What is mandibular nerve injury?
By this concept, dentists mean injury to one of the nerves:
- chin;
- lingual;
- alveolar.
Types of injuries include sprain, compression, crushing and rupture - partial or complete. The cause of the stretching is the long-term retraction of the mucoperiosteal flap, which is created by an implant of greater length than necessary. Crush injuries and compression are caused by needle injuries during the administration of anesthesia. Rupture occurs in two cases: when cutting the mucosa or during preparation of the hole for the implant.
Algorithm for patient management in the acute phase (first 30 hours)
There is a limited time window of up to 30-48 hours to make the most correct decision - to recognize the fact of damage to the alveolar and/or lingual nerve after implantation, endodontic treatment or removal of mandibular third molars.
Report by reference Khawaja N, Renton T Case studies on implant removal influencing the resolution of inferior alveolar nerve injury. Br Dent J. 2009 Apr 11;206(7):365–370 suggests that early removal of the causative implant (within the first 30 hours) results in maximum recovery, but the evidence remains weak.
Suggested protocol based on available evidence:
- Homecheck - The attending physician should contact the patient between 6 and 24 hours after surgery to determine the presence/absence of persistent partial neuropathy after local anesthesia has worn off. This contact is based on the relationship between doctor and patient, which is achieved through signed informed consent.
- Confirm the presence of neuropathy . If the neuropathy affects +/- most of the dermatome, severe nerve injury should be considered, which will be accompanied by neuropathic severe pain if not treated immediately.
- Admit the damage and apologize. An apology is NOT an admission of guilt.
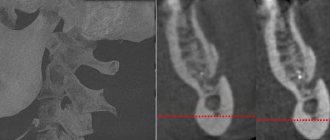
- Additional CT scans or radiography are not necessary or valuable for decision-making in cases of implantation, but are absolutely necessary in cases of third molar extraction.
- Initiate treatment for implant-related nerve damage: - Consider removal of the implant within 30 hours of implantation or sooner; - early therapeutic treatment.
- Acute phase - nerve damage during surgery - Implant removal, immediate nerve restoration +/-.
Causes and prevention of mandibular nerve injuries
The only cause of such damage is considered to be medical errors. Since in preparation for implantation, X-rays of the jaw are taken, which the doctor must carefully study so that when choosing an implant and a place for it, he does not injure the nerve, the injuries are caused by his unprofessionalism or negligence.
Damage to the mandibular nerve most often occurs when:
- improper administration of anesthesia - needle injury;
- choosing an implant that is too long;
- damage by an instrument - when preparing the site for the implant.
The only way to avoid such an injury is for a doctor to responsibly approach the stage of preparation for surgery, carefully studying the condition and structure of his patient’s jaw. The only way of prevention for the patient is to choose a trusted clinic and a highly qualified doctor. Specialists at the Implantmaster clinic have been able to reduce the number of injuries of this kind to 2%, since they carefully study three-dimensional photographs of a person’s jaw before implantation, and can correctly assess the condition of the bone tissue, the location of nerves and blood vessels, and select the optimal size of the implant.
Management of patients with post-traumatic sensory neuropathy
Consultation with a patient with post-traumatic sensory neuropathy usually requires a minimum of 30–40 minutes of time.
- It is necessary to carefully and in detail collect a medical history, including: - date and origin of nerve damage; — patient’s self-assessment of neurosensory function in terms of changes in sensitivity: hyperesthesia, hypoesthesia, anesthesia; — patient self-assessment of neurogenic discomfort and regular pain: paresthesia, dysesthesia, allodynia, dysgeusia, ageusia (loss of taste); — psychological screening; — functional screening (impact on daily life).
- It is necessary to conduct a series of standardized tests of neurosensory functions, using mapping to assess the size of the neuropathic area, determine the nature of functional problems and assess the level of pain. Pain is assessed using a visual analogue scale, where 0 is no pain and 10 is the worst possible pain.
- Assess the percentage of the neuropathic area of the extraoral and intraoral dermatomes, where 100% of the extraoral dermatome - the entire extraoral area of the skin innervated by the inferior alveolar nerve on the damaged side is involved in changes, 100% of the intraoral dermotome - the entire mucosa in the area of innervation of the lingual nerve on the damaged side is affected.
- Inform the patient about the diagnosis, extent of injury, probable cause, and persistence of injury.
- Discuss possible symptomatic and etiological treatment strategies and expectations regarding such treatment. Inform the patient how his symptoms are explained by current understanding of neurobiology (eg, cold allodynia).
- The patient must be given the opportunity to communicate by telephone with the doctor.
It is important to differentiate post-traumatic neuropathy from trigeminal neuropathy associated with malignancy, multiple sclerosis, sickle cell disease, neurological disease, alcoholism, trauma, diabetes, HIV, postherpetic neuralgia, stroke, or chemotherapy.
Management options for patients with post-traumatic neuropathy will depend on understanding of the mechanisms and duration of injury, the symptoms identified, and the wishes of the patients.
Patient management strategies include:
- Comfort and observation.
- Early medical treatment (steroid hormones, vitamin B complex, and NSAIDs-nonsteroidal anti-inflammatory drugs) is aimed at minimizing the development of the inflammatory response to nerve damage and promoting its recovery. When local pain is present, there is evidence for the use of topical lidocaine 5% patch and local clonazepam injections. Botulinum toxin type A (Botox) injections for focal neuropathic pain have limited success.
- Psychiatric and psychological support in the form of cognitive behavioral therapy and based on the results of psychometric questionnaires, including the PainDETECT . It is important to reassure patients with permanent nerve damage that their condition will neither worsen nor improve, and that the condition does not predispose them to the development of any other pathology in the area. It is also very important to explain to the patient the pathological physiology of nerve fiber damage and honestly tell how difficult this condition is to treat.
- In cases of chronic pain, systemic administration of pregabalin, oxcarbazepine, venlafaxine or nortriptyline.
- Early or delayed surgical treatment, decompression or direct anastomosis.
- In cases of trigeminal neuropathic pain, alternative pain treatment strategies such as transcutaneous electrical nerve stimulation (TENS), acupuncture, low-level laser therapy, and myogymnastics may be effective.
- Speech therapy assistance.
- Observation and assessment of the dynamics of the condition according to the following results: reduction of pain, improvement of functionality and the patient’s ability to cope with iatrogenic post-traumatic neuropathy.
Typically, patients need a comprehensive approach to treating neuropathy, based on the pain, functional and psychological problems the patient is experiencing. Juodzbalys G, Wang HL, Sabalys G. Injury of the Inferior Alveolar Nerve during Implant Placement: a Literature Review. J Oral Maxillofac Res 2011 Apr 1;2(1):e1.
Our team of doctors
Maxillofacial surgeon, Implantologist
Bocharov Maxim Viktorovich
Experience: 11 years
Dental surgeon, Implantologist
Chernov Dmitry Anatolievich
Experience: 29 years
Orthopedist, Neuromuscular dentist
Stepanov Andrey Vasilievich
Experience: 22 years
Endodontist, Therapist
Skalet Yana Alexandrovna
Experience: 22 years
Orthopedic dentist
Tsoi Sergey Konstantinovich
Experience: 19 years
Dentist-orthodontist
Enikeeva Anna Stanislavovna
Experience: 3 years
Symptoms and stages of damage
The symptoms by which this complication can be recognized are as follows:
- numbness of parts of the head - tongue, lips, chin, cheeks, etc.;
- biting lips and tongue;
- choking while eating or drinking;
- profuse salivation.
All this creates a number of inconveniences for the patient: it makes it difficult to eat and talk, disrupts facial expressions, and also prevents men from shaving and women from applying makeup. The severity of this injury is determined by its degree: a minor one goes away on its own or with the help of drug treatment, a severe one leads to irreversible processes of nerve degeneration and is not curable. Damage to the mandibular nerve, the symptoms of which the patient observes, requires immediate consultation with a doctor - only a specialist will be able to determine its extent and provide timely assistance.
Dentists distinguish the following stages of this implantation complication:
- minor - neuropraxia;
- more severe, but partial damage - axonotmesis;
- a serious injury that leads to complete loss of sensitivity - neurotmesis.
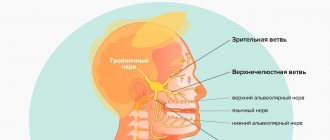
Anatomy of the trigeminal nerve
The trigeminal nerve (5th pair) is a large mixed (sensory-motor) nerve, consisting of three branches :
- Orbital (n. ophthalmicus).
- Maxillary (n. maxillaris).
- Mandibular (n. mandibularis).
The mandibular ( MF ) is the third branch of the trigeminal, innervating the skin, mucous membranes of the organs of the lower jaw, and the muscles of the lower part of the face. Its location and parameters in the human body are individual and determined by anatomical features. The nerve trunk consists of 30-80 fibers, thickness is in the range of 3.5-7.5 mm, length - 0.5-2.0 cm.
The roots of the mandibular nerve transmit information from the lower part of the face and oral cavity: teeth, gums, tongue, outer part of the ear. Motor - innervate the masticatory and part of the facial muscles.
At the exit from the skull, the LF is divided into two branches:
1. Sensitive ( anterior ) - innervating the mucous membranes and skin:
- cheeks, chin;
- floor of the mouth;
- lower teeth, jaw;
- lower lip, back of tongue;
- salivary glands (sublingual and submandibular);
- parts of the outer ear.
2. Motor ( posterior ) - ensuring coordinated work of muscles:
- chewable;
- maxillohyoid;
- suprahyoid;
- palatal-curtain;
- eardrum.
Recovery and treatment
In the first case, self-recovery takes approximately 1 month; the help of doctors is not needed, since there is no anatomical damage. Symptoms of the second appear after a while - usually 6-8 weeks, so recovery can be painful and incomplete: it will take more than 2 months. In the third stage of damage to the mandibular nerve, treatment gives results only at the beginning and is performed surgically, since we are talking about degeneration with a violation of integrity. Loss of sensitivity, which is observed in a patient for more than 3 months, indicates a high probability of losing it forever. Damage to the mandibular nerve, the consequences of which is the lack of sensitivity of the nerve for a year, leads to irreversible changes. Only the professionalism and responsibility of the doctor, which is guaranteed by the specialists of our Implantmaster clinic, can protect the patient from such unpleasant injuries.
Author:
Neuralgia of the glossopharyngeal nerve
Classical neuralgia of the lingual-trough nerve resembles trigeminal neuralgia in its clinical manifestations (which often causes diagnostic errors), but develops significantly less frequently than the latter (0.5 per 100,000 population).
SYMPTOMS
The disease occurs in the form of painful paroxysms, starting in the area of the root of the tongue or tonsil and spreading to the velum, pharynx, and ear. The pain sometimes radiates to the angle of the lower jaw, eyes, and neck. Attacks, as a rule, are short-term (1-3 minutes), provoked by movements of the tongue, especially during loud conversation, eating hot or cold food, irritation of the root of the tongue or tonsil (trigger zones). The pain is always one-sided. During an attack, patients complain of dry throat, and after the attack, hypersalivation appears. The amount of saliva on the painful side is always reduced, even during the period of salivation (compared to the healthy side). Saliva on the side of pain is more viscous, its specific gravity increases due to an increase in mucus content. In some cases, during an attack, patients develop presyncope or syncope (short-term lightheadedness, dizziness, drop in blood pressure, loss of consciousness).
DIAGNOSTICS
An objective examination of patients with neuralgia of the glossopharyngeal nerve usually does not reveal any changes. Only in a small part of cases are pain observed on palpation of the area of the angle of the lower jaw and certain areas of the external auditory canal (mainly during an attack), a decrease in the pharyngeal reflex, decreased mobility of the soft palate, perversion of taste sensitivity in the posterior third of the tongue (all taste irritations are perceived as bitter) . The disease, like trigeminal neuralgia, occurs with exacerbations and remissions. After several attacks, remissions of varying durations are noted, sometimes up to 1 year. However, as a rule, attacks gradually become more frequent, and the intensity of the pain syndrome increases.
CAUSES
Classic neuralgia of the lingual-trough nerve, like trigeminal neuralgia, is most often caused by compression of the nerve by a branch of the vessel in the medulla oblongata. Symptomatic neuralgia of the glossopharyngeal nerve differs from classical neuralgia in the frequent presence of constant aching pain in the interictal period, as well as progressive sensory impairment in the area of innervation of the glossopharyngeal nerve. The most common causes of symptomatic neuralgia of the glossopharyngeal nerve are intracranial tumors, vascular malformations, and space-occupying processes in the area of the styloid process.
TREATMENT
Treatment should be carried out exclusively by a neurologist. Self-medication is unacceptable.