
The important relationships of the facial nerve with the trigeminal and glossopharyngeal nerves in relation to the middle ear are presented schematically in Fig. 25.
1 There are, however, other opinions regarding the course of the taste fibers of the drum string, which we will not dwell on here. In any case, this issue cannot be considered finally resolved.
[to contents]
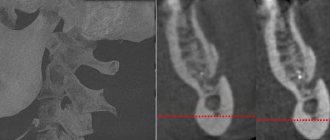
Facial nerve: treatment in children
Damage to the facial nerve in children is more common than damage to other cranial nerves, which is due to its anatomical features. The facial nerve is supplied with blood from the external carotid artery system, therefore, when the head is hypothermic, spasm of the external carotid artery leads to nerve ischemia, swelling and compression of the facial nerve. Compression of the facial nerve develops especially easily when the process is localized in the narrow canal of the temporal bone pyramid. The facial nerve canal is connected to the tympanic cavity and the pneumatic cells of the mastoid process. The outflow of lymph from the trunk of the facial nerve occurs in the cervical lymph nodes. In childhood, damage to the cervical lymph nodes is often observed.
Facial nerve: causes of damage, causes of neuritis, neuralgia, neuropathy, paresis, paralysis
The main causes of damage to the facial nerve a are inflammatory diseases (diseases) leading to primary damage to the facial nerve and its involvement in the process secondary to pathological changes in adjacent formations. Meningitis, arachnoiditis of the cerebellopontine angle, inflammatory processes in the area of the eustachian tube (eustacheitis) and mastoid process (mastoiditis), inflammation of the ear (otitis), jaw arthritis, lymphadenitis, mumps can cause the development of neuritis, paresis, paralysis, inflammation of the facial nerve. Also the cause of damage to the facial nerve are primary and secondary polyradiculoneuritis. Traumatic damage to the facial nerve occurs during traumatic brain injury with a fracture of the base of the skull in the area of the temporal bone, during surgical operations on the ear. The cause of paralysis and paresis of the facial nerve in children can be birth trauma, the application of obstetric forceps, or facial presentation. The facial nerve suffers from various tumors of the cerebellopontine ganglion region. Neuroma of the facial nerve, Recklinghausen's neurofibromatosis, tumor of the parotid salivary gland, infiltration due to leukemia are also causes of damage to the facial nerve.
In rare cases, congenital aplasia of the facial nerve nucleus and congenital narrowness of the facial nerve canal occur.
Central palsy - facial nerve
Central paralysis of the facial muscles (facial muscles) is observed as a result of damage to the corticonuclear fibers going to the nucleus of the facial nerve. Central paralysis is characterized by dysfunction of the muscles of the lower half of the face, which have unilateral cortical innervation. The main symptom of central paralysis is the smoothness of the nasolabial fold on the side opposite to the lesion. In some patients with central paralysis of the facial muscles, mild deficiency of the orbicularis oculi muscle can be detected. Central paresis of the facial muscles is usually observed in combination with central hemiparesis, or hemiplegia. In contrast to peripheral paralysis, with central paralysis of the facial muscles, the conjunctival reflex, brow reflex, and corneal reflex are preserved, and there is no degeneration reaction.
Primary neuritis of the facial nerve
Primary facial paralysis is caused by herpes viruses, mumps, enteroviruses, and adenoviruses. Bell's palsy can develop with general or local hypothermia of the face. Bell's palsy is characterized by acute development within 3 to 24 hours. The leading role in the development of Bell's palsy belongs to ischemia, which develops due to vasospasm, or vasodilation with the development of swelling of the facial nerve and compression of the nerve.
Often, neuritis of the facial nerve occurs for no apparent reason against the background of absolute complete health. Sarklinik observed many cases where the first symptoms of facial neuritis appeared after a person slept, at the moment of awakening. This may be due to the activation of chronic infection with weakened immunity, the development of various allergic reactions.
Neuritis of the facial nerve secondary
Secondary neuritis of the facial nerve is most often of otogenic origin, observed after or during otitis, mastoiditis, eustacheitis. In these cases, reactive inflammation of the nerve trunk develops. Also, the inflammatory process can penetrate directly into the facial nerve itself due to the penetration of infectious agents into it. This is often observed with purulent epidemic partitis, lymphadenitis of the stylomastoid area. Secondary neuritis of the facial nerve can occur with infectious mononucleosis, toxoplasmosis, typhus, tuberculous meningitis, acute leukemia, cranial polyneuritis, polyradiculoneuritis.
Neuritis of the facial nerve occurs with fractures and cracks of the base of the skull passing through the pyramid of the temporal bone (post-traumatic neuritis of the facial nerve). Hereditary factors and congenital developmental anomalies play a major role in the occurrence of paresis of the facial muscles. There are aplasia of the facial nerve trunk and aplasia of the nucleus of the facial nerve. In this case, there may be unilateral and bilateral violations.
The occurrence of neuritis of the facial nerve is facilitated by a narrowing of the fallopian canal and an increase in the size of the styloid process.
Damage to the facial nerve can be one of the signs of such syndromes as Melkersson-Rosenthal syndrome, Mobius syndrome.
Anatomy of the nerves in the lower third of the face
The marginal mandibular nerve can be damaged during injection correction of the cheeks, jawline and neck. Caution must be exercised when injecting fillers into the midmandibular border, even with a cannula, as nerve damage may impair mobility.
In most cases, the marginal mandibular nerve passes anteriorly above the border of the mandible, but in 19% of cases it passes below this border. the cervical branch of the facial nerve is also at risk .
When correcting the neck, it is necessary to avoid introducing dermal fillers into the subplatysmal plane.
Chin augmentation requires a mental nerve . Care must be taken to avoid nerve damage, which can lead to loss of sensation in the front of the chin and lower lip. Equally careful injection of dermal fillers into the supraperiosteal plane is necessary.
Neuritis of the facial nerve diagnosis
Diagnosis of facial nerve neuritis is based on an analysis of the symptoms preceding and accompanying diseases of the nerve damage. Neurologists, neuropathologists, and reflexologists distinguish such forms of damage as neuritis of the facial nerve and neuropathy of the facial nerve. According to pathogenesis, neuritis is divided into primary and secondary.
Neuritis of the facial nerve must be differentiated from isolated damage to the motor nucleus of the nerve, a variety of common pathological processes in the area of the cerebellopontine angle. Damage to the nucleus of the facial nerve is accompanied by isolated paresis of the facial muscles of the same half of the face without autonomic and sensory disorders, which occurs mainly in the pontine form of poliomyelitis or poliomyelitis-like diseases, tick-borne encephalitis.
When the lower parts of the bridge are damaged, which occurs with tumors, encephalitis, vascular diseases, along with the nucleus of the facial nerve, the pyramidal tract is involved in the pathological process. In such cases, peripheral paresis of the facial muscles is combined with central hemiparesis of the opposite side (Millard-Hübler syndrome). If the nucleus of the abducens nerve is affected, then paresis of the external rectus muscle of the eye (Fauville syndrome) is added to the above symptoms.
Isolated neuritis of the facial nerve is differentiated from processes in the area of the cerebellopontine angle, which develop, for example, with arachnoiditis, tumors of the vestibulocochlear nerve, which is manifested by decreased hearing, deafness, paresis of the facial muscles, sometimes dysfunction of the trigeminal nerve, contralateral spastic hemiparesis.
Polyneuritis and polyradiculoneuritis often involve lesions of the facial nerve. Usually the lesion in these cases is bilateral, often asymmetrical, accompanied by limited or diffuse damage to other parts of the human peripheral nervous system.
Treatment of facial nerve neuropathy
A combination of drug and non-drug methods is used for treatment. As a rule, doctors prescribe medications from these groups:
- non-steroidal anti-inflammatory drugs (NSAIDs): ibuprofen, meloxicam, nimesulide, diclofenac and other drugs; necessary to relieve pain and inflammation, eliminate swelling; used for mild to moderate neuropathy;
- glucocorticosteroids: prednisolone, hydrocortisone, dexamethasone; have an anti-inflammatory effect, relieve swelling; used for severe forms of the disease, as well as when NSAIDs are ineffective;
- diuretics: furosemide, lasix; necessary to eliminate tissue swelling;
- vascular drugs: pentoxifylline, nicotinic acid, cavinton; stimulate active blood flow in the affected area, improve tissue nutrition;
- metabolic agents: actovegin; necessary to stimulate metabolism and regenerate damaged structures;
- antiviral and antibacterial agents for the infectious nature of the pathology;
- anticholinesterase drugs: neuromidin, axamon; improve the transmission of excitation from nerve to muscle, help to quickly get rid of paralysis of facial muscles;
- B vitamins: milgamma, combilipen; stimulate nerve regeneration and improve impulse conduction.
If neuropathy has become chronic and muscle paresis has given way to spasm, muscle relaxants are prescribed: mydocalm, carbamazepine, baclofen. They replace anticholinesterase drugs and promote muscle relaxation. If these remedies are ineffective, injections based on botulinum toxin are used.
Drug treatment is complemented by physiotherapy. In the acute period the following are used:
- UHF;
- exposure to alternating magnetic field;
- phonophoresis with hormones.
After one and a half to two weeks from the onset of the disease, these methods are added:
- electrotherapy (diadynamic currents, etc.);
- electrical stimulation of muscles;
- electrophoresis;
- magnetic therapy;
- laser therapy;
- Darsonvalization.
An additional effect is provided by mud applications, therapeutic baths, and acupuncture.
During the acute period it is also recommended:
- sleep only on your side (affected side);
- tie a scarf around your face to prevent stretching of paralyzed muscles;
- carry out muscle taping: tighten the muscles using an adhesive plaster (duration from 30-60 minutes to 2-3 hours);
- tilt your head in the direction of the lesion several times a day and support the muscles with your palm; The duration of the procedure is 10-15 minutes.
After acute inflammation has subsided, it is recommended to perform therapeutic exercises to develop the affected muscles:
- frown and raise your eyebrows;
- open and close your eyes wide;
- widen the nostrils;
- puff out one's cheeks;
- smile with your mouth open and closed;
- stretch out your lips, blow out an imaginary candle, whistle;
- stick out tongue, etc.
The more the patient grimaces, the faster the muscles will recover. During the same period, a light therapeutic massage to stimulate blood circulation is acceptable.
If treatment does not bring effect within 2-3 months, doctors recommend using surgical treatment methods. Two types of operations are used:
- restoration of impulse transmission along the nerve: decompression of the nerve fiber when it is compressed in the canal of the temporal bone;
- reinnervation: replacement of the affected area with a donor nerve (segment of the hypoglossal, phrenic or accessory nerve, as well as healthy branches of the facial nerve);
- partial suturing of the eyelids (tarsophasia);
The choice of a specific treatment method depends on the form of the disease, its cause, severity and level of damage.
Make an appointment