Often you can meet people with an interesting facial expression: it is asymmetrical, as if distorted, emotionless, perhaps accompanied by small muscle twitches.
All these signs are united by a common name - facial neurosis. This condition can have a different nature of occurrence and is provoked by both objective reasons and factors of a psychogenic nature.
Unusual sensations
It happens that a person can feel phenomena in the face and head that are unusual for the usual state. They are called paresthesias and are manifested by the following symptoms:
- tingling;
- burning;
- "goosebumps"
- numbness;
- itching and rashes.
Often facial paresthesias have an organic basis and become a sign of the disease:
- neuritis, neuralgia of the cranial nerves;
- multiple sclerosis;
- stroke and other circulatory disorders in the brain;
- shingles;
- migraine;
- diabetes;
- epilepsy;
- hypertension.
In certain cases, unusual sensations are observed in certain parts of the face. For example, similar manifestations in the language may appear for the reasons listed above, but often have a different etiology. They are provoked by cancer of the tongue and larynx, as well as trauma by a splintered tooth or denture.
Dental procedures cause numbness and other unusual feelings, especially after tooth extraction. Another reason for their appearance may be an uncomfortable position during sleep or an unsuitable pillow. But the sensations caused by such phenomena usually pass soon.
Another group of provoking factors consists of psychogenic and neurogenic disorders.
Diagnosis of NLN
CT scan of the brain
- Cost: 6,000 rub.
More details
If you suspect facial neuropathy, you should consult a neurologist as soon as possible. Other neurological diseases have similar symptoms to NLN. To avoid mistakes, the neurologist prescribes standard examinations.
- Laboratory tests
Blood, urine, blood glucose, serological tests (antigen-antibody) if infection is suspected - Chest X-ray
Detects tuberculosis, tumor process, scars and lumps - MRI and brain
MRI identifies possible pathological processes at the base of the brain, CT scan – to study the temporal bone - Electroneuromyography
Determines the speed of nerve impulse conduction in muscles, reveals connective tissue degeneration of nerve fiber - Consultation with a therapist, ENT specialist, endocrinologist, infectious disease specialist
If there are concomitant diseases
When the diagnosis is completed, there is no doubt left.
Electroneuromyography (ENMG) must be performed as early as possible to determine the severity of the disease and prognosis.
This method determines which part of the nerve is more damaged - the myelin sheath or the central axon. Damage to the myelin sheath has a more favorable prognosis because it is restored in most cases. Axonal damage is much more serious.
Disorders of facial innervation
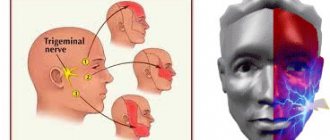
A neurotic face may develop due to damage to the nerves that innervate it. Most often these are the trigeminal and facial nerves.
The trigeminal nerve is the 5th pair of cranial nerves. It is the largest of all 12 pairs of these nerve fibers.
N. trigeminus arises symmetrically on both sides of the face and consists of 3 large branches: the ophthalmic, maxillary and mandibular nerves. These three large processes innervate a fairly large area:
- skin of the forehead and temples;
- mucous membrane of the oral and nasal cavities, sinuses;
- tongue, teeth, conjunctiva;
- muscles - chewing, floor of the mouth, palatine, tympanic membrane.
Accordingly, when it is damaged, pathological sensations arise in these elements.
Facial nerve – 7th pair of cranial nerves. Its branches surround the temporal and ocular region, the zygomatic arch, and descend to and behind the lower jaw. They innervate all facial muscles: auricular, orbicularis and zygomatic, chewing, upper lip and corners of the mouth, cheek. As well as the muscles of the lower lip and chin, around the mouth, the muscles of the nose and laughter, and the neck.
N. facialis is also paired, and is located on both sides of the face.
In 94% of cases, the damage to these nerve fibers is unilateral, and only 6% is a bilateral process.
Disruption of innervation can also be primary or secondary.
Primary is the lesion that initially involves the nerve. This could be hypothermia or strangulation.
Secondary damage develops as a consequence of other diseases.
Another reason for the development of facial neurosis is neurogenic and mental disorders. When unpleasant sensations in the face and head occur against the background of psycho-emotional arousal, shock, or as a result of stressful situations.
Causes
Inflammation of the facial nerve can occur due to its compression by a tumor, aneurysm of a vessel, or swelling of soft tissues with the development of “tunnel syndrome.” In this case, damage to both the root and the trunk of the nerve canal is possible.
The inflammatory process may spread to nerve tissue from the adjacent area. In particular, neuritis can occur against the background of inflammatory disease of the middle ear (otitis).
Often the cause of nerve damage is a viral or other infection, such as herpes or paramyxovirus (mumps).
An ischemic cause of inflammation is also possible, that is, a violation of the blood supply to the nerve due to vascular atherosclerosis or stroke. The provoking factor for the development of the disease is usually severe cooling of the face in a cold wind, rain or draft. This especially often occurs against the background of emotional experiences, stress, psycho-emotional overload or overwork.
Another possible cause of inflammation is trauma received, for example, during deep dental treatment or surgery.
Neuritis of the facial nerve occurs when there is an imbalance of the Rlung base, the main causes of which are poor nutrition, hypothermia (especially exposure to cold wind), stress, overwork, lack of sleep, psycho-emotional overload, negative emotions and mental trauma.
Wind imbalance can occur against the background of fasting, low-calorie diet, strict diet, abuse of dry, rough foods high in plant fiber.For example, a strict diet based on raw vegetables, greens, lettuce, citrus fruits can provoke an imbalance of Wind, which, on the one hand, manifests itself as restlessness, anxiety, irritability, insomnia, and on the other hand, increases the risk of neuritis and neuropathies, in particular the facial nerve.
Kulbuzhev Murat Sultanovich Reflexologist, neurologist Experience 30 years
Facial nerve neurosis
Neuritis (neurosis N. Facialis) or Bell's palsy occurs due to inflammation of the nerve fiber. Reasons leading to this condition:
- pinched nerve as a result of narrowing of the channel through which it passes. This may be a congenital phenomenon or result from inflammation;
- hypothermia;
- other diseases and infections: herpes, mumps, otitis media, stroke, cancer, central nervous system infections;
- injury N. Facialis.
The onset of the disease is usually gradual. Manifested by pain in the behind-the-ear area. After a couple of days, neurological facial symptoms appear:
- smoothing of the nasolabial fold, drooping of the corner of the mouth;
- the face becomes asymmetrical with a skew towards the healthy side;
- eyelids do not droop. When you try to do this, your eye rolls;
- any attempt to show at least some emotion ends in failure, since the patient cannot move his lips, smile, or manipulate his eyebrows. Such manifestations can worsen to the point of paresis and paralysis of the facial muscles, that is, to partial or complete immobility of the affected part of the face;
- taste sensitivity decreases, salivation appears;
- the eyes are dry, but there is lacrimation when eating;
- hearing on the affected side worsens.
The severity of pathological symptoms depends on the degree and area of damage to the nerve fiber. If the disease is treated inadequately, complications may arise in the form of muscle contractures (immobility).
Since the disease is inflammatory in nature, its treatment is aimed at eliminating it. For this, the patient is prescribed hormonal anti-inflammatory drugs - glucocorticoids, as well as decongestants.
Other methods include:
- prescription of vasodilators and analgesics, B vitamins;
- anticholinesterase agents to increase nerve conduction;
- drugs that improve metabolism in nervous tissue;
- physiotherapy;
- massage, exercise therapy in the recovery stage.
And only in extreme cases, when conservative therapy is ineffective, neurosurgical intervention is resorted to.
Diagnostics
Thanks to the characteristic symptoms, establishing a diagnosis for neuritis of the facial nerve does not cause difficulties. Diagnostics is aimed mainly at determining the causes, nature of the inflammatory process, as well as concomitant diseases.
At the initial appointment, the doctor examines and palpates the face, assesses the degree of muscle spasticity and movement disorders. At the same time, he pays attention to the smoothing of natural folds (nasolabial, frontal, etc.), as well as to the non-closure of the eyelids (the inability to close the eye).
For this purpose, several standard tests are performed in which the patient is asked to close his eyes, try to smile, close his eyes, frown, wrinkle his forehead, puff out his cheeks, blow, wrinkle his nose, raise his eyebrows, and bare his teeth. In addition, the taste sensitivity of the tongue is determined.
If additional data is needed, the patient is sent for an MRI or CT scan to identify possible lesions of the brain, blood vessels (in particular, the presence of a tumor, hematoma, aneurysm, etc.), and the presence of inflammatory foci.
To assess the affected area and disturbances in the innervation of facial muscles, electromyography (EMG) is used - a method for studying bioelectrical activity. Using electroneurography, the speed of signal transmission through nerve channels (fibers) is assessed.
In addition, a general urine and blood test and a biochemical blood test are performed.
Important! Eastern medicine views the human body as a single system. Inflammation of the peripheral nerves in this context represents a particular, local manifestation of a general imbalance, almost never the only one.
Therefore, when diagnosing neuritis, a doctor of oriental medicine assesses the degree of imbalance as a whole, identifies concomitant diseases, disorders, functional disorders of the nervous, hormonal, reproductive, immune and other systems.
A treatment plan is designed to address the common causes of all these disorders.
Trigeminal neuralgia
This is another lesion of the nerve fiber structure, which is often chronic and accompanied by periods of exacerbation and remission.
It has several causes, which are divided into idiopathic - when a nerve is pinched, and symptomatic.
The main symptom of neuralgia is paroxysmal sensations in the form of pain on the face and in the mouth.
Pain sensations have characteristic differences. They are “shooting” and resemble an electric shock; they arise in those parts that are innervated by the n.trigeminus. Having appeared once in one place, they do not change localization, but spread to other areas, each time following a clear, monotonous trajectory.
The nature of the pain is paroxysmal, lasting up to 2 minutes. At its height, a muscle tic is observed, that is, small twitching of the facial muscles. At this moment, the patient has a peculiar appearance: he seems to freeze, but does not cry, does not scream, and his face is not distorted from pain. He tries to make a minimum of movements, since any of them increases the pain. After the attack there is a period of calm.
Such a person performs the act of chewing only with the healthy side, at any time. Because of this, compaction or muscle atrophy develops in the affected area.
The symptoms of the disease are quite specific, and its diagnosis is not difficult.
Therapy for neuralgia begins with taking anticonvulsants, which form its basis. Their dose is subject to strict regulation and is prescribed according to a specific scheme. Representatives of this pharmacological group can reduce agitation and the degree of sensitivity to painful stimuli. And, therefore, reduce pain. Thanks to this, patients have the opportunity to freely eat and talk.
Physiotherapy is also used. If this treatment does not give the desired result, proceed to surgery.
Treatment methods
Depending on what caused the inflammation, a course of treatment is prescribed. For bacterial lesions, the emphasis is on antibacterial therapy through systemic administration of drugs.
However, regardless of the reasons, the doctor prescribes painkillers to relieve pain and reduce inflammation. It could be:
- ibuprofen;
- paracetamol;
- analgin;
- ketorol;
- diclofenac.
All of the listed drugs can be prescribed either in the form of tablets for oral administration, or prescribed in the form of solutions for intramuscular administration.
When conservative methods are not possible, the help of a surgeon may be needed. This primarily concerns abscesses due to the eruption of wisdom teeth, pulpitis or other dental diseases. In this case, the abscess will be opened, pus will be removed, the wound will be treated with antiseptic, and the tooth will be removed, if necessary. If a pinched nerve occurs as a result of pathologies in the structure of the skull, the surgeon will perform an operation to correct the situation and free the nerve bundles.
As a complex therapy, massage, heating or exposure to a magnetic field and electric current can be prescribed. You cannot massage or warm the inflamed area yourself, because this can lead to complications associated with rupture of the purulent capsule, blood poisoning and paralysis of the facial nerve.
Separately, you may need to consult a neurologist who will determine the cause of the inflammation if other specialists have not found obvious foci of infection and abscesses.
Traditional methods of treatment are permissible only as an addition to the main therapy. For example, rinsing with chamomile decoction will relieve inflammation and reduce swelling. But you can resort to such procedures only with the permission of the attending physician.
Real life examples
Some famous people, whose fame sometimes trumpets all over the world, were also hostage to the pathology of the facial nerve.
Sylvester Stallone, who is known for his enchanting roles, was injured at birth. The actor's mother had a difficult birth and he had to be pulled with forceps. The result is damage to the vocal cords and paresis of the left side of the face. Because of this, Stallone had problems with speech, which became a reason for ridicule from his peers.
The actor grew up as a difficult child. But, in spite of everything, he managed to overcome his defect and achieve considerable success, although partial immobility of his face remained.
Domestic showman Dmitry Nagiyev received facial asymmetry, which was nicknamed “Nagiyev’s squint”, due to paresis of the facial nerve. The illness happened unexpectedly. As a theater student, one day he felt that his face was not moving.
He spent 1.5 months in the hospital to no avail. But one day in his room a window broke due to a draft. Fright provoked a partial return of mobility and sensitivity of the facial part, but the left part retained its immobility.
Facial nerve: causes of damage, causes of neuritis, neuralgia, neuropathy, paresis, paralysis
The main causes of damage to the facial nerve a are inflammatory diseases (diseases) leading to primary damage to the facial nerve and its involvement in the process secondary to pathological changes in adjacent formations. Meningitis, arachnoiditis of the cerebellopontine angle, inflammatory processes in the area of the eustachian tube (eustacheitis) and mastoid process (mastoiditis), inflammation of the ear (otitis), jaw arthritis, lymphadenitis, mumps can cause the development of neuritis, paresis, paralysis, inflammation of the facial nerve. Also the cause of damage to the facial nerve are primary and secondary polyradiculoneuritis. Traumatic damage to the facial nerve occurs during traumatic brain injury with a fracture of the base of the skull in the area of the temporal bone, during surgical operations on the ear. The cause of paralysis and paresis of the facial nerve in children can be birth trauma, the application of obstetric forceps, or facial presentation. The facial nerve suffers from various tumors of the cerebellopontine ganglion region. Neuroma of the facial nerve, Recklinghausen's neurofibromatosis, tumor of the parotid salivary gland, infiltration due to leukemia are also causes of damage to the facial nerve.
In rare cases, congenital aplasia of the facial nerve nucleus and congenital narrowness of the facial nerve canal occur.
Migraine
This condition is accompanied by attacks of unbearable headache. It is also associated with disruption of the trigeminal nerve, or more precisely, with its irritation in one part of the head. This is where the pain is subsequently localized.
The onset of migraine includes several stages:
- initial;
- aura;
- painful;
- final one.
Paresthesia of the head and face appears with the development of the aura stage. In this case, the patient is bothered by a feeling of tingling and crawling, which occurs in the arm and gradually moves to the neck and head. The person’s face becomes numb and it becomes difficult for him to speak. I am concerned about dizziness and visual disturbances in the form of light flashes, floaters and a decrease in the field of vision.
Facial paresthesia is a precursor to migraine, but often the attack occurs without the aura stage.
Classification of the disease
Due to the occurrence
- Primary (idiopathic) trigeminal neuralgia. A classic type of neuralgia, so to speak. Occurs due to compression of the trigeminal nerve.
- Secondary trigeminal neuralgia is a consequence of other diseases and viruses.
By coverage
- Unilateral (one branch of the trigeminal nerve is affected).
- Bilateral (more than one branch is affected).
Neuralgia can affect the 1st, 2nd, 3rd branches of the trigeminal nerve. The first branch is responsible for the orbital zone, the second for the median zone (including the nose and upper lip), and the third for the lower jaw. Most often, damage to the third branch is diagnosed, so the pain affects the area of the lower jaw, and an attack often occurs during hygiene, eating or shaving.
Psychogenic causes of facial neurosis
Undoubtedly, disturbances in facial sensations quite often become a consequence of pathology of internal organs and blood vessels.
But often they are caused by psychological disorders and pathological thoughts that arise in our heads.
Facial paresthesias can be situational in nature and develop during episodic nervous excitement: as a result of quarrels, prolonged and intense screams. Such phenomena cause overstrain of the muscles, especially the cheeks and those located around the mouth. As a result, we experience facial numbness and even mild soreness.
The feeling of fear causes us to breathe quickly and shallowly, or to hold our breath. Disturbances in the respiratory rhythm can also provoke impressions that are atypical for us. A feeling arises that is characterized as a “chill running through.” Moreover, it is more concentrated at the roots of the hair. In this case they say: “chills to the marrow of the bones.” The face also becomes cold, a slight tingling appears in its area.
Such phenomena are disturbing when we are overwhelmed by strong emotions. But they accompany people suffering from mental disorders systematically.
A special type of neurotic facial manifestations is a nervous tic. It is characterized as an uncontrolled and systematic contraction of the facial muscles.
The disorder more often accompanies men. And it manifests itself with the following symptoms:
1.Motor:
- frequent blinking, winking;
- setting the lips with a tube;
- nodding head;
- constant spitting or sniffing;
- opening or upturning of the corner of the mouth;
- wrinkling of the nose.
2. Vocal:
- screaming;
- grunt;
- coughing;
- repetition of words.
There are also signs – precursors – that signal the appearance of a tic.
These include itching, facial heat and other paresthesias. Naturally, these signs are considered pathological if they occur in an inappropriate situation. It happens that only the patient himself feels them, but they are not visible to others.
But often twitching and other nervous symptoms become noticeable by other people, and they cause a lot of discomfort to the patient.
Tics can be simple, when there is only one symptom, or complex, which combines several manifestations.
The most common, main cause of tics is mental stress. It can be caused by a strong stress factor of one-stage action. Perhaps you were very scared of something, or broke up with your loved one. That is, the shock was so strong for you that your nervous system lost control.
Or, on the contrary, disorders develop as a result of prolonged monotonous exposure. Symptoms often appear due to lack of sleep and overwork.
Their duration varies. A situational nervous tic disappears a few hours or days after the cause is eliminated. In another case, it persists for years or haunts the patient throughout his life. In such a situation, in addition to eliminating the provoking factor, subsequent psychological work with the patient is required. This type of disorder is called chronic.
A nervous tic can be one of the signs of mental disorders such as neurosis, obsessive thoughts and phobias, depression.
Another group of provoking factors include:
- diseases - stroke, brain injury, infections or poisons;
- neurodegenerative diseases - Huntington's chorea. Characterized by destruction of brain tissue. Accompanied by uncoordinated, sudden movements, as well as neurological disorders of the face. Of these, the first sign is slow eye movements. Then a muscle spasm of the face occurs, which manifests itself in grotesque facial expressions - grimacing. Speech, chewing and swallowing are impaired;
- burdened heredity;
- parasitic infestations;
- eye fatigue due to prolonged eye strain;
- unbalanced diet, when the body receives little magnesium, calcium, glycine. These elements participate in the normal conduction of nerve impulses and are responsible for the coordinated functioning of the nervous system.
Nervous tics in children
There are several types of such disorders in childhood.
Transient tic disorder begins to manifest itself during early school age. Its duration ranges from 1 month to 1 year. Motor types of tics occur more often. Mainly typical for children with developmental delays and autism.
Chronic disorder occurs before age 18. And lasts from 1 year and above. In this case, either motor or vocal tics develop. The earlier the pathological symptoms appear, the easier and faster they pass.
Tourette syndrome is a multiple tic disorder characterized by both motor and movement types. A serious disease, which, however, softens with age.
A special type of disease, which is also characterized by signs of the nervous type, is minor chorea. It develops against the background of infections caused by streptococcus: sore throat, tonsillitis, rheumatism. Accompanied by pathological changes in nervous tissue.
Along with hyperkinesis, emotional instability, irritation, restlessness and anxiety, this condition corresponds to neurotic changes in the face. They are expressed in tension and spasms of the facial muscles, which is often mistaken for grimacing. There is also a spasm of the larynx, manifested in inappropriate screams.
At school, such children, not knowing the true cause of facial hyperkinesis, and even in combination with increased activity, are reprimanded and kicked out of class. Such an attitude towards the child forces him to miss school classes and avoid going to school. Treatment for chorea minor, along with sedatives, includes antibiotics to fight infection and anti-inflammatory drugs.
A nervous tic leaves a heavier imprint on a child’s psyche than on an adult. It often causes anxiety and detachment, withdrawal, and even provokes depressive disorders. Causes sleep disturbances, speech difficulties, and learning difficulties.
Tic disorders lead to distorted self-perception and decreased self-esteem.
Parents of such children are advised not to focus the child’s attention on the problem. On the contrary, they recommend finding ways to shift attention and increase self-esteem. A special place is given to support groups for such people and communication in general.
How to get rid of nervous tics
In order to free yourself from unpleasant sensations, you must first eliminate their problem. Sometimes all it takes is a good night's sleep. In another case, you need to change the situation for a while, get out of the destructive environment.
Among the auxiliary methods used are herbal soothing teas, baths with the addition of aromatic oils, swimming, walks in the fresh air or sports: running, yoga.
Add ingredients with a high content of calcium and magnesium to your menu. These include fermented milk products, buckwheat, bran bread, red fish, eggs, and meat. Vegetables and fruits include beets, currants, dried fruits, nuts and parsley.
If these foods do not fit into your diet, consider taking appropriate vitamin supplements. Do not overuse strong tea and coffee.
And most importantly: remain optimistic and calm in any situation!
In cases where the condition worsens, psychotherapy is sought. Cognitive behavioral therapy is especially effective in helping to stop tic disorders at the stage of their precursors.
Habit reversal therapy teaches patients movements that help prevent the development of neurological facial symptoms.
Medications include anticonvulsants and muscle relaxants, Botox injections, and antidepressants.
If the above methods are ineffective in combating nervous tics, they turn to deep brain stimulation. A device is installed in the GM that controls electrical impulses.
How to remove teak yourself
If a nervous facial tic is situational and is not too intense, but at the same time obsessive, you can try to get rid of it using physical methods.
One way is to try to disrupt the pathological muscle rhythm by overexerting it. For example, if your eye twitches, try to close your eyes tightly.
It is possible to calm an overexcited muscle through a light massage. Or apply cold to it. The temperature difference will also help. Wash your face alternately with cold and warm water.
Dermatillomania
Neurosis of the face and scalp can manifest itself in a behavioral disorder such as dermatillomania.
Its main manifestation is scratching the skin of the face and head, not because of itching, but because of dissatisfaction with its appearance. This also includes an obsessive zeal to squeeze out pimples, scratch off scabs, and pull out hair. Self-injurious actions cause a short-term feeling of pleasure, followed by feelings of shame, frustration, and dissatisfaction.
The face of such patients is covered with scars and scars due to constant trauma to the skin. This process is uncontrollable and can occur at any time of the day. But most often traumatic actions are carried out in front of a mirror.
Symptoms of the disorder also include the habit of biting the lips and mucous membranes of the cheeks. Patients are not deterred by the prospect of redness, bleeding, and scarring of the skin. They repeat the ritual day after day. It lasts from a few minutes to an hour.
Such actions can be provoked by feelings of fear, anxiety, and close examination of one’s skin because there is nothing to do.
Dermatillomania has been described as a state of addiction. It begins with concentrating on what the patient thinks is a skin defect. Gradually, attention is increasingly focused on this detail. A person begins to think that he is sick with something serious. This provokes irritability and nervousness in him, leading to obsessive actions.
The root cause of the disease is rooted in the psychological state of a person and lies in self-dissatisfaction, anger, feelings of shame and malice. Traumatic rituals are a way of punishment, self-flagellation.
Treatment of this pathology requires the intervention of a psychotherapist and a dermatologist.
The main method of treating addiction is psychotherapy, in particular cognitive behavioral therapy.
Yoga, physical exercise, relaxation procedures, as well as any hobby that absorbs a person and helps redirect attention will help reduce anxiety, distract and relax.
The help of a dermatologist is necessary to eliminate skin lesions in order to prevent infection and reduce the degree of dermatological defect.
Neuroses
This is a large group of diseases, manifested primarily in psycho-emotional disorders, as well as malfunctions of the autonomic nervous system. They do not cause pathological disorders of the nervous tissue, but have a significant impact on the human psyche.
There are several types of disorders in which the symptoms are visible.
Muscular neurosis is manifested by muscle tension, spasm and convulsive twitching. Neurosis of the facial muscles makes itself felt with the following manifestations:
- nervous tic;
- lip tension, clenching;
- convulsive contraction, the face seemed to move;
- tingling, burning sensation;
- muscle pain;
- Tension of the neck muscles is manifested by a feeling of lack of air, a lump in the throat.
When we find ourselves in a stressful situation, our body produces stress hormones. They, among many other reactions, cause muscle tension. Now imagine, if we are exposed to chronic stress, what happens to our muscles, and specifically to the muscles of the face. Being systematically in hypertonicity, they overexert themselves. This is what causes their nervous twitching, spasms, and convulsions.
Another type of neurosis is skin. It causes paresthesias in the facial skin of the following type:
- severe itching, burning in the facial and scalp without clear localization;
- sensation as if something were touching the face. And it's terribly annoying;
- the appearance of red spots on the face and neck. Possible rash.
The causes of such phenomena are nervous and mental overstrain, chronic stress, sleep disturbances, as well as disruptions in hormonal regulation.
With neuroses associated with disruption of the autonomic nervous system, various manifestations may also occur. Malfunctions in the functioning of the vascular network occur, and a vascular neurotic disorder develops.
Vascular neurosis of the face is manifested by flaking and dryness, a feeling of tightness of the skin. She becomes pale, sometimes cyanotic, and her sensitivity worsens. In addition, sneezing appears, the nose is stuffy, the eyes become red and watery, the skin itches and itches. This indicates the development of vegetative-allergic reactions.
What is the trigeminal nerve and why does it become inflamed?
The trigeminal nerve on the face is the nerve through which we feel the face and can bite and chew. On each side of the face there is a trunk with three branches - the orbital nerve, the maxillary nerve and the mandibular nerve. This nerve is the most complex in the skull.
Inflammation of the trigeminal nerve (or, in other words, neuralgia or neuritis) can be caused by several reasons.
Firstly, this is damage to the fibers by a bacterial infection. Pathology can also be caused by:
- injury or abnormal structure of the skull bones;
- hypothermia of the head;
- high blood pressure;
- stroke;
- intoxication, poisoning;
- tuberculosis;
- infection with herpes or HIV;
- high intracranial pressure due to osteochondrosis;
- inflammatory diseases of the gums, mainly in the area of wisdom teeth;
- changes in hormonal levels, for example, during pregnancy;
- procedures in the dentist's office. Installation of a filling or removal of roots may be accompanied by contact with nearby nerves.
Doctors also identify a complex of psychosomatic causes - stress, strong experiences that affect well-being.